Highlights
- •
Discontinuing pelvic drain (PD) placement after RARP did not increase the risk of overall or high-grade complications.
- •
Patients without PD required fewer opioids, indicating better postoperative pain management.
- •
PD omission resulted in substantial CO2e reductions, from 220 kg in 2016 to 2,180 kg in 2022.
- •
Annual cost savings from discontinuing PD placement increased from €1,855 in 2016 to €18,506 in 2022.
- •
Avoiding unnecessary PD placement reduced pain, healthcare costs, and environmental impact, while maintaining patient safety and outcomes.
Abstract
Purpose
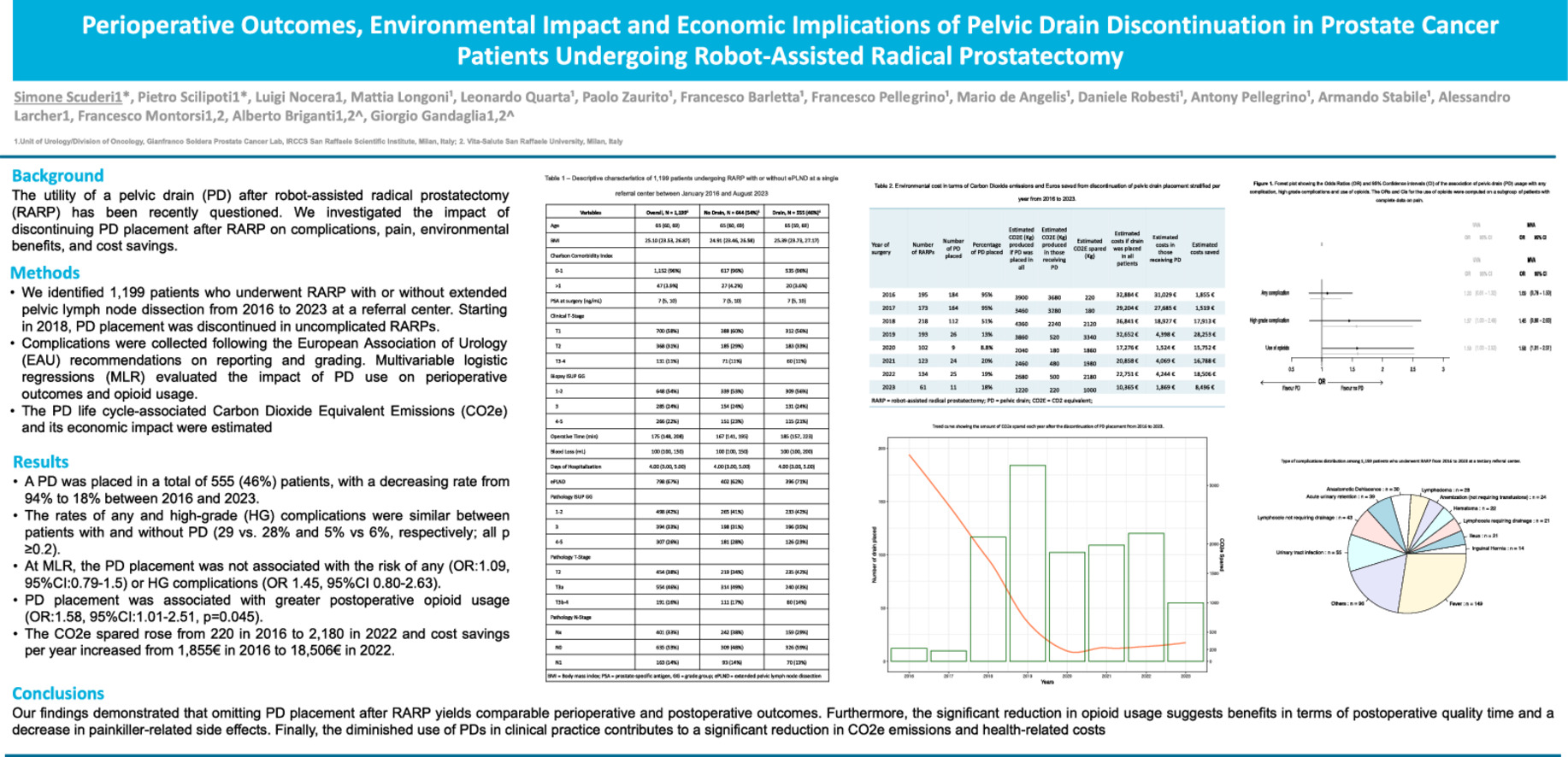
The utility of a pelvic drain (PD) after robot-assisted radical prostatectomy (RARP) has been recently questioned. We investigated the impact of discontinuing PD placement after RARP on complications, pain, environmental benefits, and cost savings.
Methods
We identified 1,199 patients who underwent RARP with or without extended pelvic lymph node dissection from 2016 to 2023 at a referral center. Starting in 2018, PD placement was discontinued in uncomplicated RARPs. Complications were collected following the European Association of Urology (EAU) recommendations on reporting and grading. Multivariable logistic regression models (MLR) evaluated the impact of PD use on perioperative outcomes and opioid usage. The PD life cycle-associated Carbon Dioxide Equivalent Emissions (CO2e) and its economic impact were estimated.
Results
A PD was placed in a total of 555 (46%) patients, with a decreasing rate from 94% to 18% between 2016 and 2023. The rates of any and high-grade (HG) complications were similar between patients with and without PD (29 vs. 28% and 5% vs. 6%, respectively; all P ≥ 0.2). At MLR, the PD placement was not associated with the risk of any (OR:1.09, 95%CI:0.79–1.5) or HG complications (OR 1.45, 95%CI 0.80–2.63). PD placement was associated with greater postoperative opioid usage (OR:1.58, 95%CI:1.01–2.51, P = 0.045). The CO2e spared rose from 220 in 2016 to 2,180 in 2022 and cost savings per year increased from 1,855€ in 2016 to 18,506€ in 2022.
Conclusion
Unnecessary PD placement should be avoided in uncomplicated RARPs to obtain environmental benefits, reduce health-related costs, and improve patients’ outcomes.
Graphical Abstract
1
Introduction
Pelvic drain (PD) placement has been a standard procedure in open radical prostatectomy, yet its necessity in robot-assisted radical prostatectomy (RARP) is increasingly questioned. Studies on RARP cohorts have shown that PD placement does not significantly impact complication rates or postoperative outcomes and may therefore be omitted [ ]. Despite this evidence, many surgeons remain reluctant to alter their practice, adhering to the traditional belief in PD placement [ ]. Previous studies supporting the safety of omitting a drain after RARP did not comprehensively report postoperative outcomes using standardized methodologies for complication assessment [ ]. Moreover, they failed to evaluate the carbon footprint of avoiding drain placement, measured in Carbon Dioxide Equivalent (CO2e) emissions, and the potential economic impact on healthcare systems. This aspect is crucial, as operating theatres are significant contributors to annual carbon emissions and each surgical unit emits between 3 to over 5 million CO2e annually [ ]. Notably, PDs, constructed from manufactured silicone, contribute significantly to CO2e emissions [ ].
Under this light, we aimed to assess the complication rates of patients after the discontinuation of the PD placement after RARP at our center using a standardized collection system for postoperative outcomes. Additionally, we sought to assess the benefits in terms of patient outcomes, environmental advantages in terms of spared CO2e emissions, and cost savings associated with avoiding unnecessary pelvic drain placement during uncomplicated RARP procedures.
2
Materials and methods
2.1
Study population
After institutional review board approval, we relied on a prospectively maintained database including 11,038 consecutive patients who underwent radical prostatectomy at our center from 1998 to 2023. For the study purpose, we selected patients diagnosed with localized prostate cancer (PCa) who underwent RARP with or without extended pelvic lymph node dissection (ePLND) from January 1st, 2016, to August 31st, 2023 (n=1,317). Patients with missing data on postoperative complications were excluded (n=118).
2.2
Surgical procedure
All the RARPs were performed using a Da Vinci Xi surgical system (Intuitive Surgical, Sunnyvale, CA, USA) in a fourth arm configuration with a transperitoneal approach [ ]. ePLND was performed when the risk of lymph node infiltration calculated using validated nomograms was higher than the proposed cut-offs [ ]. Anatomically defined ePLND involved the removal of the obturator, internal iliac, and external iliac lymph nodes. All procedures were conducted by 5 urologists with extensive robotic experience, each having performed a minimum of 50 RARPs in total at the time of study initiation. Due to the mounting evidence of equivalence of placing a drain vs. no drain RARPs and the low incidence of urinary leaks, blood and/or lymphorrhagia from the drain placed during the procedure, which was typically removed in postoperative day 1, since 2018 we discontinued the systematic PD placement after uncomplicated procedures (defined as any procedure with Intraoperative Adverse Incident Classification (EAUiaiC) 0–1) [ ]. All PDs placed were tubular with a 21 Fr diameter. All specimens were submitted for pathologic evaluation in multiple packages and were evaluated by dedicated uropathologists at each center.
2.3
Covariates and outcomes
2.3.1
Covariates
Preoperative, intraoperative, and postoperative data were collected [ ]. Pre-operative data were age at surgery, body mass index (BMI), Charlson comorbidity index (CCI), PSA value, clinical TNM-stage, and biopsy Gleason Grade Group (GGG). Intraoperative data included blood loss (mL), operative time (minutes), intraoperative complications, and PD placement. Postoperative data included pathological GGG, pathological TNM-stage, days of hospitalization, postoperative pain according to visual analog scale (VAS), painkillers administration, and complications within 90 days.
2.3.2
Outcomes
The study outcomes were the rate of any complications and HG complications within 90 days after RARP, the administration of post-operative opioids due to persisting pain after non-steroidal anti-inflammatory drugs (NSAID) usage, the estimated CO2 equivalent spared, and the costs (in euros) saved due to the discontinuation of the PD placement.
2.3.2.1
Complications
Since September 2016, a prospective collection system of perioperative outcomes has been implemented at our center, according to the European Association of Urology (EAU) guidelines for collecting and reporting postoperative complications [ ]. Complications were graded according to the Clavien-Dindo (CD) classification. We defined complications as any complication occurring within 90 days of the surgery. High-grade (HG) complications were defined as CD >2. Postoperative complications were collected after patient discharge through an interview done by medical doctors within 90 days after surgery. The quality criteria for accurate and comprehensive reporting of surgical outcomes recommended by the EAU guidelines on reporting and grading of complications were fulfilled [ , ].
Acute post-operative pain was detected using the VAS, a validated, subjective measure for acute and chronic pain. The VAS was administered to the patient during the postoperative days 0, 1, and 2. Moreover, we collected data on post-operative Paracetamol, NSAIDs, and opioid use. The protocol in our center consisted of intravenous (IV) administration of Paracetamol 1000 mg every 6–8 hours the day after the surgical procedure. NSAIDs (Ketorolac 30 mg IV every 8 hours) were administered IV postoperatively when the pain was not controlled by Paracetamol alone. Opioids (Tramadol 100 mg/ml IV every 8 hours) were given to the patient when the pain was persisting after the NSAID administration. We used opioid administration as a surrogate of pain rather than the VAS since the latter relies on the patient’s subjective interpretation of their pain level, which can vary based on individual perception and interpretation.
2.3.2.2
Estimation of the carbon footprint of PD placement
We assessed the carbon footprint of PD production by considering the CO2e emissions associated with different phases of the production process. We assumed the weight of a single PD to be 0.3 kg. We considered 11 kg of CO2e produced per kilogram of silicon, in line with prior studies [ ]. Waste management was estimated to produce 1 kg of CO2e per kilogram of silicon [ ]. The estimated surgical operation footprint was 2.8 kg CO2e per minute of surgery (using 5 minutes as a median operating time for placement) [ ]. Transportation CO2e included the emissions from an urban truck delivery, covering an average distance of 500 kilometers, and transporting an average of 100 PDs [ ]. The final emission estimation amounted to 1.5 kg CO2e per PD.
2.3.2.3
Estimation of the economic impact of PD placement
We estimated the economic impact of the PD placement by calculating the 2023 cost of the single PD (1.92€) and needle (8€) adjusted for the constant annual inflation rate (2%) as reported from publicly available sources [ ]. Finally, we estimated the additional operative time required for pelvic drain (PD) placement. To achieve this, we analyzed the time between the completion of the vesicourethral anastomosis and the final skin suture in our last 100 cases. Our findings indicated that placing a PD would increase the operative time by approximately 5 minutes, resulting in an additional operating room cost of €160 per surgery [ , ].
2.3.3
Statistical analysis
Frequencies and proportions were reported for categorical variables, while medians and interquartile ranges (IQRs) for continuous ones. We investigated the differences between patients who placed the PD and those who did not, as well as between men who underwent ePLND and those who received RARP alone. Multivariable logistic regression (MLR) analyses assessed the impact of PD placement after adjusting for preoperative (BMI, year of surgery, comorbidities) and intraoperative variables (surgical time and ePLND). We then investigated the role of PD positioning on post-operative pain, and we performed a MLR to assess the impact of PD placement on the use of postoperative opioids after adjusting for preoperative features (BMI, year of surgery, clinical T-stage) and operative time among patients that had complete data on pain. We further used multivariable linear regression to assess whether the pelvic drain placement was associated with longer operative time, after accounting for BMI, age, clinical T-stage, and lymph node dissection. Finally, we estimated the CO2 equivalent spared the costs saved each year due to the PD placement discontinuation, and we graphically plotted the results using trend curves.
3
Results
3.1
Baseline characteristics
Overall, 1,199 patients with complete pre-operative and intra-operative data represented our final cohort. A total of 555 patients (46%) received a PD after the surgical procedure (46%). The proportions of RARP in which a PD was placed decreased from 94% (n=184) to 18% (n=12) in 2023. The preoperative and intraoperative characteristics of the population are reported in Table 1 . Patients’ characteristics were similar between patients who received PD and those who did not. Patients in which a PD was placed experienced a higher operative time [185 (IQR 157, 223) vs. 167 (IQR 141, 195)] and received more frequent ePLND [396 (71%) vs. 402 (62%)] compared to those without PD. Table 2
| Characteristic | Overall, N = 1,199 1 | No Drain, N = 644 (54%) 1 | Drain, N = 555 (46%) 1 |
|---|---|---|---|
| Age | 65 (60, 69) | 65 (60, 69) | 65 (59, 69) |
| BMI | 25.10 (23.53, 26.87) | 24.91 (23.46, 26.58) | 25.39 (23.73, 27.17) |
| Charlson Comorbidity Index | |||
| 0–1 | 1,152 (96%) | 617 (96%) | 535 (96%) |
| >1 | 47 (3.9%) | 27 (4.2%) | 20 (3.6%) |
| PSA at surgery (ng/mL) | 7 (5, 10) | 7 (5, 10) | 7 (5, 10) |
| Clinical T-Stage | |||
| T1 | 700 (58%) | 388 (60%) | 312 (56%) |
| T2 | 368 (31%) | 185 (29%) | 183 (33%) |
| T3-4 | 131 (11%) | 71 (11%) | 60 (11%) |
| Biopsy ISUP GG | |||
| 1–2 | 648 (54%) | 339 (53%) | 309 (56%) |
| 3 | 285 (24%) | 154 (24%) | 131 (24%) |
| 4–5 | 266 (22%) | 151 (23%) | 115 (21%) |
| Operative Time (min) | 175 (148, 208) | 167 (141, 195) | 185 (157, 223) |
| Blood Loss (mL) | 100 (100, 150) | 100 (100, 150) | 100 (100, 200) |
| Days of Hospitalization | 4.00 (3.00, 5.00) | 4.00 (3.00, 5.00) | 4.00 (3.00, 5.00) |
| ePLND | 798 (67%) | 402 (62%) | 396 (71%) |
| Pathology ISUP GG | |||
| 1–2 | 498 (42%) | 265 (41%) | 233 (42%) |
| 3 | 394 (33%) | 198 (31%) | 196 (35%) |
| 4–5 | 307 (26%) | 181 (28%) | 126 (23%) |
| Pathology T-Stage | |||
| T2 | 454 (38%) | 219 (34%) | 235 (42%) |
| T3a | 554 (46%) | 314 (49%) | 240 (43%) |
| T3b-4 | 191 (16%) | 111 (17%) | 80 (14%) |
| Pathology N-Stage | |||
| Nx | 401 (33%) | 242 (38%) | 159 (29%) |
| N0 | 635 (53%) | 309 (48%) | 326 (59%) |
| N1 | 163 (14%) | 93 (14%) | 70 (13%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree