Overview of Resections around the Shoulder Girdle
James C. Wittig
Martin M. Malawer
Kristen Kellar-Graney
BACKGROUND
The upper extremity is involved by bone and soft tissue neoplasms only one-third as often as the lower extremity.3 The scapula and proximal humerus are common sites of primary sarcoma, including osteosarcoma and Ewing sarcoma in children and chondrosarcoma in adults. Metastatic tumors, especially hypernephroma, also have a propensity for the proximal humerus. When soft tissue tumors occur in the upper extremity, they tend to favor the shoulder girdle and may secondarily involve the scapula, proximal humerus, or clavicle. The axilla is another site around the shoulder girdle where primary soft tissue tumors may develop or where metastases can spread to and replace the local lymph nodes. The axilla is a relatively “silent” area, where tumors may grow to large sizes before they become symptomatic and are detected.
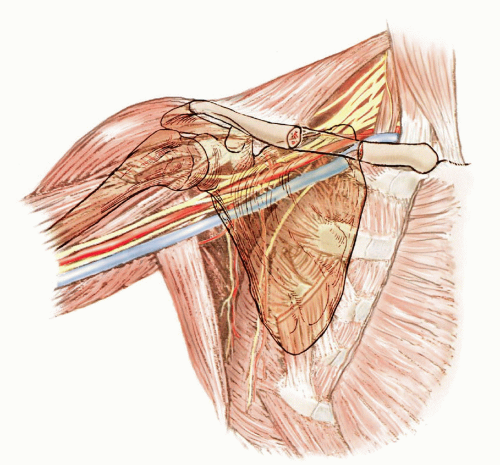
The shoulder girdle consists of the proximal humerus, the scapula, and the distal third of the clavicle as well as the surrounding soft tissues. Each bone may be involved by a primary malignant bone tumor or metastases, with or without soft tissue extension. The bones of the shoulder girdle also may be secondarily involved by a soft tissue sarcoma, which requires resection and reconstruction techniques similar to those of a primary bone tumor (FIG 1).
Until the mid-20th century, forequarter amputation was the treatment for malignant tumors of the shoulder girdle. Today, about 95% of patients with sarcomas of the shoulder girdle can be treated safely by limb-sparing resection such as the Tikhoff-Linberg resection and its modifications.6 The relation of the neurovascular bundle to the tumor and other structures of the shoulder girdle is the most significant anatomic factor in determining resectability, removal of the tumor, and reconstruction.
The resection and reconstruction of tumors of the shoulder girdle consists of three components:
Surgical resection of the tumor following oncologic principles
Reconstruction of the skeletal defect (ie, endoprosthetic replacement)
Soft tissue reconstruction using multiple muscle transfers to cover the skeletal reconstruction and provide a functional extremity
The goals of all shoulder girdle reconstructions are to provide a stable shoulder and to preserve normal elbow and hand function. The extent of tumor resection and remaining motor groups available for reconstruction dictate the degree of shoulder motion and function that are retained.
Historical Background
Some of the earliest discussions concerning limb-sparing surgery focused on techniques for resection of tumors about the scapula. Initial reports of shoulder girdle resections were confined to the individual bones or portions of the scapula. The first reported scapular resection was a partial scapulectomy performed by Liston in 18197 for an ossified aneurysmal tumor. Between this time and the mid-1960s, several other authors discussed limb-sparing resections about the shoulder girdle.4,11,12,13,14,15,16,19 In 1965, Papioannou and Francis17 reported 26 scapulectomies and discussed the indications and limitations of the procedure.
The Tikhoff-Linberg interscapulothoracic resection or triple-bone resection was described in the Russian literature by Baumann1 in 1914. He referred to a 1908 report by Pranishkov that described the removal of the scapula, the head of the humerus, the outer one-third of the clavicle, and the surrounding soft tissue for a sarcoma of the scapula. The shoulder was suspended from the remaining clavicle by metal sutures. Tikhoff and Baumann performed three such operations between 1908 and 1913, and Tikhoff was named as the originator of the procedure. The technique became established in the Western surgical community only after Linberg’s English publication in 1926.6
Classically, most shoulder girdle resections were done for low-grade tumors of the scapula and for periscapular soft tissue sarcomas. Before 1970, most patients with high-grade spindle cell sarcomas (eg, osteosarcoma, chondrosarcoma) involving the shoulder girdle were treated with a forequarter amputation. In 1977, Marcove et al12 were the first to report limb-sparing surgery for high-grade sarcomas arising from the proximal humerus. These authors reported performing an en bloc extra-articular resection that included the proximal humerus, glenoid, overlying rotator cuff, lateral two-thirds of the clavicle, deltoid, coracobrachialis, and proximal biceps. Local tumor control and survival rates were similar to those achieved with a forequarter amputation. Resection, however, preserved a functional hand and elbow. These early results were confirmed by other surgeons.5,18 After the 1980s, osteosarcoma, chondrosarcoma, and Ewing sarcoma of the proximal humerus became the tumors most commonly treated with a Tikhoff-Linberg resection. A variety of new techniques and modifications of shoulder girdle resections have been developed. Most have been reported as Tikhoff-Linberg or modified Tikhoff-Linberg resections. These eponyms are not accurate descriptions, however, because the Tikhoff-Linberg procedure was not intended to refer to sarcomas of the humerus.
As the popularity of limb-sparing surgery for shoulder girdle sarcomas grew, the extent of resection necessary for various tumors, particularly indications for an extra-articular resection, remained a matter of debate. The best method for reconstruction also came under considerable discussion.
In response, Malawer et al developed a surgical classification system (FIG 2) based on tumor location, extent, grade, and pathologic type. This system was intended to provide guidelines regarding the extent of resection necessary for primary bone sarcomas and soft tissue sarcomas that secondarily involve the bones of the shoulder girdle.
SURGICAL CLASSIFICATION SYSTEM
The current surgical classification system was described by Malawer and associates2,8,9,10 in 1991 (see FIG 2). It is based on the current concepts of surgical margins, the relation of the tumor to anatomic compartments (ie, intracompartmental vs. extracompartmental), the status of the glenohumeral joint, the magnitude of the individual surgical procedure, and precise considerations of the functionally important soft tissue components. It includes six categories:
Type I: intra-articular proximal humeral resection
Type II: partial scapular resection
Type III: intra-articular total scapulectomy
Type IV: extra-articular total scapulectomy and humeral head resection (classic Tikhoff-Linberg resection)
Type V: extra-articular humeral and glenoid resection
Type VI: extra-articular humeral and total scapular resection
Each type is subdivided according to the status of the abductor mechanism (the deltoid muscle and rotator cuff):
Abductors intact
Abductors partially or completely resected
Type A resections, in which the abductors are preserved, usually are recommended for high-grade spindle cell bone sarcomas that are entirely intracompartmental (ie, contained within either the proximal humerus or scapula bone). This is a rare situation, however. This type of resection also is recommended for low-grade bone sarcomas, selected metastatic carcinomas, and, often, round cell sarcomas.
Type B resections, in which the abductors are resected, are extracompartmental resections and are the most common type of resection performed for high-grade spindle cell sarcomas.
All six of these types of shoulder girdle resections and their indications are described briefly in the following section. The surgical techniques for each resection and reconstruction are described in Chapters 9, 10, and 11,12 and 13 in this section.
GUIDELINES FOR SHOULDER GIRDLE RESECTION
Local Growth and Transarticular Involvement by Shoulder Girdle Tumors
The shoulder joint appears to be more prone than other joints to intra-articular or pericapsular (ligamentous) involvement by high-grade bone sarcomas.
Four basic mechanisms underlie tumor spread across the shoulder joint: direct capsular extension, tumor extension along the long head of the biceps tendon, fracture hematoma from a pathologic fracture, and poorly planned biopsy (FIG 3).
These mechanisms place patients undergoing intra-articular resections for high-grade sarcomas at greater risk for local recurrence than those undergoing extra-articular resections. Therefore, it often is necessary to perform an extra-articular resection for high-grade bone sarcomas of the proximal humerus or scapula.
Most tumors arise from the metaphyseal portion of the proximal humerus. They extend beyond the cortices and spread underneath the deltoid muscle, subscapularis muscle, and remaining rotator cuff muscles. As the tumor grows, the extraosseous component spreads along the long head of the biceps tendon, along the glenohumeral ligaments, and underneath the rotator cuff, heading toward the glenoid or directly crossing the glenohumeral joint. The deltoid, subscapularis, and remaining rotator cuff muscles are compressed into a pseudocapsular layer. These muscles form compartmental boundaries around the tumor. The axillary nerve and circumflex vessels enter this compartment. The major neurovascular bundle is displaced by the tumor; however, in most instances, the fascia overlying the subscapularis muscle as well as the axillary sheath that contains the blood vessels and nerves protect the major neurovascular bundle from tumor involvement or encasement.
Similarly, most scapular sarcomas originate from the metaphyseal portion of the scapula or the scapula neck and grow centripetally into the soft tissues. They form a soft tissue mass that extends outward and usually is contained by the subscapularis and other rotator cuff muscles. These tumors follow the path of least resistance and are directed toward the glenohumeral joint and proximal humerus. Eventually, the tumor contaminates these structures. The subscapularis muscle and its investing fascia function as a barrier and protect the axillary vessels and brachial plexus from tumor invasion. These neurovascular structures usually are displaced by the adjacent tumor that lies deep to the subscapularis muscle.
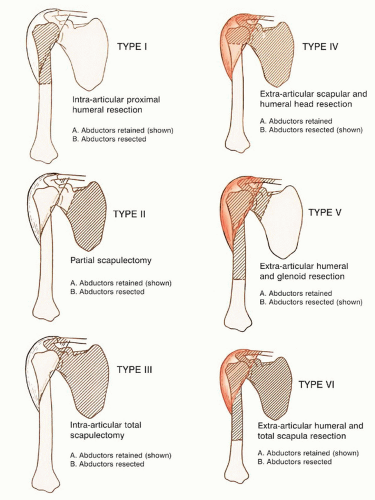 FIG 2 • Classification of shoulder girdle resections as reported by Malawer in 1991. (Reprinted with permission from Malawer MM, Meller I, Dunham WK. A new surgical classification system for shoulder-girdle resections. Analysis of 38 patients. Clin Orthop Relat Res 1991;267:33-44.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|