This article highlights the epidemiology and pathophysiology of pheochromocytomas and paragangliomas. The current management of pheochromocytoma and paragangliomas, including utilization and interpretation of biochemical testing, preoperative imaging, and genetic screening are discussed. Furthermore, perioperative surgical management, outcomes, and recommended follow-up are reviewed.
Key points
- •
Pheochromocytomas and paragangliomas (Pheo/PGL) are rare neuroendocrine tumors that are being discovered incidentally at an increasing rate.
- •
At least one-quarter of patients with Pheo/PGL display germline mutations; genetic testing plays an increasingly important role in the evaluation and management of these patients.
- •
Plasma-free metanephrines and urinary fractionated metanephrine levels are highly sensitive in the diagnosis of Pheo/PGL.
- •
Selective or nonselective alpha blocking agents and calcium channel blockers appear to be equally effective in treating the physiologic effects of Pheo/PGL.
- •
Several surgical approaches are used to remove Pheo/PGL, and the choice of approach depends on patient and tumor-related factors, as well as surgeon preference.
Introduction: nature of the problem
The terms paraganglioma (PGL) and pheochromocytoma (Pheo) were first mentioned in 1908 and 1912 respectively when pathologists Henri Alezais, Felix Peyron, and Ludwig Pick noted tumors with a positive chromaffin reaction in extra-adrenal and adrenal chromaffin tissue. However, according to Welborne and colleagues it was not until 1922, when Marcel Labbe and colleagues reported a case of symptomatic paroxysmal hypertension in a patient with a Pheo, that the relationship between the tumor and its symptoms was established.
The first successful resection for Pheo was performed by Cesar Roux in February 1926. The patient, Madam S, was 33 years old and had suffered attacks of vertigo and nausea for 2 years. At laparotomy, she was found to have a 13-cm adrenal Pheo. Charles Mayo performed the second and perhaps better-known resection for Pheo in October 1926. The patient, Mother Joachim, a nun from Canada, suffered from paroxysmal hypertension, weakness, vomiting, and headaches. At the time, it was felt that her hypertension was mediated through the sympathetic nerves and that sympathectomy may provide relief. She underwent an exploratory laparotomy, and a tumor “the size of a lemon” was found behind the tail of her pancreas. Without preoperative pharmacologic blockade, the entire procedure was completed in 64 minutes and the patient recovered well.
By 1934, more than 60 patients had been diagnosed with a Pheo or PGL and by 1940, 20 successful operations had been performed. The operative mortality in these early series was 30% to 45%. These high mortality rates were partly due to a lack of preoperative alpha blockade and modern anesthesia management. Since that time, much has been learned about the management of these rare tumors. Herein we discuss the incidence and prevalence of Pheo/PGL; describe the typical clinical presentation and diagnostic evaluation of these tumors; explore the known genetic associations; and summarize the preoperative, intraoperative, and postoperative management strategies.
Introduction: nature of the problem
The terms paraganglioma (PGL) and pheochromocytoma (Pheo) were first mentioned in 1908 and 1912 respectively when pathologists Henri Alezais, Felix Peyron, and Ludwig Pick noted tumors with a positive chromaffin reaction in extra-adrenal and adrenal chromaffin tissue. However, according to Welborne and colleagues it was not until 1922, when Marcel Labbe and colleagues reported a case of symptomatic paroxysmal hypertension in a patient with a Pheo, that the relationship between the tumor and its symptoms was established.
The first successful resection for Pheo was performed by Cesar Roux in February 1926. The patient, Madam S, was 33 years old and had suffered attacks of vertigo and nausea for 2 years. At laparotomy, she was found to have a 13-cm adrenal Pheo. Charles Mayo performed the second and perhaps better-known resection for Pheo in October 1926. The patient, Mother Joachim, a nun from Canada, suffered from paroxysmal hypertension, weakness, vomiting, and headaches. At the time, it was felt that her hypertension was mediated through the sympathetic nerves and that sympathectomy may provide relief. She underwent an exploratory laparotomy, and a tumor “the size of a lemon” was found behind the tail of her pancreas. Without preoperative pharmacologic blockade, the entire procedure was completed in 64 minutes and the patient recovered well.
By 1934, more than 60 patients had been diagnosed with a Pheo or PGL and by 1940, 20 successful operations had been performed. The operative mortality in these early series was 30% to 45%. These high mortality rates were partly due to a lack of preoperative alpha blockade and modern anesthesia management. Since that time, much has been learned about the management of these rare tumors. Herein we discuss the incidence and prevalence of Pheo/PGL; describe the typical clinical presentation and diagnostic evaluation of these tumors; explore the known genetic associations; and summarize the preoperative, intraoperative, and postoperative management strategies.
Epidemiology
The annual incidence of Pheo and PGL is between 2 and 8 per million and the prevalence in the population is 1:6500 to 1:2500, respectively. Pheo/PGLs are thought to occur in 0.05% to 0.1% of patients with sustained hypertension. However, this accounts for only 50% of people with Pheo/PGL because approximately half of patients will have paroxysmal hypertension or normotension. Pheochromocytomas comprise 4% to 8% of all adrenal incidentalomas. The peak age of occurrence is in the third to fifth decade of life. Today, 10% to 49% of Pheo/PGLs are found incidentally during imaging studies obtained for other reasons.
In 1951, John Graham analyzed the records of 207 Pheo/PGLs and concluded that Pheo/PGLs follow the “rule of 10s,” with 10% occurring in extra-adrenal tissues, 10% bilateral, and 10% malignant. Later, the teaching that 10% of these tumors were familial was added to this rule. Although this teaching persists in many textbooks and medical school lectures, studies have shown that the “rule of 10” no longer applies. Approximately 15% to 25% of Pheo/PGLs originate in extra-adrenal chromaffin tissue, 8% of sporadic and 20% to 75% of hereditary Pheo/PGL are bilateral at presentation, 5% of adrenal-based and 33% extra-adrenal tumors are malignant, and at least 24% of sporadic Pheo/PGLs have a genetic basis. Today, bilaterality, extra-adrenal location, and prevalence of malignancy depend directly on the underlying genetic mutation.
Pathophysiology
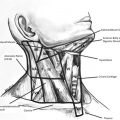
Pheo/PGLs are neuroendocrine tumors that arise from paraganglia cells derived from the neural crest and are distributed along the paravertebral and para-aortic axis from the base of the skull to the pelvic floor. Adrenal-based Pheos arise in the sympathetic adrenal chromaffin cells. Extra-adrenal sympathetic PGLs most commonly occur around the inferior mesenteric artery or at the aortic bifurcation in the organ of Zuckerkandl, but can occur in any chromaffin tissue in the thorax, abdomen, and pelvis. Almost all adrenal-based Pheos and extra-adrenal sympathetic PGLs produce, store, metabolize, and secrete catecholamines or their metabolites. Extra-adrenal parasympathetic PGLs are most commonly found in the head and neck region and are usually not associated with catecholamine secretion. In this article, head and neck PGLs are not discussed.
The uncontrolled release of catecholamines by Pheo/PGLs leads to several physiologic changes and end-organ effects. Prolonged and repeated norepinephrine release has been associated with long periods of vasoconstriction and contraction of the venous pool, and thus decreased circulating blood volume. The decrease in blood volume can lead to acute hypovolemia on cessation of norepinephrine-induced vasoconstriction when the Pheo/PGL is surgically removed. Tumors that secrete predominantly epinephrine have been associated with tachycardia and tachyarrhythmias in addition to arterial hypertension. Elevated plasma catecholamine levels can result in increased glycogenolysis and inhibition of insulin release by islet cells, resulting in signs and symptoms of diabetes mellitus. Additionally, elevated catecholamines can lead to stress-induced cardiomyopathy (Takotsubo cardiomyopathy) with severe left ventricular dysfunction. Pheochromocytoma crisis is the name given to a constellation of symptoms that can result from uncontrolled release of catecholamines and consists of multisystem organ failure, high fever, encephalopathy, and severe hypertension and/or hypotension. Although rarely seen today, these symptoms can progress to severe metabolic acidosis and death if not recognized and treated.
Clinical presentation and diagnosis
Clinical Presentation
The main signs and symptoms of excess circulating catecholamines from Pheo/PGL are headache, palpitations, sweating, pallor, nausea, constipation, flushing, weight loss, fatigue, anxiety, sustained or paroxysmal hypertension, orthostatic hypotension, fever, and hyperglycemia. According to the degree of catecholamine excess, patients may present with myocardial infarction, arrhythmia, or stroke. Because similar signs and symptoms are produced by numerous other clinical conditions ( Table 1 ), Pheo/PGL is often referred to as the “great mimic.” In our experience, patients are often diagnosed with an incidental “asymptomatic” adrenal mass and when a focused history is obtained, the classic symptoms of Pheo/PGL are often elicited in retrospect.
| Organ System | Possible Diagnosis |
|---|---|
| Endocrine | Hyperthyroidism, carcinoid syndrome, hypoglycemia, medullary thyroid carcinoma, mastocytosis, menopause |
| Cardiovascular | Congestive heart failure, arrhythmias, ischemic heart disease, baroreflex failure |
| Neurologic | Migraine, stroke, meningioma, postural orthostatic tachycardia |
| Miscellaneous | Porphyria, panic disorder, factitious disorders, monoamine oxidase inhibitor use, clonidine withdrawal, cocaine abuse |
Biochemical Evaluation
Traditional biochemical tests include measurements of urinary and plasma catecholamines, urinary fractionated and plasma-free metanephrines, and urinary vanillylmandelic acid (VMA). When a patient is suspected to have a Pheo/PGL, the recommended initial test is plasma-free metanephrines or 24-hour urinary fractionated metanephrines. Norepinephrine and epinephrine are metabolized within the tumor by catechol- O -methyltransferase to normetanephrine and metanephrine, respectively. The lack of this enzyme in sympathetic nerves means that the O-methylated metabolites are relatively specific markers of chromaffin tumors. These metabolites are produced continuously in the tumor independent of physiologic catecholamine release and therefore have been shown to be both more sensitive and specific diagnostic biomarkers of Pheo/PGL than their parent catecholamine. There is no consensus that one test is superior. The investigators prefer to start by measuring plasma-free metanephrines because of their high sensitivity and patient convenience. Blood sampling should be performed with the patient in the supine position 15 to 20 minutes after intravenous (IV) catheter insertion. Eight to 12 hours before testing, food, caffeinated beverages, strenuous exercise, and/or smoking should be avoided, to reduce false-positive results from secondary catecholamine release. Providers interpreting tests results should be aware that sympathomimetic agents such as labetalol, sotalol, acetaminophen, buspirone, mesalamine, sulfasalazine, methyldopa, and antidepressants can interfere with the biochemical assays. In a multicenter cohort study of 858 patients, Lenders and colleagues found that the use of multiple initial diagnostic tests increases sensitivity at the cost of decreased specificity. A single plasma or urine metanephrine level remains superior to that of a combination of biochemical tests for initial diagnostic workup.
Studies have shown that in comparison with plasma-free metanephrines or urinary fractionated metanephrines, urinary VMA has a lower sensitivity (68%) and therefore it is not used routinely in our practice. Plasma or urinary dopamine and its metabolite (methoxytyramine) may also be elevated in patients with Pheo/PGL. Although they are not used for diagnostic purposes, their elevation has been associated with SDHB and SDHD mutations and therefore may help guide management.
A suggested algorithm for the biochemical evaluation of Pheo/PGL is depicted in Fig. 1 . If urine and/or plasma metabolites are normal, the diagnosis of Pheo/PGL can be excluded due to the high sensitivity of these tests. If urine and/or plasma metabolite levels are >4 times above the upper limit of normal for any given laboratory, the diagnosis of Pheo/PGL is highly probable. Patients with slight or moderate elevation (>1 time or less than 3 times above the normal limit) of both or either metabolite should undergo repeat testing once potential causes of false-positive results are removed or addressed. Finally, if repeat testing results in elevation of metabolites, a clonidine suppression test can be considered to confirm the diagnosis. This test is useful in distinguishing between high levels of plasma norepinephrine caused by release from sympathetic nerves and those from Pheo/PGL. It is considered diagnostic if norepinephrine levels remain elevated 3 hours after administration of 0.3 mg of oral clonidine. It is important to note that this test is not useful for tumors that intermittently secrete catecholamines or in patients who have marginally elevated norepinephrine levels. Additionally, diuretics and tricyclic antidepressants can cause false-positive values. When the diagnosis of Pheo/PGL is suspected but not confirmed (lack of >4 times elevation of metabolites) and there is a mass on imaging, our group prefers to forgo the clonidine test and proceed directly to resection, particularly when such patients have indications for surgical intervention, such as a large size and atypical imaging characteristics.
When possible, biochemical testing should always precede imaging, as it is the most cost-effective approach to the diagnosis of Pheo/PGL and if biochemical testing proves negative, the patient is not subject to unnecessary radiation. However, in clinical practice, many patients with Pheo/PGL present with an incidentally discovered mass and are in need of biochemical evaluation after imaging is already complete.
Imaging
The 2 most commonly used imaging modalities in the initial evaluation of Pheo/PGL are computerized tomography scan (CT) with and without IV contrast (adrenal protocol for adrenal lesions) and MRI. Functional imaging, including 123 I-metaiodobenzylguanidine (MIBG), 111-In-Pentetreotide (octreotide scan), and PET combined with CT (PET/CT) using fluorodeoxyglucose (FDG) and other radiolabeled agents are also used for the localization of Pheo/PGL.
Computed tomography
CT provides an excellent initial method for the localization of Pheo/PGL because of its outstanding spatial resolution for the thorax, abdomen, and pelvis. To obtain the best results, CT scans should be performed with and without IV contrast. CT scans are highly sensitive (88%–100%) but lack specificity. Pheo/PGL may appear homogeneous or heterogenous, can be necrotic with some calcifications, and may appear solid or cystic ( Fig. 2 A ). Pheo/PGLs demonstrate avid contrast enhancement due to their rich capillary network, and most exhibit mean attenuations of more than 10 Hounsfield units on unenhanced CT. Some studies suggest that the sensitivity of CT for extra-adrenal or bilateral tumors can be low, and therefore the use of MRI or other functional studies is advised in these populations. However, in our practice, CT scan is often the only imaging study necessary to localize lesions and plan for resection of a Pheo/PGL.
MRI
This imaging technique has the same sensitivity and specificity as CT scan in detecting adrenal-based Pheos but has shown superior sensitivity (near 100%) in detecting PGLs and familial adrenal pheochromocytomas. Pheo/PGLs show enhancement on T2-weighted imaging and may appear heterogenous due to internal hemorrhage and cystic components ( Fig. 2 B, C). MRI is useful in patients with inability to tolerate IV contrast, those with intracorporeal metal or surgical clips, and in patients in whom radiation exposure should be limited; that is, children, pregnant women, patients with germline mutations, or in patients with previous excessive radiation exposure.
Functional imaging
There is debate over the role of functional imaging in the preoperative evaluation of Pheo/PGL. Some groups recommend functional imaging for all Pheo/PGLs except for metanephrine producing a small adrenal-based Pheo (PGLs do not produce epinephrine). Others recommend selective use of functional imaging for patients with a high risk of recurrent, multifocal, or malignant disease and for patients with occult lesions on CT or MRI. The field of functional imaging is expanding and some techniques are available only under clinical trials at selected centers.
Metaiodobenzylguanidine with single-photon emission computed tomography
Metaiodobenzylguanidine with single-photon emission CT (MIBG-SPECT) is a guanethidine analog resembling norepinephrine that is taken up and concentrated in sympatho-adrenergic tissue. SPECT data can be fused with CT images to improve spatial resolution and provide anatomic correlation ( Fig. 3 ). The 123 I-MIBG is used preferentially over 131 I-MIBG because of its higher sensitivity, shorter half-life, lack of beta emission, lower radiation dose, and better image quality. The 131 I-MIBG can be used to treat MIBG avid metastasis. MIBG displays improved specificity (95%–100%) when compared with CT or MRI. MIBG can be used to identify sites of primary disease, evaluate metastases, and confirm the biochemical diagnosis. However, 123 I-MIBG-SPECT has lower sensitivity (80%–100%, 88%–100%, respectively) when compared with MRI and CT. Some studies show that the sensitivity of MIBG scans is further reduced in familial PGL syndromes, malignant disease, and extra-adrenal Pheo/PGLs ( Fig. 4 ). Furthermore, up to 50% of normal adrenal glands demonstrate physiologic uptake of 123 I-MIBG and thus false-positive results for adrenal-based lesions are a problem.
Octreotide scan
The radiolabeled octreotide binds to somatostatin receptors in tumors; however, the extent of the binding is variable and dependent on the presence of such receptors in the Pheo/PGL.
The 123 I-MIBG is more sensitive than octreotide for the site of primary disease; however, octreotide has high sensitivity for metastatic disease and can be positive in tumors that have no MIBG uptake. Therefore, octreotide scans may be useful if MIBG scan is negative and/or metastatic disease is suspected.
PET/computed tomography scan
Depending on the radioactive tracer used, the use of PET/CT scans in Pheo/PGL can have superior sensitivity and specificity when compared with 123 I-MIBG and octreotide scans.
However, because of its limited availability and sometimes high cost, it is not commonly used in the evaluation of Pheo/PGL. There are multiple agents used in PET scanning for Pheo/PGL and include 18F-FDG, 18F-fluorodopamine (18F-FDA), 18-F-fluorodihydroxy-phenylalanine (18F-FDOPA) and 68-gallium 1,4,7,10-teraazacyclododecane-1,4,5,10-teraacetic acid-octreotate (68-Ga-DOTATATE). The currently known strengths and weaknesses of these imaging agents and the aforementioned imaging modalities are summarized in Table 2 .
| Strengths | Weakness | |
|---|---|---|
| CT with and without IV contrast |
|
|
| MRI |
|
|
| 123 I-MIBG-SPECT with or without CT |
|
|
| Octreotide scan |
|
|
| 18 F-FDG PET/CT |
|
|
| 18 F-FDA PET/CT |
|
|
| 18 F-FDOPA PET/CT |
|
|
| 68 Ga-DOTATATE PET/CT |
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree