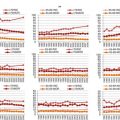
Diagnosis
Median age
% of patients dying
Place of death
In hospital
Home
Nursing home
Hospice
MM
73.0
63.4
64.5
15.7
12.0
7.8
DLBCL
70.4
51.8
64.5
14.7
11.3
9.6
MDS
76.0
74.9
70.9
15.8
7.4
5.9
AML
71.1
79.4
72.1
14.1
7.2
6.6
CLL
71.6
33.2
65.1
17.5
11.8
5.6
MPN
71.2
23.8
56.9
17.7
18.7
6.7
FL
64.5
22.6
61.5
19.6
10.8
8.1
HD
44.1
21.9
74.6
13.5
7.9
4.0
MCL
74.0
71.1
53.7
19.5
10.6
16.2
TCL
64.9
56.8
70.9
17.1
4.3
7.7
CML
59.2
21.7
72.7
9.1
11.4
6.8
In-Hospital Situation
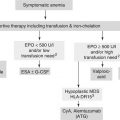
Hematological malignancies where associated with higher death rates, higher in-hospital mortality and lower discharge rates in an acute palliative care unit compared to patients with solid tumours [4].
Providing Hospice and Palliative Care
Howell et al. performed a systematic review and meta-analysis to identify the frequency of patients with hematological malignancies that received palliative or hospice care [1]. Twenty-four studies were identified, nine could be included. All in all, patients with hematological malignancies were less likely to receive palliative or hospice care compared to patients with solid tumours. The following possible reasons were mentioned: (a) ongoing management by the haematology team and consequent strong bonds between staff and patients, (b) uncertain transitions to a palliative approach to care, (c) sudden transitions, leaving little time for patients, input.
In a further analysis, the authors report on the use of specialized palliative care (SPC) referrals in a population-based cohort of 323 patients diagnosed with acute myeloid leukaemia, diffuse large B-cell lymphoma or multiple myeloma over a 5-years period who died within 2–7 years after diagnosis. 48 % of them had at least one SPC referral. The following factors were associated with higher use of SPC: longer survival (>12 months vs. <1 months), multiple myeloma vs. acute myeloid leukemia. Patients dying not in hospital had a higher rate of SPC referrals. Forty-four percent of the patients included were 75 years and older [5].
Sexauer et al. report that there are about 70,000 deaths of patients with hematological malignancies each year in the US. Only 2 % of them use a hospice. They report a length of stay of 9 days in home hospice care and of 6 days in inpatients hospice care, with some of them receiving blood transfusion during hospice stay [6].
Prognosis
The majority of prognostic scores are based on patients, and disease characteristics when patients are newly diagnosed with a certain disease, for more details see the specific chapter for the different diseases in this book.
Other prognostic scores have been proposed to better adjust the likelihood of dying within a certain period after transition of patients to palliative care. They mainly included physicians, estimate of survival time, performance status, presence of symptoms, such as dyspnoea and cachexia, and some lab-results [7].
None of them focuses on patients with hematological malignancies in a palliative care setting.
Kripp et al. analysed factors associated with survival of 290 patients with hematological malignancies referred to an in patient acute palliative care unit [8]. The following factors were identified: (a) Eastern Cooperative Oncology Group (ECOG) Performance Status (PS): 0–2 vs. 3–4; (b) platelet counts: >= 90 vs. <90 × 10 E-9/L; (c) Lactate-Dehydrogenase (LDH) < = 248 vs. 248 U/L; (d) opioid use: WHO level 0–2 vs. 3; (e) albumin > =30 vs. <30 g/L; (f) packed red blood cell transfusion no vs. yes. According to the above mentioned factors, the authors suggested three different risk groups, see Table 19.2.
Table 19.2
Number of risk factors, frequency of patients, and outcome regarding survival in patients with hematological malignancies referred to an acute palliative care unit [8]
No. of risk factors | No. of patients | Median time of survival |
|---|---|---|
0–1 | 48 | 440 days |
2–3 | 120 | 63 days |
4–5 (6) | 78 | 10 days |
Age, comorbidities, or other items of a comprehensive geriatric assessment were not included in the analysis.
The time of referral to palliative care is not a clearly defined and generally known point of time within the course of the disease, but varies widely from factors such as availability of service etc that are not patient- or disease-related. This limits the use of prognostic scores in the palliative care setting.
Burdens of Symptoms in Patients with Hematological Malignancies
The palliative care approach is more symptom-than disease-orientated. Symptoms in patients with hematological malignancies are common. Manitta et al. reported a mean number of symptoms of 8.8 in 180 patients diagnosed with hematological malignancies with a median age of 61 years, range 17–95 years. Most common symptoms were lack of energy 69 %, feeling worried 50 %, difficulty to sleep 41 %, feeling sad 41 %, drowsiness 41 %, dry mouth 40 %, pain 39 %, numbness hands/feet 38 %, shortness of breath 36 %, irritability 36 %, difficulty concentrating 34 %, cough 33 %, feeling nervous 33 %, lack of appetite 27 %. The mean number of symptoms was significant greater in those on treatment, those with poor performance status, inpatients, and those with advanced disease [9]. Age was not included in the analysis.
The prevalence and type of symptoms of patients with hematological malignancies in the palliative care setting varies according to the type of underlying disease. However data are limited. Following we report some data for patients with acute myeloid leukaemia, multiple myeloma, and for patients with malignant lymphoma.
Acute Leukaemia
Zimmermann et al. reported the symptoms of patients with acute leukaemia, mainly acute myeloid leukaemia, referred to a palliative care service. Two hundred and forty-nine were included. The analysis was not restricted to elderly patients. The patients reported nine physical and two psychological symptoms. Main symptoms reported lack of energy 79 %, feeling drowsy 56 %, difficulty sleeping 55 %, dry mouth 54 %, weight loss 53 %, lack of appetite 52 %, change in taste of food 51 %, pain 49 %, nausea 45 %, worrying 43 % [10]. Only 2 of 35 patients dying in the period of the study were referred to a palliative care service.
Stalfeld et al. reported the final phase of 106 adult patients with acute myeloid leukaemia, who died. Twenty-seven were treated with curative intent, 79 were in a palliative care approach. Forty-four percent suffered from bleeding, 71 from infection and 76 from pain in the last week of their life [11].
Multiple Myeloma
Palliative care needs of patients with multiple myeloma in advanced disease are often dominated by symptoms of the disease, especially pain, related to bone destruction, infections, bone marrow failure and renal impairment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree