Author
No. of Pts
Treatment
Response rate (%)
Median survival (months)
First–line treatment chemotherapeutic agents
Jacobs
245
PF
P
F
32a
17
13
5.5
5.0
6.1
Forastiere
277
PF
CF
M
32a
21
10
6.6
5.0
5.6
Clavel
382
PMBV
PF
P
34a
31a
15
7.0
7.0
7.0
Gibson
218
PF
PPac
27
26
8.7
8.1
Forastiere
210
PacP
HDPacP
36
35
7.0
7.0
Urba
397
PPlac
PPem
8.1
12.1
6.3
7.3
Fountzilas
166
PacGem
Pac-LD
20
29
8.6
11.05
First-line treatment with targeted agents
Schrijvers
240
PF
PF+ INF
47.1
37.4
6.3
6.0
Burtness
117
P+ Plac
P+ C
10
26a
8.0
9.2
Vermorken
657
PF
PF + Pan
9.0
11.1
Vermorken
442
PF
PF + C
20
36a
7.4
10.1a
Second-line treatment
Stewart
486
G250
G500
M
2.7
7.6
3.9
5.6
6.0
6.7
Argiris
270
DocPlac
Doc + G
6.2
12.5
6.0
7.3
Machiels
483
M
Afatinib
5.6
10.2
1.7
2.6b
Many combinations of chemotherapeutic agents and targeted drugs (e.g., interferon, cetuximab, panitumumab) are not superior in terms of overall survival compared to chemotherapy alone [19–21]. Only in one study, the combination of chemotherapy with cetuximab resulted in an improved overall survival (overall survival 7.4 versus 10.1 months, hazard ratio (HR) for death, 0.80; 95 % confidence interval (CI), 0.64–0.99; P = 0.04) compared to chemotherapy alone [22].
After progression on first-line treatment, some patients are still fit enough to receive second-line treatment. However, none of the newer drugs (e.g., gefitinib, axitinib) were able to improve overall survival compared to chemotherapy (e.g., methotrexate, docetaxel), although axitinib induced a slightly higher progression-free survival (median progression-free survival 2.6 months versus 1.7 months; HR 0.80; 95 % CI 0.65–0.98; P = 0 · 030) [23–25].
Since overall survival is not influenced by most of the treatments, improving quality of life (QoL) is one of the most important aims of chemotherapeutic treatment in this patient population. However, studies looking at QoL were not able to demonstrate an important improvement in QoL [23, 26], and even the influence on pain was not significantly better by giving the newer drug combinations compared with the older ones [26].
These data show that the impact of anticancer treatment in patients with RMHNC is limited in terms of survival and even on QoL. Therefore, patients should be carefully selected for anticancer treatments, and the treatment regimen should be individualized based on comorbidity and treatment aim.
A conceptual framework may be used to select anticancer treatment (Fig. 17.1). Patients with RMHNC have a certain symptom burden due to disease recurrence but also due to the residual toxicity of previous treatments. The optimal treatment approach should decrease the total disease burden compared to the initial status by combining an important disease regression and minimal toxicity. However, if the treatment does not lead to a tumor control and induces a significant toxicity, it increases the symptom burden and such treatments should not be offered since they only decrease QoL.
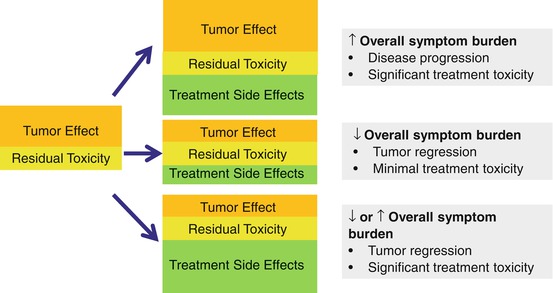
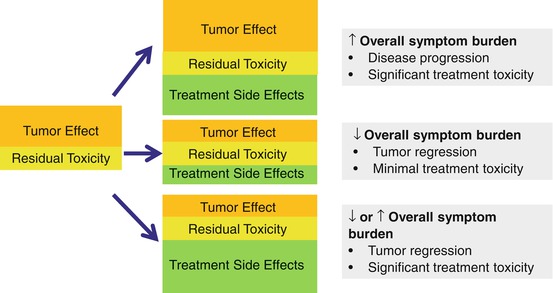
Fig. 17.1
Symptom burden according to disease control and treatment toxicity (Based on Jackson et al. [11])
Palliative Care in Patients with RMHNC
Palliative care is an approach that improves the QoL of patients and their families facing the problem associated with life-threatening illness. This aim is realized through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of physical, social psychosocial, and spiritual problems [27]. Palliative care should be given by a multidisciplinary team that addresses all these problems.
Physical problems can be addressed by a palliative treatment, directed towards the cancer itself (e.g., palliative chemotherapy, palliative radiotherapy), with the aim to control or decrease the disease hereby improving QoL. In this setting, cure is not an aim (≠ treatment with curative intent).
At the same time, symptomatic treatment approaches (e.g., analgesics) that address only the problem without doing something against the cancer itself should be initiated to control symptoms.
Studies have shown that including palliative care in patients with cancer improves their QoL and sometimes their survival [28] and all patients with RMHNC should be offered palliative care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree