Parenteral Nutrition Support
1 Cleveland Clinic, Cleveland, OH
2 Brody School of Medicine, East Carolina University, Greenville, NC
Parenteral nutrition (PN) is a complex admixture of amino acids, dextrose, fat emulsions, water, electrolytes, vitamins, minerals, and trace elements. It is provided for patients whose gastrointestinal (GI) tract is not functional, accessible, or safe to use and is infused via peripheral or central veins. The exact route of administration will depend on the length of therapy, nutrition requirements, goal of nutrition therapy, availability of intravenous (IV) access, severity of illness, and fluid status.
Indications for PN
Enteral nutrition (EN) is always preferable over PN due to its expense and potential for serious complications. PN should be used only when enteral feedings are not possible in patients who require nutrition support. The following conditions may warrant the use of PN.
- Paralytic ileus
- Mesenteric ischemia
- Small bowel obstruction
- High output enterocutaneous fistula
- Severe GI bleed
- Lack of enteral access
- GVHD of the gut
- Short bowl symdrome
- Radiation enteritis
According to the 2009 American Society of Parenterl and Enteral Nutrition (ASPEN) guidelines for the provision of Nutrition Support Therapy in the Critically Ill Adult, PN should be initiated 5 to 7 days pre-operatively if a patient is malnourished; PN should not be initiated until 5 to 7 days post-operatively if EN is not feasible; PN should not be initiated unless the anticipated duration is ≥7 days.
Components of PN
Amino Acids
The primary function of amino acids in PN solutions is to maintain or improve nitrogen balance and promote maintenance of lean body mass. Parenteral amino acids are provided in the form of crystalline amino acids and contain a mixture of essential and non-essential amino acids providing 4 calories per gram. The concentration of amino acids in these solutions ranges from 3 to 20 percent. Thus, a 10 percent solution of amino acids supplies 100 g of protein per liter. In general, 15 to 20 percent of the total energy prescription should be supplied as protein; however, this may differ based on tolerance, clinical status and disease state.
Carbohydrates
Carbohydrates are provided as an energy substrate and are supplied as dextrose monohydrate in concentrations ranging from 2.5 to 70 percent. A 10 percent solution yields 100 g of carbohydrate per liter of solution. Dextrose monohydrate used in PN solutions yields 3.4 calories per gram. The use of carbohydrate ensures that protein is not catabolized for energy during conditions of normal metabolism. Higher dextrose concentrations, usually greater than 10 percent, are used when central access is available as thrombophlebitis may occur in a peripheral vein.
Metabolic stress is characterized by insulin resistance, hyperglycemia, and impaired glucose oxidation. When glucose oxidation rates are exceeded, fat synthesis will occur, which may generate excessive CO2. This may contribute to CO2 retention in patients with respiratory disease. In addition, exceeding glucose oxidation rates may also contribute to hepatic steatosis or fat deposition in the liver. Therefore, dextrose infusion should be limited to 7 mg/kg per minute in stable hospitalized patients and greater than 4 mg/kg per minute in the critically ill. Consideration should be given to the dextrose content of other intravenous fluids, which may be infusing simultaneously.
Lipids
Intravenous fat emulsions (IVFE) supply lipids, which are a source of essential fatty acids (EFAs) and a concentrated source of calories. In addition, the use of IVFE may aid in blood glucose control in the hyperglycemic patient.
IVFE are available in 10 and 20 percent concentrations for infusion and 30 percent for compounding. They are composed of aqueous suspensions of soybean or safflower oil, with egg yolk phospholipid as the emulsifier. Patients who are allergic to eggs should not be given IVFE and can be given safflower or sunflower oil topically or enterally. Glycerol is added to make an isotonic solution. A 10 percent emulsion provides 1.1 kcal/mL; a 20 percent emulsion provides 2 kcal/mL; and 30 percent emulsion provides 3 kcal/mL. To prevent EFA deficiency (EFAD), 2 to 4 percent of total calories should be provided from linoleic acid and 0.25 to 0.5 percent of total calories as alpha-linolenic acid.
The high levels of linoleic acid in soy-based lipids produces pro-inflammatory and immunosuppressive effects, particularly at high doses and at faster infusion rates. A maximum dose of 1 g of lipid per kg per day should be infused to avoid hepatic effects such a steatosis, cholestasis, and/or parenteral nutrition related liver disease (PNALD), which can be seen in long-term PN patients. Daily infusion of lipid should therefore be avoided in long-term PN-dependent patients. However, increasing attention is being brought to alternative sources of fat emulsion such as medium-chain triglycerides, olive oil, and fish oils. Lipid emulsions should not be given in hypertriglyceridemia-induced pancreatitis or when serum triglyceride values are greater than 400 mg/dL.
Fluid, Electrolytes, Vitamins, Minerals, and Trace elements
Once the macronutrient portion of the PN prescription has been established, the day-to-day management centers on fluid and electrolytes. Daily fluid requirements can be estimated from the sum of fluid losses including urine, GI and insensible losses, minus the fluid gains, such as other IV fluids and/or oral intake. Weighing the patient daily is the best means of assessing net gain or loss of fluid. Rapid weight gain or loss (more than 4 pounds (1.8 kg) in 1 week) generally represents fluid changes and not tissue synthesis. Vital signs, such as blood pressure and heart rate, and physical examination changes (e.g., edema, ascites, and skin turgor) also offer evidence of fluid status. In general, young adults require 30 to 40 mL/kg per day and older adults require 20 to 30 mL/kg per day.
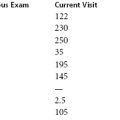
Electrolytes are routinely added to PN solutions in amounts sufficient to provide for daily needs (Table 13-1). Electrolyte requirements will vary depending on the patient’s current electrolyte, renal, and fluid status, as well as their underlying disease process. If the patient has been receiving maintenance IV fluids prior to starting PN, it is helpful to note the electrolyte composition of these fluids and use this as a guide to prescribe the PN formula. Patients receiving PN may have higher intracellular electrolyte requirements than patients receiving standard IV fluids.
Table 13-1 Daily Electrolyte Requirements during Parenteral Nutrition in Adults
Source: National Advisory Group on Standards, and Practice Guidelines for Parenteral Nutrition, ASPEN: Safe practices for parenteral nutrition formulations. J Parenter Enteral Nutr. 2004; 28(suppl):S38–S70.
| Electrolyte | ParenteralEquivalent of RDA | Standard Intake |
|---|---|---|
| Calcium | 10 mEq | 10–15 mEq |
| Phosphate | 30 mmol | 20–40 mmol |
| Magnesium | 10 mEq | 8–20 mEq |
| Sodium | NA | 1–2 mEq/kg + replacement |
| Potassium | NA | 1–2 mEq/kg + replacement |
| Acetate | NA | As needed to maintain acid-base balance |
| Chloride | NA | As needed to maintain acid-base balance |
NA: Not applicable
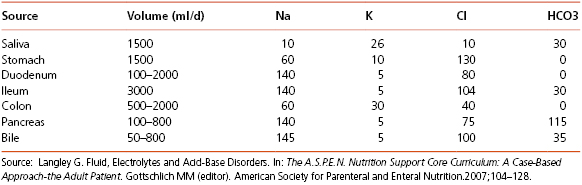
Sodium is a major extracellular cation and functions in the maintenance of osmotic pressure and in acid–base balance. The usual dose is 1 to 2 mEq/kg per day. Requirements may be increased when there are excess losses from urine, ostomies, or fistulas or decreased in renal, cardiac, or hepatic failure. See Table 13-2 for electrolyte content of the GI tract secretions.
Table 13-2 Volume and Average Electrolyte Content of Gastrointestinal Secretions
Potassium is the major cation of intracellular fluid. The normal dose is 1 mEq/kg per day. Hypokalemia may result from diuretics, amphotericin B, nasogastric suction, or vomiting. Other medications such as cyclosporine and tacrolimus may cause hyperkalemia. The PN solution should provide maintenance potassium requirements. Acute deficits of potassium should be corrected outside of the PN with an intravenous (IV) replacement dose.
Sodium and potassium may be added to PN solutions in the form of chloride or acetate salts. Chloride is a major extracellular anion and functions in the maintenance of osmotic pressure and acid–base balance. Acetate maybe added to PN solutions when clinically appropriate since it is converted to bicarbonate in the liver and functions as a systemic alkalinizer. Bicarbonate should never be added to PN solutions since it is not compatible with other additives and may form a precipitate.
Calcium is an extracellular cation that is essential for normal muscle contraction, nerve function, blood coagulation, and bone mineralization. The usual dose is 10 to 15 mEq/day. Sixty percent of serum calcium is bound to protein, primarily albumin. Therefore, in the presence of a low serum albumin level, a low serum calcium level needs to be adjusted for hypoalbuminemia.
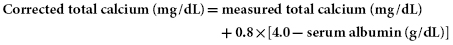
This equation provides an estimate of the adjusted calcium level in the presence of hypoalbuminemia. When in doubt and when the serum albumin is less than 2.8 g/dL, an ionized calcium level should be obtained. Along with calcium, phosphorus is the major component of bone hydroxyapatite and teeth. Phosphorus is the primary intracellular anion and functions in the metabolism of carbohydrate, fat, and protein. The usual dose is 20 to 40 mmol/day. The combination of calcium and phosphorus in PN formulas has the potential of forming a precipitate. Thus, the maximum calcium and phosphorus product should be <200 in a PN formula as per the formula below.
Magnesium functions in enzyme reactions such as glycolysis and in all reactions involving adenosine triphosphate (ATP). Magnesium is often depleted in patients with protein calorie malnutrition and prolonged IV fluid therapy. The usual dose of magnesium sulfate is 8 to 20 mEq/day. Magnesium sulfate provides 8.12 mEq/g of magnesium.
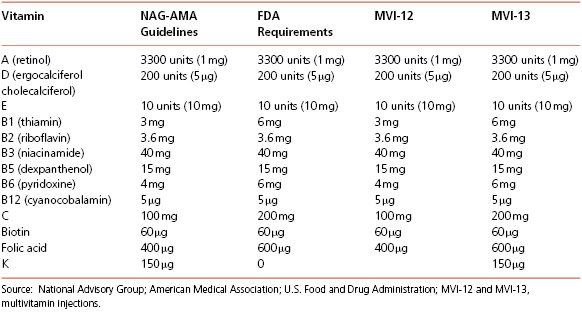
Vitamins, minerals, and trace elements are essential for humans and should be added daily to the PN solution in order to prevent deficiencies. Since they are provided parenterally and therefore bypass the digestive and absorptive process, the amounts are lower than the Dietary Reference Intakes (DRI). Parenteral vitamins and trace elements are given as standard multiple-vitamin and trace element preparations. In the event that vitamin, mineral, or trace element deficiencies or unusual losses occur, they can sometimes be supplemented above the amount normally added to the PN solution. Tables 13-3 and 13-4 show the daily multivitamin and trace element requirements as well as the common commercially available products.
Table 13-3 Daily Trace Element Requirements
Source: A.S.P.E.N. Board of Directors and the Task Force for the revision of safe practices for parenteral nutrition. J Parenter Enteral Nutr. 2004; 28(suppl):S38–S70.
| Trace Element | ASPENRecommendations | GI Losses |
|---|---|---|
| Chromium | 10–15 μg | 20 μg/day |
| Copper | 0.3–0.5 mg | 500 μg/day |
| Manganese | 60–100 μg | |
| Selenium | 20–60 μg | |
| Zinc | 2.5–5.0 mga | Additional zincb |
a Additional 2 mg/day in hypermetabolic states.
b Additional 12 mg/L of small bowel losses and 17 μg/kg of stool or ileostomy losses.
Table 13-4 Adult Parenteral Multivitamins: Guidelines and Products
Nutrition Requirements
Determining nutrient requirements is dependent on age, gender, weight, body composition, activity level, and clinical status. In the clinical setting, this can be determined via indirect calorimetry or equations; in the research setting via direct calorimetry. Direct calorimetry measures the release of heat, however, it is expensive and impractical in the hospital setting. Indirect calorimtery (IC) is considered the gold standard in the intensive care patient where most clinicians use a metabolic cart to estimate the resting metabolic rate (RMR), however it is not often used due to its expense and the need for clinical expertise. Equations for the healthy subject such as the Mifflin–St. Jeor are used to estimate energy expenditure. Those equations that are most often used in the critically ill patient include the Ireton–Jones or the Penn State equations as seen in Table 13-5. ASPEN recommends a range of 20 to 35 calories per kilogram of body weight for adults.
Table 13-5 Predictive Equations
Source: Data from Wooley JA, Frankenfield D. Energy. In: Gottschlich MM (Editor). The A.S.P.E.N. Nutrition Support Core Curriculum: A Case-Based Approach-the Adult Patient. 2007: The American Society for Parenteral and Enteral Nutrition, pp. 19–32.
| Mifflin–St Jeor | Men: Energy expenditure = 5 + 10 (wt in kg) + 6.25 (ht in cm) − 5 (age) Women: Energy expenditure = −161 + 10 (wt in kg) + 6.25 (ht in cm) − 5 (age) |
| Ireton–Jones | Spontaneous breathing IJEE (s) = 629 − 11(A) + 25(W) − 609(O) Ventilator-dependent IJEE (v) = 1784 − 11(A) + 5(W) + 244(S) + 239(T) + 804(B) where IJEE = kcal/day; s = spontaneously breathing; v = ventilatory-dependent; A = age (years); W = actual body weight (kg), S = sex (male = 1, female = 0); T = diagnosis of trauma (present = 1, absent = 0); O = obesity greater than 30 percent above IBW from 1959 Metropolitan Life Insurance Tables or BMI greater than 27 (present = 1, absent = 0). |
| Penn State (2003b) (<60 years) | RMR (kcal/day) = Mifflin (0.96) + VE (31) + Tm(167) − 6212 VE = minute ventilation Tm = maximum body temperature |
| Penn State 2010 (>60 years) | RMR (kcal/day) = Mifflin (0.71) + VE (64) Tm(85) − 3085 |
Routes of Infusion
The components of a PN solution will determine the osmolarity and infusion route. PN can be administered as a total nutrient admixture (TNA) also known as a 3-in-1, which includes all macronutrients and micronutrients or as a 2-in-1 solution which excludes the IVFE.
Peripheral parenteral nutrition
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree