The clinical circumstances in which catecholamines and metanephrines are measured must be assessed in each case. Catecholamine secretion may be appropriately increased in stress or illness (e.g. stroke, myocardial infarction, congestive cardiac failure, obstructive sleep apnoea, head injury).
Imaging
If the biochemical results are abnormal, imaging with computed tomography (CT) or magnetic resonance imaging (MRI) of the abdomen and pelvis is required to locate the tumour. Either test detects almost all sporadic tumours as most are 3 cm or larger. Around 90% of tumours will be visualized in the abdomen. If the tumour is not localized in the adrenals, whole-body imaging should be performed.
Both CT and MRI are sensitive (98–100%) but are only about 70% specific.
Computed tomography
Radiological features of the phaeochromocytomas on CT (Fig. 8.1a) include:
Figure 8.1 (a) Computed tomography scan showing a left-sided phaeochromocytoma. (b) Radio-iodine-labelled MIBG scans in the same patient: anterior and posterior views 4 hours and 24 hours after injection. There is reduced uptake in the middle of the tumour due to necrosis.
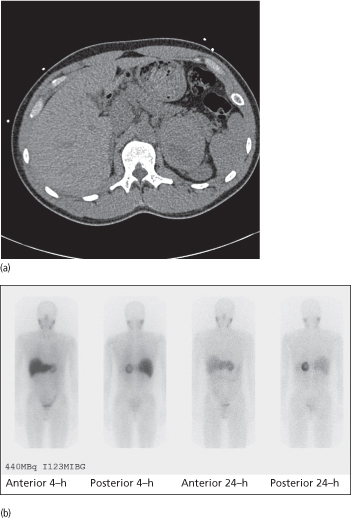
- size > 3 cm
- irregular/heterogeneous
- high (> 20) Hounsfield unit (unit of X-ray attenuation) reading as they contain less fat.
There is a risk of exacerbation of hypertension if an intravenous contrast agent is given (which can be prevented by pre-treatment with alpha-adrenergic blockade).
Magnetic resonance imaging
Phaeochromocytomas appear hyperintense (compared with the liver) on T2-weighted imaging. With MRI, there is neither radiation nor dye. However, it is more expensive than CT.
MIBG scintigraphy
123Iodine-metaiodobenzylguanidine (MIBG) is a compound resembling noradrenaline that is taken up by adrenergic tissue (Fig. 8.1b). An MIBG scan can detect tumours not detected by CT or MRI, or multiple tumours when CT or MRI is positive. MIBG scintigraphy is indicated in patients with large (> 10 cm) adrenal phaeochromocytomas (increased risk of malignancy) or paragangliomas (increased risk of multiple tumours and malignancy).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree