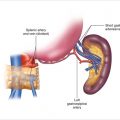
Figure 4.1
The parathyroid gland is grasped along its long axis (shown here with DeBakey forceps) and, using a scalpel with a #10 Bard Parker blade, whole tissue discs approximately 3 mm thick are sliced and removed. Strips of parathyroid tissue measuring 3 mm are then sectioned from a tissue disc and placed on a flat metal surface, where slivers of parathyroid tissue 1 × 3 mm in size are cut from the strip with a rocking motion of the blade
Figure 4.2
In preparation for grafting, the brachioradialis muscle bed is exposed, and a retractor is placed
Figure 4.3
(a) An incision is made in the overlying thin layer of fascia and the muscle fibers are separated. (b) A single parathyroid sliver is placed in each of 15–20 muscle pockets. (c) The muscle is then closed over the parathyroid piece with a single, nonabsorbable suture. (d) The transplanted parathyroid sliver must be buried 2–3 mm below the muscle surface and completely covered by muscle fibers. (e) The ends of each marking suture should be about 2–3 mm in length
Figure 4.4
Parathyroid sliver in a muscle bed 1 year after grafting (hematoxylin and eosin, original magnification ×100)
4.3 Results and Conclusions
Because parathyroid glands may be compromised during radical head and neck procedures, the transplantation of normal parathyroid tissue at the time of such procedures will substantially reduce the incidence of permanent hypoparathyroidism, and there has been little controversy about this indication. Since the original reports of TPTx in patients with primary or secondary parathyroid hyperplasia, investigators at numerous centers have published their experience with this technique. Results have varied from center to center, but generally they have been comparable to those achieved with SPT. The only randomized controlled trial comparing SPT versus TPTx was a single-institution study in patients with renal osteodystrophy. In this study, patients treated by TPTx had a more rapid normalization of serum calcium and alkaline phosphatase than those treated with SPT, as well as more rapid improvement in radiological signs and greater relief of symptoms such as pruritus and muscle weakness [8]. Unfortunately, no prospective, multicenter, randomized clinical trials have compared the results of the two operative procedures in patients with either primary or secondary parathyroid hyperplasia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree