Fig. 8.1
Dissection is performed deep to Buck’s fascia
3.
Control of dorsal venous complex.
4.
Dissection between urethra and corporal bodies without dividing the urethra.
5.
Dissection between the glans and tips of corpora cavernosa.
6.
The glans is attached only on the urethra that is divided (Fig. 8.2).
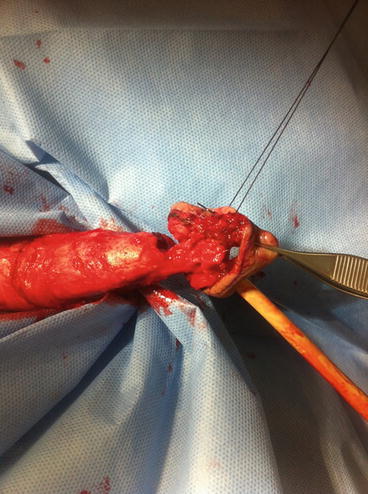
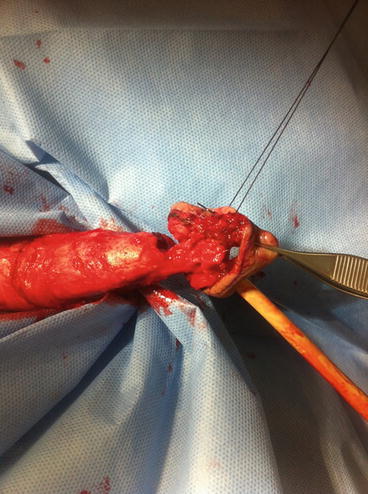
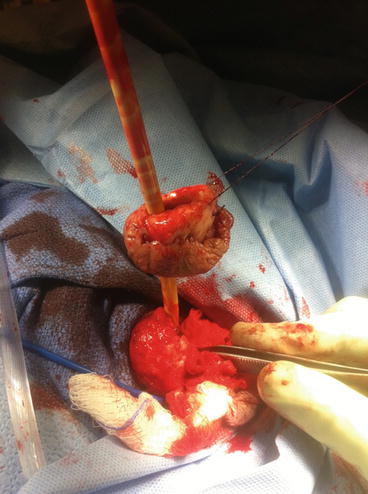
Fig. 8.2
The dorsal venous complex is divided. Glans is hanging on the urethra
8.
Adequate frozen sections are sent from the distal tunica.
9.
Urethra is spatulated.
Methods of covering the exposed tips of corpora cavernosa following glansectomy:
1.
Penile skin advancement: Perhaps, that is the easiest method for covering the exposed corpora. Penile skin is degloved and the penile skin is advanced to be sutured to the edges of the spatulated urethra.
2.
Urethral advancement with spatulation: Following glansectomy, a plane of dissection is developed sharply between the urethra and the 2 corpora. Every attempt is made when doing that dissection not to button hole the urethra which is particularly thin dorsally. The urethra is spatulated and advanced over the tips of the corpora and sutured to the penile skin giving an appearance similar to the lost glans (Figs. 8.4, 8.5, 8.6, and 8.7). Patient undergoing glansectomy should be warned that sometimes their female partners may complain of increased pain during sexual intercourse following that surgery. This is because the cushion effect of the flaccid glans during normal erection is lost.

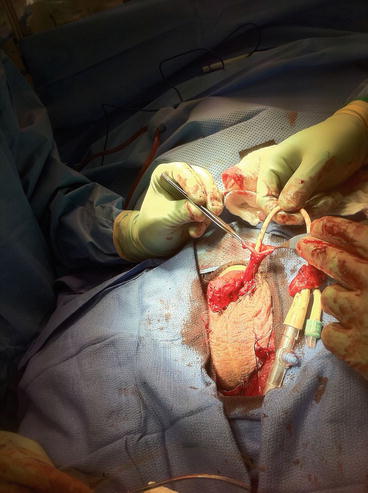



Fig. 8.4
Urethra is mobilized off the corpora cavernosa
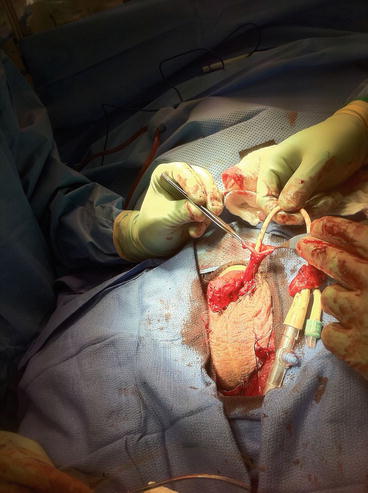
Fig. 8.5
Urethra is spatulated

Fig. 8.6
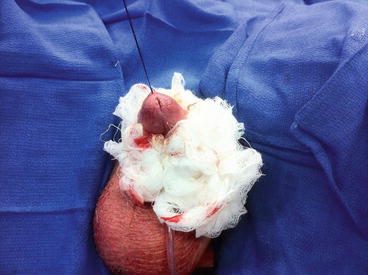
Eversion of the spatulated urethra on the corpora cavernosa

Fig. 8.7
Urethra is sutured to penile skin
3.
Split-thickness skin graft (STSG): The technique of performing an STSG can be easily performed by most urologists. However, if the surgeon is not adequately trained in STSG, plastic surgeon help should be requested. The donor site selected is typically the inner (non-hairy) aspect of the thigh (Figs. 8.8 and 8.9). Experience has shown that the graft should be taken 30 % larger than the recipient site since it tends to contract after transplanting [6]. Following harvesting, the graft is applied with quilting sutures of 3-0 SAS to immobilize it in place (Fig. 8.12). A key to the success of this type of defect coverage is the dressing that should keep the graft stable (together with the quilting sutures). This allows for improved graft take. Split-thickness skin graft can be used to cover defects on the glans penis or shaft (Figs. 8.10, 8.11, and 8.12). We don’t normally use full-thickness skin graft because of poor cosmetic outcome in the penis and poor recipient site intake [7].



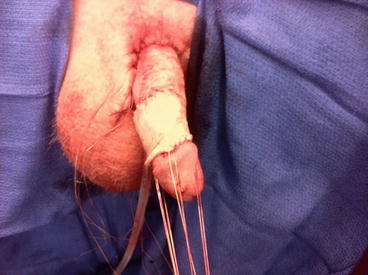

Fig. 8.8
Typical site for donor STSG on the medial aspect of the thigh

Fig. 8.9
Donor site on the thigh after harvesting

Fig. 8.10
Quilting sutures to fix the graft to the exposed tips of the corpora cavernosa
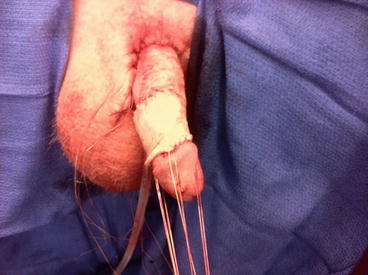
Fig. 8.11
STSG applied on the penile shaft
Oncological and Functional Outcome of Glansectomy
Smith et al. reported their experience with 72 patients treated by glansectomy and STSG for T1/T2 penile cancer. In that report, the mean follow-up was 27 months. The local recurrence rate was 4 % and only two patients required early re-excision due to positive margin in the permanent specimen [8]. The functional outcome was reported to be adequate in terms of voiding and sexual function. However, it may be associated with increased discomfort of the female partner during intercourse due to loss of the cushion effect of the tumescent glans [9].
Partial Penectomy
Partial penectomy is considered the most aggressive form of penis-conserving surgery. It is indicated for tumors on the glans and extending onto the distal shaft or tumors of the distal shaft of the penis. The main goal of that surgery is to eradicate the penile cancer while maintaining adequate remaining penile length sufficient for urinating in a standing position and possibly able to attain sexual intercourse. Usually a penile stump of 2–3 cm is enough to achieve that. If that cannot be achieved at the time of partial penectomy, total penectomy with perineal urethrostomy is advised. Patients undergoing partial penectomy should be counseled about the risks of urethral meatus stenosis (6 %) and urine spraying during micturition that may necessitate sitting down when urinating [10].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree