Palliative Care in the Intensive Care Unit Setting
Thomas J. Prendergast
Intensive care units (ICUs) combine, in one physical location, the most desperately ill patients with the intensive care physicians and nursing staff who are trained to use the latest in medical technology. The result is an approach to patient care that has been characterized as “rescue medicine.” (1) This term correctly suggests that a primary goal of critical care medicine is to save the lives of patients who would have died without their aggressive interventions. The term also carries a negative connotation: in their zeal to save lives, critical care practitioners (intensivists) may undervalue the wishes of the patient, the needs of the family, pain and suffering caused by the treatment, and the potential for functional recovery, as opposed to mere survival. Because these concerns form the very core of palliative medicine, there is a widespread assumption that critical care medicine is at best indifferent and at worst antithetical to palliative care. For example, one of the major (negative) outcome measures of the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) study was the presence of a patient in an ICU before death (2).
Accusations of a rescue mentality are anecdotal and difficult to assess (3). We might infer a mindset of rescue medicine when all dying patients receive all therapies, including ineffective cardiopulmonary resuscitation (CPR). From the inception of ICUs in the 1960s till the 1980s, this was the approach to patients dying in ICUs. Since then there has been an astonishing evolution in critical care practice (Table 76.1). In 2001, most ICU deaths followed a considered decision to either withhold or to withdraw life-sustaining therapy (4). In the past decade, intensivists have acquired a new responsibility to manage the death of patients who do not survive. This is not yet palliative care, but it opens the door to palliative care because it raises the question: how is this newly appreciated responsibility to the dying patient handled, and how well (5)?
Table 76.1 Changing Management of Death Within American Intensive Care Units | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
Table 76.2 Median Predicted 2-Month Mortality Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Approaches to Palliative Care in the Intensive Care Unit
Some patients are referred to the ICU for symptom control that cannot easily be provided elsewhere in the hospital. Palliation of symptoms may require intensity of nursing care that is not available in the ward. It may require interventions that can be comfortably managed in the ICU [e.g., treatment of intractable distress with barbiturate or propofol coma (12)]. The therapeutic goal may be to initiate ICU-specific interventions (e.g., vasopressor support or assisted ventilation) allowing time for the family to arrive to say good-bye. Instances of specific, circumscribed palliative care are a legitimate, although uncommon, use of critical care resources. For such patients, the ICU is not only an appropriate location but also quite likely, the best place to die.
Patients admitted for symptom control represent a small minority of ICU admissions. Most patients are admitted to the ICU emergently, under the presumption of treatment until more information is available, or because the clinician and patient/surrogate have made a decision to pursue a trial of curative therapy. There is an expectation of recovery or, at least, uncertainty about prognosis. Most patients improve and are discharged. Mortality rates vary from <5% of admissions to some surgical ICUs, to 15% of admissions to general medical ICUs, to >40% of admissions to ICUs that primarily treat oncology patients (4, 13, 14). Age alone does not appear to be an independent predictor of mortality (15). Certain diagnoses place patients at higher risk for death (16, 17). Critically ill patients with cancer have a particularly poor prognosis, with multiple studies documenting in-hospital mortality rates from 50% to >90% in patients who develop critical illness following bone marrow transplant (18). A recent attempt to develop a mortality prediction model, specifically for patients with cancer identified three variables associated with higher mortality: allogeneic bone marrow transplant, progression of underlying disease, and poor performance status (13).
Patients admitted to the ICU for curative therapy also may benefit from palliative care. It is uncertain, however, which patients will benefit and when palliation should be emphasized in their course of intensive care. One approach emphasizes symptom control in patients known to be dying. Therefore, intensivists may arrive at palliative care through a natural extension of the ICU’s core mission to rescue the grievously ill: treat aggressively for cure until death appears inevitable, then redirect the goals of care to control the patient’s symptoms. This model and the accompanying language of transitioning from curative to comfort care have become commonplace in critical care medicine (19, 20). The transition approach demonstrates a willingness to acknowledge the dying and to attend to the details of patients’ deaths. In this sense, it is a significant advance beyond the relentless drive to treat, that sometimes has characterized critical care medicine. There are drawbacks to a transition approach, however. To state the obvious, there is more to palliative care than symptom control of the imminently dying. Another problem, one that remains underappreciated outside critical care medicine, is that it is surprisingly difficult to predict who is going to die (21, 22).
Table 76.3 Some Obstacles to Palliative Care in the Intensive Care Unit | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
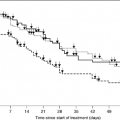
A transition model of palliative care in the ICU depends on the intensivist’s ability to identify a clinical change in individual patients that redirects the goals of care away from curative therapy toward symptom control. Experienced intensivists can accurately predict the short-term mortality of groups of patients; many computer-based mortality prediction models do the same (23). Neither computer-aided decision systems nor expert clinical opinion allows specific identification of the individual patient who will die (22). Data from the SUPPORT study (21) demonstrate that, in most patients, there are no identifiable points when death becomes imminent that allows for a change in direction of care (Table 76.2). These data challenge the assumption that we have advance notice of death. The uncomfortable reality is that a high percentage of ICU patients die but individual ICU patients are difficult to identify as dying. Therefore, if the criterion for palliative care in ICU patients is that the providers first recognize that the patient is imminently dying, ICU practice will be deficient in two ways. Many patients will die without the benefit of palliative medicine because they will die unexpectedly. Those
who do receive palliative care will receive it very late in their disease course.
who do receive palliative care will receive it very late in their disease course.
Despite an emerging consensus that palliative care can coexist in parallel with aggressive critical care, many clinicians in and out of ICUs strongly support the concept of a transition to palliative care. There are many reasons for the persistence of this approach. A few patients do have an abrupt change in their clinical course that significantly changes their prognosis (e.g., the elderly patient with lung cancer who has a myocardial infarction that precipitates cardiogenic shock). Predicted survival may drop precipitously with additional organ dysfunction, and appreciation of this change may facilitate a decision to limit therapy. In other patients, the decision to change the direction of therapy is based on nonprognostic factors, such as suffering, quality of life, or comorbid illnesses, that suggest a high likelihood of recurrent hospitalization or death despite the possibility of short-term recovery (24). The same patient, although hemodynamically stable but with severe permanent left ventricular dysfunction, may face a degree of debilitation that he and his family may find to be unacceptable. Sometimes, clinicians and families frame the facts to suit their need for explanations in a way that creates transitions (25). Perhaps the patient’s quality of life will be no different after the myocardial infarction but the event reshaped the patient and family’s thinking toward acceptance of his mortality.
Finally, the transition model permits separation of the curative and palliative roles. To the extent that this separation allows the intensivist to withdraw from involvement as death approaches, it may represent a strategy to cope with feelings of helplessness, failure, and grief (26). The alternative, to assert that all patients at high risk of dying need palliative care, asks the intensivist simultaneously to be an advocate of rescue and palliative medicine (21, 27). To assume both these roles is to move far beyond the transition model.
Adapting Palliative Care to the Intensive Care Unit
Palliative care in or out of the ICU starts with adequate symptom control. Symptom control is essential because pain and suffering without purpose are destructive, because untreated pain may adversely affect outcomes (28, 29, and because unrelieved pain and suffering interfere with the patient’s ability to address important life issues that may be brought to closure before death. Palliative medicine promises more than symptom control, however. It emphasizes the possibility of growth at the end of life. Palliative care means acknowledging and addressing psychological suffering (depression, anxiety), existential suffering (estrangement, alienation, lost opportunities, and the meaning of one’s life), and spiritual suffering (Why am I dying?) (30). This ideal of palliative care depends upon a predictable disease course that allows time to plan and a patient who is alert enough to speak for himself and to participate in discussions of both medical planning and personal growth with a provider who has a relationship with the patient and, preferably, has known the patient and the family over time. Critical care medicine violates this model in almost every respect (Table 76.3) (31).
Some of the barriers to palliative care listed in Table 76.3 actually contribute to the success of critical care medicine. An emphasis on technology, and expert providers willing to push its limits, are desirable if they help the desperately ill and injured. Other barriers seem inevitable if less desirable. In an environment dedicated to treating the sickest patients, prognostic uncertainty dictates that some patients will die under aggressive therapy to successfully treat those who survive. This is neither a mistake nor necessarily a failure but an expected consequence of not knowing who will respond to treatment (27). The nature of critical illness is that clinical situations change rapidly and decisions must be made quickly. Pervasive prognostic uncertainty, pressure to make decisions, and significant mortality seem an inescapable part of the ICU environment. Some barriers shown in Table 76.3 are cultural and, therefore, subject to change. Struggling to save lives is fully consistent with acknowledging that the quality of death can be as important as the quality of life (32). To teach the importance of interpersonal relations and communications skills, need not devalue the technical and scientific accomplishments that distinguish modern critical care. Technology does not imply dehumanization; intensivists can be full participants in the human stories being played out under their care.
There are key elements of palliative care that are adaptable to the ICU in a way that improves the care of patients while respecting the critical care provider’s appropriate role as advocate for the desperately ill. These features of palliative medicine are not inconsistent with good ICU practice. They are increasingly seen to define good ICU practice (19, 27, 33, 34, 35). The internist or oncologist whose patient is admitted to the
ICU may reasonably expect this degree of expertise from their ICU staff, if not now, at least as a goal to be reached in the near future.
ICU may reasonably expect this degree of expertise from their ICU staff, if not now, at least as a goal to be reached in the near future.
First, as mentioned, it is absolutely essential that adequate attention be paid to symptom control. There are very few situations where attention to the physical and psychological needs of patient’s conflicts with curative treatment. Palliative care can teach the intensivist about good symptom management.
A second aspect of palliative care applicable to the ICU is to recognize that each individual patient lives within a web of human relationships. To care for a critically ill patient is to have a relationship, not only with the patient but also with all those people to whom the patient is related. Regardless of the caregiver’s interest or willingness to explore those relationships, the caregiver cannot escape the complex and frequently difficult communications environment that those relationships create. The ability to communicate effectively with groups of people is absolutely essential to the intensivist. Because of uncertainty about the prognosis is pervasive and colors everything else that occurs in the ICU, a communication strategy that diffuses the power of uncertainty by acknowledging it directly, facilitates good ICU care therefore opening the door to good palliative care.
Third, a fundamental principle of palliative care is acceptance of impending death, by the patient, by loved ones, and by the health care provider. In the ICU, the unexpected nature of illness or injury combined with prognostic uncertainty leads to common self-protective strategies. In their hope of recovery, family members may deny the possibility of death whereas physicians may avoid discussion of death. The approach from palliative care means acknowledging the possibility of death in an ongoing discussion with the family and, when appropriate, moving to limit life-sustaining treatments. It is in the area of withdrawal of life-support that intensivists have most clearly changed their practice and where the most concrete recommendations can be offered.
Pain and Symptom Control in the Intensive Care Unit: General Principles
There are multiple reasons for patients to experience pain, anxiety, dyspnea, and other distressing symptoms during treatment in the ICU. Surgical procedures, bedside instrumentation, placement and maintenance of an endotracheal tube including endotracheal suctioning, and prolonged immobilization, in addition to the trauma or serious illness that warranted hospitalization in the first place, all may cause significant physical and psychological symptoms (36, 37). Patients report significant distress associated with pain that may manifest as anxiety or agitation (38). In a recent survey, hunger, thirst, and disruption of sleep were reported as moderate or severe by >50% of ICU patients (39). The act of weaning patients from mechanical ventilation may be associated with significant anxiety even in patients who are clinically improving (40). The overall symptom burden may be particularly high in dying patients (41).
Despite the apparent prevalence of pain and other symptoms, rigorous research into prevalence and control of symptoms has been scarce. Partly, this lack of research reflects the difficulty of symptom assessment in ICU patients. Critically ill patients frequently have altered cognition, they may either be heavily sedated or a significant proportion is endotracheally intubated, which renders them speechless. Although there are symptom assessment tools that can assist providers in obtaining information in many patients (42, 43, including intubated and dying patients (39), these tools are time consuming and labor intensive, and have not generally been tested for both reliability and validity (44, 45). In the routine practice of critical care medicine, symptom assessment has been subjective and poorly standardized (46).
The most basic principle in the assessment of pain is that pain is irreducibly subjective (42). Therefore, the best indicator of pain is the patient’s own report. Patients who can report their pain should be treated accordingly, although their cognition may be altered by illness or medication, and the stress of critical illness may significantly change their ability to cope with or to describe pain. Appropriate treatment always requires a careful pain history, particularly a history of chronic opioid use, to dose analgesics correctly. Instruments available for patients who can communicate range from a simple linear scale to quantify the pain, to more intricate inventories of psychological states such as the McGill pain questionnaire (47). Visual analog scales require less cognitive processing than visual descriptors or numerical rating scales but do require that the patient be able to see (42). None of these scales has been validated in critically ill patients.
Patients who cannot describe pain may manifest it as “agitation.” Agitation is not a diagnosis but a description of excessive or inappropriate motor activity. Despite the difficulty of identifying a specific etiology, a diagnostic review of the agitated patient is essential before instituting therapy. Anxiety, fear, frustration with inability to communicate, pain, delirium, dyspnea, and ventilator dyssynchrony all may manifest as agitation. Failure to search for an etiology may lead to inappropriate treatment. To treat pain with sedatives that have no analgesic properties may require excessive sedation to the point of general anesthesia. Delirium may be exacerbated by opioids or benzodiazepines and is best treated with haloperidol.
In >50% of ICU patients who cannot report their subjective experience, assessment is particularly dependent on careful physical examination for potential sources of pain, such as early decubiti, pressure points, intravenous lines, surgical wounds, traumatic fractures, and constricting bandages or restraints. Assessment of the nonverbal patient also depends on the observation of nonspecific physiological data, such as changes in blood pressure and heart rate, tearing or diaphoresis, along with a subjective assessment by the provider of the patient’s appearance and how the patient responds to specific treatments such as, turning, positioning, and suctioning (42, 48). Observational methods that do not elicit information directly from the patient lack sensitivity and specificity (39, 46). Family members may help interpret nonverbal information in such patients, although the validity of such surrogate interpretations is unknown.
Virtually all ICU patients require sedation, analgesia, or both to protect them and facilitate their treatment (49). To administer sedating agents presupposes a therapeutic goal and a way to determine when that goal has been reached. These goals are sometimes poorly defined, the assessments may be made subjective, and documentation of both is frequently poor. A recent systematic review of sedation scoring systems (44) identified 25 sedation instruments, of which only four (one pediatric scale) had been tested for both reliability and validity. The oldest and most widely used scale in adult ICU patients is the Ramsay Scale (50). In many institutions, this has been superseded by instruments that discriminate better among levels of agitation (Table 76.4). A first step in improving sedation practice is to standardize assessment of therapeutic goals and patient assessment using one of these instruments. Systematic assessment can be combined with therapeutic algorithms to perform continuous quality improvement (51). Nonpharmacologic strategies to manage agitation may be underutilized (52, 53).
Table 76.4 Quantitative Assessment of Sedation in Critical Care | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
Current Practice
Most of the data regarding symptom control are found in studies of pharmacologic management of pain and agitation. There is a paucity of data on nausea, dyspnea, sleep deprivation, and so on. Studies of pain management in the ICU suggest systematic undertreatment. The SUPPORT study (2) is a major reference point for the management of pain in severely ill, hospitalized patients, half of whom were treated in ICUs during their hospitalizations. Twenty-two percent of patients interviewed in the second week of the SUPPORT study reported that they had “moderate or severe pain almost half the time.” Family members of patients who died reported that their loved ones had been in moderate or severe pain half the time. Puntillo reported a series of 24 primarily surgical ICU patients where 63% of patients reported moderate to severe pain (56). Whipple et al. investigated the different perceptions of physicians, nurses, and 17 patients admitted to the ICU after a traumatic injury (57): 95% of house staff and 81% of nurses reported the patients received adequate pain control but 74% of patients reported significant pain (27% moderate and 47% severe). The conclusion seems inescapable: intensivists systematically undertreat pain.
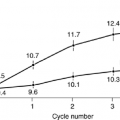
A number of recent papers have raised questions about systematic oversedation. Kress et al. reported the results of a randomized controlled trial in 128 medical ICU patients (58). In the intervention group, sedative infusions were interrupted each morning until the patients were awake or uncomfortable; in the control group, the infusions were not interrupted routinely but at the discretion of the ICU clinicians. The investigators found a shorter duration of mechanical ventilation and shorter ICU length of stay in the intervention group, along with fewer diagnostic studies to assess altered mental status. No measure of patient distress or satisfaction was reported in the original paper. The authors have subsequently published in abstract form a summary of patient interviews that does not reveal any difference in psychological well-being, depression, or post-traumatic stress disorder between intervention and control patients (59). Only 1 patient of 12 recalled awakening from sedation; the patient was a control subject. These data suggest that, in a medical ICU, the current standard of practice sedates mechanically ventilated patients so heavily that it may prolong their ICU stay.
It is not yet clear how to reconcile these findings with data that pain is undertreated. Sedation may be given excessively whereas analgesics are underdosed. In particular, continuous infusion of sedatives and analgesics may prolong mechanical ventilation but the constant levels so achieved may not suffice for procedural pain from suctioning, turning, and other aspects of ICU care that patients report are uncomfortable (60). Given the paucity of data on patient distress or satisfaction, it may be that adequate symptom control requires medication that itself prolongs ICU treatment (39).
There are even fewer data about the management of pain and sedation in ICU patients at the end of life. This clinical context is very specific: most patients who die in ICUs have life-support withheld or withdrawn. The usual considerations of balancing adequate sedation with hemodynamic stability or avoiding prolongation of mechanical ventilation are no longer issues. There may be new considerations. Some patients may want to remain alert as long as possible to be able to communicate with their families. Some providers may worry about administering large amounts of opioids or sedatives to a patient who will die soon afterwards, for fear that such practice blurs the line between withdrawal of life-support and active euthanasia.
Two studies address to this question. In 1988–89, Wilson et al. retrospectively reviewed over 1 year all patients at the San Francisco General Hospital who had life-support withheld or withdrawn (61). They randomly selected an equivalent number (n = 22) of patients from their affiliated University Hospital. Seventy-five percent (33/44) of the patients who had received either sedation or analgesics or both, at doses that were significantly increased from baseline, once the decision was made to withdraw life-support, died. The rest who did not receive sedation were deeply comatose and died faster than those who received additional medication. The authors concluded that administration of opioids and sedatives was
common in the withdrawal of life support from ICU patients and did not appear to hasten death. The latter conclusion was seriously weakened by significant clinical differences between the two patient groups.
common in the withdrawal of life support from ICU patients and did not appear to hasten death. The latter conclusion was seriously weakened by significant clinical differences between the two patient groups.
Hall and Rocker reviewed charts from 174 consecutive patients who died over a 1-year period in 1996–97 (62). Seventy-nine percent (138/174) had life-support withheld or withdrawn, whereas 21% (36/174) had aggressive therapy continued up to the time of death. Doses of morphine and lorazepam were fivefold higher in patients from whom life-support was withdrawn, and most of this increase occurred in the 4 hours before death. Neuromuscular blocking agents (NMB) were administered to 25 patients, of whom 17 had NMB started in the last 12 hours of life. In 20% (5/25) patients a single dose of NMB was administered to facilitate endotracheal intubation. Nine patients had an NMB infusion at the time of death, five of whom had life-support (but not mechanical ventilation) withdrawn. Sixteen percent (4/25) of patients receiving NMB were also receiving intermittent sedation/analgesia but not continuous infusions.
These and other studies show that the range of opioid doses necessary to control acute pain or dyspnea is very wide; large doses may be necessary. However, the dose in milligrams is much less relevant than careful administration. It is entirely appropriate to give large amounts provided that these doses are carefully titrated to specific effects. In rare cases, it may only be possible to control symptoms with doses that hasten death. Provided that the intended effect is relief of suffering and the doses are carefully titrated to that effect, there is broad consensus in bioethics and the law that ameliorating symptoms is not euthanasia, that is, not the deliberate administration of drugs with the intent to terminate the patient’s life (63, 64). One of the most egregious failings in end-of-life care is the systematic failure to adequately to treat pain and dyspnea, based on a misunderstanding of this distinction (65).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree