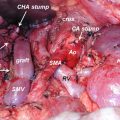
Fig. 9.1
FDG PET/CT imaging of a patient with pancreatic adenocarcinoma. Primary tumor is located at uncinate process of the pancreas. Whole body projection image and PET/CT tomography reveal metastasis at para-aortic and supraclavicular lymph nodes (arrows). Metastasis in supraclavicular lymph nodes was not detected by other conventional imaging modalities. The numbers along the arrows represent SUVmax of each lesion
In a retrospective study with 14 patients with metastasis, the sensitivity of detecting metastatic disease for PET/CT, standard CT, and the combination of the two were 61%, 57%, and 87%, respectively [4]. In seven patients occult metastatic disease was found on PET/CT scan alone. Two patients had metastasis in a supraclavicular lymph node. Two patients had occult liver metastases. Two patients had a peritoneal implant and one had a periesophageal lymph node. These seven patients (11%) with invasive cancer had a change in their management.
According to National Comprehensive Cancer Network (NCCN) guideline 2016, PET/CT can be considered as an adjunct to a formal pancreatic CT protocol in high-risk patients including borderline resectable disease, markedly elevated CA 19-9, large primary tumors, large regional lymph nodes, and patients who are very symptomatic [8].
There are limited data on the use of FDG PET to assess early tumor response after treatment in pancreatic cancer. In a study with small number of patients, FDG PET scans helped monitoring clinical outcome of complete surgical resection as early as one cycle after neoadjuvant treatment in patients with locally advanced pancreatic cancer. Among patients who were PET responders (≥50% decrease in SUVmax), 100% (2/2) had complete surgical resection. Only 6% (1/16) had surgical resection in the PET nonresponders (<50% decrease) [1]. Further studies with larger population of patients are needed to confirm the role of FDG PET in identifying patients who could undergo complete surgical resection after the neoadjuvant treatment.
There are several studies that FDG PET can predict prognosis of patients with pancreatic cancer. Generally speaking, the higher the FDG uptake, the poorer the survival outcome. In a retrospective study analyzing 118 patients with pancreatic cancer who had performed FDG PET before receiving palliative chemotherapy, patients with high metabolism showed shorter survival than patients with low metabolism (SUVmax <4.5, 11.1 months; HR 1 vs SUVmax ≥ 4.5, 7.8 months; p = 0.004) [2].
Since SUVmax represents only one value of single pixel in ROI, it is vulnerable to noise. Thus, values representing tumor burden in whole body were developed. Metabolic tumor volume (MTV) is a sum of each tumor volume above certain FDG uptakes. Generally, all voxels with an SUV of 2.5 or greater within the isocontour line were counted for the calculation of MTV. Total lesion glycolysis (TLG) reflects FDG activities from all tumors in the body. TLG is calculated as MTV multiplied by the SUVmean. In a retrospective study, 51 patients with resectable pancreatic cancer underwent FDG PET/CT and curative operation [5]. SUVmax, MTV, and TLG were compared as prognostic factors. Multivariate analysis revealed that MTV and TLG were independent prognostic factors for recurrence-free survival (RFS) and overall survival (OS). SUVmax was an independent prognostic factor for OS, but not for RFS.
9.1.2 Intraductal Papillary Mucinous Neoplasms
Intraductal papillary mucinous neoplasms (IPMN) are cystic tumors of the pancreas. IPNMs are important because if they are left untreated some of them may progress to invasive cancer. However, up to 85% of patients treated surgically according to the international consensus guidelines (ICG) subsequently reveal no malignancy. Thus, it could be said that the resection of these IPMNs was unnecessary. In a report analyzing 162 patients with IPMN, the sensitivity of the ICG in detecting malignancy was 93.2%, but their specificity was only 22.2%. Therefore, more accurate diagnostic methods differentiating between benign and malignant IPMNs are needed.
The sensitivity and specificity of multi-detector CT were 32–53% and 77–95%, respectively [6]. Those of magnetic resonance cholangiopancreatography were 37–59% and 71–91%. Those of endoscopic ultrasound-guided aspiration were 55–60% and 74–93%. In a study analyzing 69 histologically confirmed patients, the sensitivity and specificity of FDG PET were 83.3% and 100%, respectively [9]. The cutoff value was set as SUVmax of 2.5 or more. FDG PET is more accurate than any other procedures in differentiating benign and malignant lesions in patients already diagnosed as IPMN (Fig. 9.2). On the other hand, ICG is useful for predicting the incidence of malignant transformation and the consequent need for resection in low-risk patients with a long life expectancy.
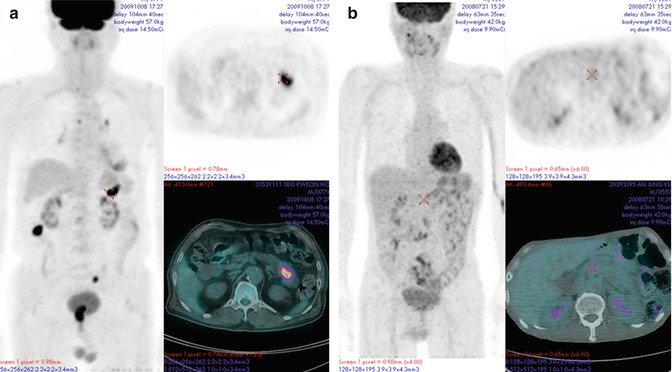
Fig. 9.2
FDG PET/CT images in patients with intraductal papillary mucinous neoplasm. While a malignant lesion (a) shows high FDG uptake in the tumor, a benign lesion (b) cannot be distinguished from background of the normal pancreas
9.1.3 Neuroendocrine Tumor
Neuroendocrine tumor (NET) is a heterogeneous group of malignant tumors that originate from the neuroendocrine system. For diagnosis of NETs, conventional radiological imaging methods such as CT, MRI, and ultrasonography (US) have been used. However, these anatomical imaging methods have a limitation in diagnostic value when the lesions are small and located at unexpected sites. By the use of these conventional imaging, endocrine pancreatic tumors can be localized in approximately 50% of the cases. Patients with metastatic NET had improved survival after the removal of the primary tumor, even in the presence of liver metastasis. Locating the primary tumor is important to the surgeon. Thus, functional nuclear imaging covering the whole body has been applied to diagnose NETs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree