and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Acute Pain Crisis
Definition
The Acute Painful Crisis (APC) is an episode of pain, usually of abrupt onset, which in severe cases requires hospital treatment with opioid analgesia. Since there is no diagnostic test for APC, other potential causes of pain need to be excluded.
Etiology
APC is thought to be a clinical consequence of sickle hemoglobin-containing red blood cells becoming trapped in the microcirculation, leading sequentially to ischemia, infarction, reperfusion, and inflammation. Within the bone marrow, the result of this process is local tissue damage and increased intra-osseous pressure, together with the release of a variety of chemical mediators. These activate nociceptive neural pathways in the peripheral and central nervous system, leading to the perception of pain. Some features of APC, for instance the mechanism whereby trigger factors (temperature changes, infection, over-exertion, physical and psychological stress) lead to the onset of crisis, and the mechanisms whereby the site of pain changes and multiple sites of pain are recruited during the course of the episode, are poorly understood.
Incidence
APC is by far the commonest acute complication of SCD, but is highly variable in frequency. The majority of episodes are managed at home and usually go unrecorded. These mild episodes nevertheless result in significant morbidity, including exclusion from education, work and social activities as well as psychological maladaptation. Assessing frequency using a pain diary, or by careful systematic enquiry at routine out-patient clinic visits is important.
A recent American study showed that adults experienced pain on 50 % of days but only access health care services on 3 % of days. Another study found that patients have an average of 2.5 acute care encounters and 1.5 hospital admissions per year. Twenty-nine percent of patients do not seek acute care at all, whilst 16 % have 3 or more acute care encounters over 1 year.
The incidence of APC tends to increase during childhood and peak in adolescence and early adulthood, and in this age range is more common in males (Fig. 5.1). Pain crises become less frequent in patients over the age of 40.
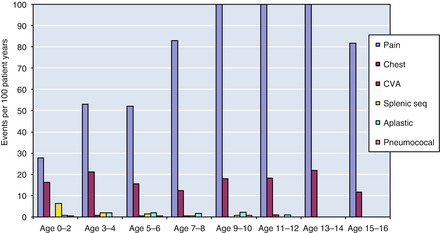
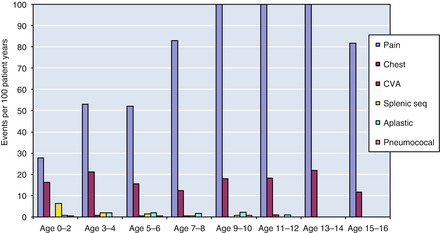
Figure 5.1
Age specific rates of acute painful crisis and other acute complications in the East London Newborn Cohort (data from HbSS children)
UK Health Service Perspective
NHS hospital treatment episodes with a diagnosis of SCD doubled over the previous 10 years to about 25,000 per annum by 2009/10. On average, a patient will be admitted once per year, for 3–4 days. The majority of admissions are in London and occur most frequently in the age group 15–25 years. SCD is also the commonest reason for repeated readmissions to hospital within 28 days in London.
Presentation, Course and Complications
Typical precipitating factors include exposure to adverse weather conditions (particularly cold wind or rain) with inadequate clothing, over exertion, swimming in cold water, and psychological stress including family crises, school and university exams. APC can also accompany other acute complications, such as acute anemic episodes, infections, abdominal and respiratory crises, and may be a feature of some delayed transfusion reactions. Sometimes there is no apparent trigger. Patients are often able to recognise a prodrome of malaise, fatigue and gradual onset of pain. Pain may be intermittent and fluctuate in location, but usually there is a specific site or sites of maximum intensity. Ballas et al. have studied a large number of APC episodes and have described the evolution of pain and biomarkers in a four-stage scheme (1) prodromal (2) initial infarctive (3) established and (4) resolving (see http://asheducationbook.hematologylibrary.org/content/2007/1/97.full). Fever and increased inflammatory markers are typical of the later stages of a crisis, and the patient is often incorrectly diagnosed as suffering from infection.
About 50 % of children with HbSS experience hand and foot syndrome (dactylitis) as their first crisis, usually between 6 months and 3 years of age. Children in the age range 2–5 years often experience limb pain and swelling (thigh, shin, knee, forearm, elbow, upper arm). This swelling is characteristic, and should not be confused with septic arthritis or osteomyelitis. Abdominal pain is also common in childhood. The chest, back, pelvis and proximal limb bones become more common sites in older children and adults, probably reflecting the sites of active bone marrow in these age groups.
APC can last from several hours up to several weeks. More prolonged episodes are probably related to extensive bone infarction and a lengthy phase of inflammation and healing. In adults it is common for pain to persist after discharge from acute hospital care, and recurrences of acute pain requiring readmission to hospital are part of the typical course. These may be related to increased blood viscosity due to high levels of inflammatory mediators and to the adhesive properties of reticulocytes which increase as the bone marrow recovers.
One of the most important complications of APC is acute chest crisis (ACS). Monitoring for development of ACS with regular assessment of respiratory rate, oxygen saturation and daily examination of the chest is an essential part of the management of APC.
Diagnosis
There are no specific diagnostic tests for APC. This is a clinical diagnosis based on the patient’s history, the similarity to previous episodes of APC, and exclusion of other possible causes of pain.
Assessment and Investigations
A proforma capturing the important points in the history and examination is shown in Appendix 1. The essential baseline observations should include pain score, sedation score, respiratory rate and oxygen saturation.
Essential laboratory and radiological examinations are shown in Table 4.3. Hemoglobin electrophoresis is not routinely required (HbS% does not change during APC).
Home Management
Hospital Management
The care pathway for APC needs to carefully planned and explained. Usually, the patient presents to the emergency department (ED), and from there is transferred to an acute care ward. In high prevalence areas, there is often a dedicated ward. Monitoring of pain score and vital signs, together with administration of analgesia continues seamlessly along the journey from ED to the medical ward. One of the roles of a sickle cell nurse specialist is to facilitate and co-ordinate this care pathway. Staff need to develop expertise in pain management, and should be able to identify signs of deterioration, and develop an understanding of the patient’s perspective in order to provide sympathetic and responsive care. Training of medical and nursing staff is important and will influence outcomes, in terms of efficacy, safety and patient satisfaction with the care pathway.
Day Care management is a suitable alternative model of care for uncomplicated APC episodes. Patients can be assessed and treated rapidly by a specialized team of nurses and doctors. A limited number of boluses of strong opiate analgesia can be given, either by mouth or by injection. At the end of the day, the patient can be discharged home, provided no additional complications develop, and that there is a carer present to observe and support the patient at home. The patient can reattend the next day if necessary. Day Care management is generally preferred by patients, and can lead to substantial cost savings if hospital admissions are prevented. This care model works best with extended opening hours, since the majority of acute presentations occur outside of the working day.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree