Overview of Nutrition Assessment in Clinical Care
1 Jefferson Medical College, Philadelphia, PA
2 City College of New York, New York, NY
3 The Permanente Medical Group, Oakland, CA
Nutrition Assessment in Clinical Care
Nutrition assessment is the evaluation of an individual’s nutritional status based on the interpretation of clinical information. Nutrition assessment is important because obesity and malnutrition are common in the clinical setting. The purpose of nutrition assessment is to:
- accurately evaluate an individual’s dietary intake and nutritional status,
- determine if medical nutrition therapy and/or counseling is needed,
- monitor changes in nutritional status, and
- evaluate the effectiveness of nutritional interventions.
Accurate nutritional assessment leads to correct diagnosis and treatment. Many patients can benefit from medical nutrition therapy (MNT) using established evidence-based protocols.
Integrating Nutrition into the Medical History and Physical Examination
The following illustrates how nutrition can be integrated into all components of the clinical assessment, including the medical history, diet history, review of systems, physical examination, laboratory data, and treatment plan.
Medical History
Past Medical History
Standard past medical history including immunizations, hospitalizations, surgeries, major injuries, chronic illnesses, and significant acute illnesses may have nutritional implications. Detailed information should be obtained about current or recent medication use including vitamins, minerals, laxatives, topical medications, over-the-counter medications, and products such as nutritional or herbal supplements which patients frequently fail to report as medications. Nutritional supplements include any products that may alter caloric, vitamin, or protein intake. Whether the patient has any known food allergies (i.e., peanut, gluten) or suffers from lactose (milk) intolerance is also important.
Family History
In assessing risk for future diseases, patients are asked to identify their parents, siblings, children, and partner, give their respective ages and health status, and indicate familial occurrences of disease or cause of death of any deceased family members. Family history of diabetes, cancer, heart disease, thyroid disease, obesity, hypertension, osteoporosis, food allergies, eating disorders, or alcoholism should be ascertained. Food sensitivity may be based on inherited immune system characteristics and family history of food intolerance should be assessed.
Social History
The diet history is typically obtained as part of the patients’ social history because socioeconomic factors such as who the patient lives with and what resources they have available influence food selection and preparation. Pertinent non-medical information recorded in the social history includes the patient’s occupation, daily exercise pattern, and marital and family status. Information should be solicited regarding the patient’s education, economic status, residence, emotional response and adjustment to illness, and any other information that might influence the patient’s understanding of his or her illness and adherence to a nutritional therapy. Details concerning the duration and frequency of the patient’s use of substances such as alcohol, tobacco, illicit drugs, and caffeine are also documented. These data can be extremely useful when formulating the treatment plan. Economic limitations that influence access to an adequate diet, difficulties shopping for or preparing food, participation in feeding programs (e.g. Women, Infants, and Children (WIC), Meals on Wheels) are relevant aspects of the nutritional assessment.
The Importance of Taking a Diet History
The purpose of obtaining dietary information from patients is to assess their nutritional intake and establish a baseline from which to negotiate changes. Infants, children, adolescents, pregnant women, older adults, and patients with a family history of or who have diabetes, hypertension, heart disease, hyperlipidemia, obesity, eating disorders, alcoholism, osteoporosis, gastrointestinal or renal disease, cancer, or weight loss or gain should consistently be asked about their eating habits, even during routine visits. Relative strengths for each method of collecting dietary information are described in this section. In addition, patients’ past and/or current dietary patterns, such as vegetarian or kosher diet practices, cultural background, and social situations should be considered during the interview. Family members who purchase and prepare foods should be invited for the interview process whenever possible. Diet-related questions may take a few minutes, if properly directed (See Table 1-1). Registered dietitians typically collect more detailed information from a diet history and make this information available to the physician, nurse practitioner, or physician assistant. This history may include information on food preferences, portion sizes, frequency of eating out, and emotional responses to eating. The detailed intake information can be used to determine calories, fat, protein, sodium, and fiber intake along with adequacy of vitamin and mineral intake can serve as a basis for counseling.
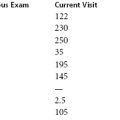
Table 1-1 Key Diet History Questions for Brief Intervention
Source: Lisa A. Hark, PhD, RD. 2014. Used with permission.
Questions for All Patients
|
| In addition to the questions above: Questions for Patients with Hyperlipidemia (Chapter 6)
|
Questions for Patients with Hypertension (Chapter 6)
|
Questions for Patients with Diabetes (Chapter 8)
|
24-Hour Recall
Purpose This informal, qualitative, questioning method elicits all foods and beverages the patient has consumed in the preceding 24 hours. This method is recommended for follow-up visits for patients with diabetes because of the ability to assess the timing of meals, snacks, and insulin injections.
Questions “Starting with the last thing you ate please describe everything that you ate or drank within the past 24 hours (meals and snacks), including quantities, and how you prepared these foods.” Family members are usually consulted if the patient is a child or unable to convey adequate detail. Patients can be asked to write down what they ate the day before while they are waiting to be seen. Hospitalized patients can be monitored through calorie counts reported by the nursing or dietary staff, who can record the daily amounts of food and drink the patient consumes. Keep in mind that the 24-hour recall method, when used alone, may underestimate or overestimate a person’s usual caloric intake because the patient’s recollection may not reflect long-term dietary habits. It may be helpful to add the question, “Is this fairly typical or was there something unusual about yesterday?” Use caution generalizing this information.
Usual Intake/Diet History
Purpose Similar to the 24-hour recall, a usual intake/diet history is a retrospective method to obtain dietary information by asking the patient to recall his or her normal daily intake pattern, including amounts of foods consumed. This method is suggested for older adults who may frequently skip meals, or for interviewing pediatric patients whose diets may not be varied. This approach provides more information about usual intake patterns than others and tends to reflect long-term dietary habits with greater accuracy.
Questions “Please tell me what you usually eat and drink during the day for meals and snacks?” As a busy clinician, this question may be all that you will have time to ask, but it can serve as a screening mechanism to identify patients who need further screening with a registered dietitian. When using this approach it is important to be flexible. Begin by asking patients to describe their usual intake and if they cannot recall their usual diet, ask what they ate and drank the day before (a switch to the 24-hour recall method). You can then ask if these 24 hours are typical. Also bear in mind that some patients tend to report having eaten only those foods that they know are healthy. It is also important to ask patients if they have changed their diet for health reasons or because of a health professional’s advice.
Food Frequency Questionnaire
Purpose The food frequency questionnaire is another retrospective approach used to determine trends in a patient’s usual consumption of specific foods.
Questions Patients are usually asked several key questions regarding the frequency of intake of particular foods. Frequencies have been created to identify daily, weekly, or monthly consumption patterns and are especially good for specific nutrients (e.g., fiber, iron, or saturated fat). Patients can be asked these questions during the history, or these items can be added to the written form for new patients that can be mailed to them prior to their visit or completed while they are in the waiting room. For the clinician, questions can be geared toward the patient’s existing medical conditions, which is why this method is effective for patients with diabetes, heart disease, hypertension, or osteoporosis and can be used for evaluating current intake of, for example, fruits, vegetables, dairy products, or processed foods.
Three-Day Food Record
Purpose Unlike the retrospective tools mentioned earlier, a food record is ideally completed prospectively and daily as patients consume their usual diet and reviewed by the clinician at the medical visit. More accurate results can be obtained by collecting data over a longer period (e.g., 7 days).
Questions Patients are asked to record information on meals, food items, quantity consumed, preparation methods, etc., and details such as activities while eating, mood, hunger level, etc., can also collected. This method is preferred for active patients who may be trying to adhere to a new dietary regimen (e.g., a weight loss diet). Three-day records are the most accurate reflection of patients’ diets but it is difficult for most patients to keep a written log, including portion sizes, of everthing they ate and drank over three days.
Review of Systems
This subjective reexamination of the patient’s history is organized by body systems. It differs from the past medical history by concentrating on symptoms, not diagnoses, and by emphasizing current more than past information. All positive and negative findings are listed. Nutrition questions vary according to the patient’s age. One goal of this part of the history is to determine whether any dietary changes have occurred in the patient’s life, either voluntarily or as a consequence of illness, medication use, or psychological problems. Examples within the review of systems that may have nutritional implications (and their potential significance) include weakness and fatigue (anemia), clothes tighter or looser (weight gain or weight loss), post-meal cramping or diarrhea (lactose intolerance), chronic headaches, fatigue, gastrointestinal symptoms (gluten sensitivity), constipation (low fluid or fiber intake), amenorrhea (anorexia nervosa), or changes in appetite.
Physical Examination
The physical examination begins with the patient’s vital signs (blood pressure, heart rate, respiration rate, temperature), height, weight, body mass index (BMI), and general appearance. For example, “On examination, she is a well-developed, athletic woman.” When terms such as obese, overweight, undernourished, thin, well-nourished, well-developed, or cachectic (profound, marked state of ill health and malnutrition) are used, they should be supported by findings in the physical examination and noted in the problem list.
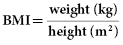
Body Mass Index (BMI)
To calculate BMI using the metric system:
To calculate BMI using English units:
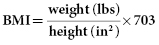
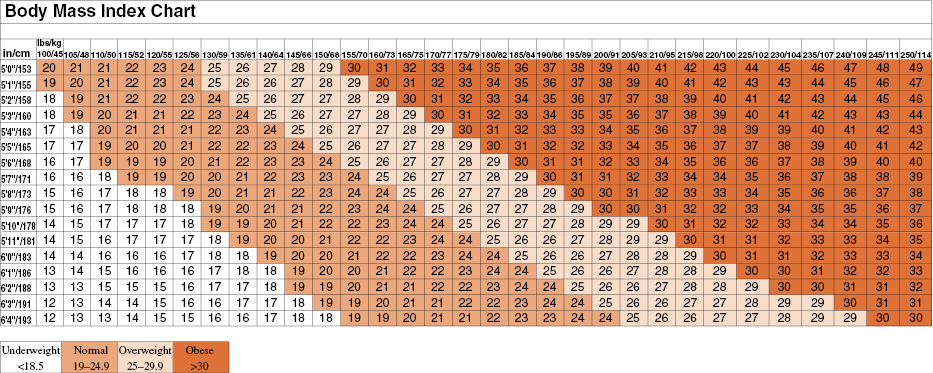
Body mass index provides a more accurate measure of total body fat (adiposity) than body weight alone. The BMI is also more accurate than the older height–weight tables, which were based on a homogeneous population, primarily Caucasian, with higher than average socioeconomic status. BMI has also been shown to more estimate obesity than bioelectrical impedance tests. BMI values associated with the lowest mortality increase slightly as people age. However, BMI may overestimate body fat in very muscular people and underestimate body fat in some underweight people who have lost lean tissue, such as the elderly. Classifications of underweight, normal weight, overweight, and obesity are shown in Table 1-2. Health professionals should routinely assess height, weight, and BMI, and evaluate growth and development in infants, children, and adolescents.
Table 1-2 Classifications of BMI
Source: National Heart, Lung, and Blood Institute, NIH. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. 1998. Used with permission.
| Underweight | <18.5 kg/m2 |
| Normal weight | 18.5–24.9 kg/m2 |
| Overweight | 25–29.9 kg/m2 |
| Obesity (Class 1) | 30–34.9 kg/m2 |
| Obesity (Class 2) | 35–39.9 kg/m2 |
| Extreme obesity (Class 3) | ≥40 kg/m2 |
Diagnosis and Assessment of Overweight and Obesity
Body Mass Index (BMI)
According to the National Heart Lung and Blood Institute’s (NHLBI) Clinical Guidelines, many people with a BMI of 25 kg/m2 or greater begin to experience negative health effects, such as elevated low-density lipoprotein cholesterol (LDL-C) and total cholesterol levels, high blood pressure, and glucose intolerance. These guidelines define overweight individuals as those with a BMI of 25 to 29.9 kg/m2 and obese individuals as those with a BMI of 30 kg/m2 and above. The NHLBI Clinical Guidelines classify BMI as shown in Table 1-2. BMI values can be determined from height and weight measurements as shown in Figure 1-1.
Waist Circumference
Waist circumference is an independent measure of risk in normal weight and overweight individuals. Excess fat located in the abdominal area (termed visceral adipose tissue) is reflected by waist circumference measurement. Waist circumference is a predictor of morbidity, and is considered an independent risk factor for diabetes, dyslipidemia, hypertension, and cardiovascular disease when BMI is not markedly increased. In patients with a BMI greater than 35 kg/m2, there is little additional risk from elevated waist circumference, as severe risk is already present. Therefore, measuring waist circumference is recommended in patients with a BMI less than 35 kg/m2. The waist circumference measurement is particularly important for patients with a family history of diabetes and those who may be borderline overweight.
In order to obtain an accurate waist circumference measurement, patients should be standing in only their underwear. A horizontal mark should be drawn just above the uppermost lateral border of the right iliac crest, which should then be crossed with a vertical mark in the midaxillary line. The measuring tape is placed in a horizontal plane around the abdomen at the level of this mark on the right side of the trunk. The plane of the tape should be parallel to the floor and the tape should be snug but not tight. Patients should be advised to breathe normally while the measurement is taken. Waist circumference values greater than 102 cm (40 inches) in men and greater than 88 cm (35 inches) in women are considered indicators of increased risk, although these values may differ for different ethnic groups. Waist circumference is one of the diagnostic criteria of metabolic syndrome (Chapter 1: Case 1). In patients trying to lose weight by exercising, waist circumference may decrease without significant weight loss.
Percent Weight Change
Weight loss is very common in hospitalized patients and those residing in chronic care facilities. Weight loss is also frequently seen in older adults or those with decreased changes due to chronic illnesses such as cancer, gastrointestinal problems, or secondary to surgery, chemotherapy, or radiation therapy. If weight loss is identified in the medical history or review of systems, it is essential to take a diet and weight history and determine the percent weight change over that period of time using the patient’s current body weight and usual weight. Severity of weight loss is defined by percent change in a defined period of time (Table 1-3).
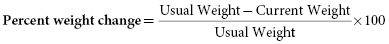
Table 1-3 Interpretation of Percent Weight Change
| Time | Significant Weight Loss | Severe Weight Loss |
|---|---|---|
| 1 week | 1–2% | >2% |
| 1 month | 5% | >5% |
| 3 months | 7.5% | >7.5% |
| 6 months | 10% | >10% |
| 1 year | 20% | >20% |
Physical Examination Findings
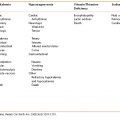
Nutrition-oriented aspects of the physical examination focus on the skin, hair, eyes, mouth, nails, extremities, abdomen, skeletal muscle, and fat stores. Areas to examine closely for muscle wasting include the temporalis muscles, thenar, hypothenar, and interosseous muscles on the hands. The skeletal muscles of the extremities are a less sensitive indicator of malnutrition. Subcutaneous fat stores should be examined for losses due to a sudden decrease in weight or for excess accumulation in obesity. Isolated vitamin deficiencies such as scurvy or pellagra are rarely seen in modern clinical practice. At the present time, the most commonly encountered nutritional problem seen in clinical practices in the United States and many developed countries is obesity and its associated complications. Specific clinical signs that are attributable to nutrient deficiencies and significance on physical examination are shown in Table 1-4. Combined nutrient deficiencies are still seen in those with disordered intake such as alcoholics or patients receiving chemotherapy.
Table 1-4 Physical Examination Findings with Nutritional Implications
Source: Lisa A. Hark, PhD, RD and Darwin Deen, MD, MS. 2014. Used with permission.
| Exam | Nutritional implications |
|---|---|
| Vital signs | Blood pressure, height, weight, BMI, percent weight change |
| General | Wasted, cachectic, overweight, obese, muscle weakness, anorexic, waist circumference |
| Skin | Acanthosis nigricans (obesity, metabolic syndrome, insulin resistance, diabetes) |
| Ecchymosis (vitamin K, C deficiency) | |
| Dermatitis (marasmus, niacin, riboflavin, zinc, biotin, EFA deficiency) | |
| Follicular hyperkeratosis (vitamin A deficiency) | |
| Petechiae (vitamin A, C, K deficiency) | |
| Pigmentation changes (niacin deficiency, marasmus) | |
| Pressure ulcers/delayed wound healing (kwashiorkor, diabetes, vitamin C, zinc deficiency) | |
| Psoriasiform rash, eczematous scaling (zinc deficiency) | |
| Purpura (vitamin C, K deficiency) | |
| Scrotal dermatosis (riboflavin deficiency) | |
| Pallor (iron, folic acid, vitamin B12, copper, vitamin e deficiency) | |
| Thickening and dryness of skin (linoleic acid deficiency) | |
| Hair | Dyspigmentation, easy pluckability (protein), alopecia (zinc, biotin deficiency) |
| Head | Temporal muscle wasting (marasmus and cachexia) |
| Delayed closure of fontanelle (pediatric undernutrition or growth retardation) | |
| Eyes | Night blindness, xerosis, bitot spots, keratomalacia (vitamin A deficiency) |
| Photophobia, blurring, conjunctival inflammation, corneal vascularization (riboflavin deficiency), macular degeneration | |
| Mouth | Angular stomatitis (riboflavin, iron deficiency) |
| Bleeding gums (vitamin C, K, riboflavin deficiency) | |
| Cheilosis (riboflavin, niacin, vitamin B6 deficiency) | |
| Dental caries (fluoride deficiency) | |
| Hypogeusia (zinc, vitamin A deficiency) | |
| Glossitis (riboflavin, niacin, folic acid, vitamin B12, vitamin B6 deficiency) | |
| Nasolabial seborrhea (vitamin B6 deficiency) | |
| Papillary atrophy or smooth tongue (riboflavin, niacin, iron deficiency) | |
| Fissuring, scarlet or raw tongue (niacin, folate, B12, B6 deficiency) | |
| Neck | Goiter (iodine deficiency) |
| Parotid enlargement (marasmus, bulimia) | |
| Thorax | Thoracic achitic rosary (vitamin D deficiency) |
| Abdomen | Abdominal obesity (metabolic syndrome, diabetes, heart disease) |
| Diarrhea (niacin, folate, vitamin B12 deficiency, marasmus) | |
| Hepatomegaly/ascites (kwashiorkor, alcoholism) | |
| Cardiac | Heart failure (thiamin, selenium deficiency, anemia) |
| Genital/urinary | Delayed puberty (marasmus, eating disorder, celiac disease) |
| Hypogonadism (zinc deficiency) | |
| Extremities | Ataxia (vitamin B12 deficiency, vitamin B6 toxicity) |
| Bone ache, joint pain (vitamin C deficiency) | |
| Bone tenderness, kyphosis (vitamin D deficiency) | |
| Edema (thiamin or protein deficiency) | |
| Growth retardation, failure to thrive (energy deficiency) | |
| Hyporeflexia (thiamin deficiency) | |
| Bone tenderness, kyphosis (calcium, vitamin D deficiency) | |
| Muscle wasting and weakness (vitamin D, magnesium deficiency, marasmus) | |
| Tenderness at end of long bones (vitamin D deficiency) | |
| Squaring of shoulders—loss of deltoid muscles (kwashiorkor) | |
| Nails | Spooning (koilonychias) (iron deficiency) |
| Transverse lines (kwashiorkor, hypochacemia) | |
| Neurological | Dementia, delirium, disorientation (niacin, thiamin, vitamin E deficiency) |
| Loss of reflexes, wrist drop, foot drop (thiamin deficiency) | |
| Ophthalmoplegia (vitamin E, thiamin deficiency) | |
| Peripheral neuropathy (thiamin, vitamin E, vitamin B12 deficiency) | |
| Tetany (vitamin D, calcium, magnesium deficiency) |
Laboratory Data Used to Diagnose Nutritional and Medical Problems
No single blood test or group of tests accurately measures nutritional status. Therefore clinical judgment is important in deciding what tests to order based on the individual’s history and physical findings. The following tests are grouped according to medical condition.
- Alcoholism: Aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), thiamin, folate, and vitamin B12.
- Anemia: Complete blood count (CBC), serum iron and ferritin, total iron binding capacity (TIBC), transferrin saturation, mean corpuscular volume (MCV), reticulocyte count, red blood cell folate, and serum vitamin B12.
- Diabetes: Fasting serum glucose, hemoglobin A1C, insulin levels, C-reactive protein (CRP), serum, and urinary ketone bodies.
- Eating Disorders: Potassium, albumin, serum amylase, thyroid studies, beta carotene aspartate amino transferase (AST), alanine aminotransferase (ALT), and anemia.
- Fluid, Electrolyte, and Renal Function: Sodium, potassium, chloride, calcium, phosphorus, magnesium, blood urea nitrogen (BUN), creatinine, urine urea nitrogen, urinary and serum, oxalic acid, and uric acid.
- Hyperlipidemia: Cholesterol, triglyceride, low density lipoprotein-cholesterol (LDL-C), high density lipoprotein-cholesterol (HDL-C), LPa, homocysteine, and thyroid stimulating hormone (TSH) (secondary cause).
- Musculoskeletal pain, weakness: 25(OH) vitamin D, phosphate, parathyroid hormone (PTH).
- Malabsorption: 24-hour fecal fat, barium imaging studies, electrolytes, albumin, serum triglycerides, and hydrogen breath test.
- Metabolic Syndrome: Fasting serum glucose, lipid panel, and uric acid.
- Refeeding Syndrome: Albumin, calcium, phosphorous, magnesium, and potassium.
Malnutrition: Protein Status
Clinically, visceral protein status may be depleted by increased protein losses in the stool and urine as a result of wounds involving severe blood loss, or by poor dietary protein intake. The following serum protein levels may prove useful in conjunction with other nutrition assessment parameters. Once again, however, each of these tests has limitations because serum protein levels are affected not only by nutrition and hydration status, but by disease states, surgery, and liver dysfunction.
The half-life (t1/2) of each protein is given because it allows use of these tests to monitor changes in protein nutrition over time:
- Serum albumin Serum albumin has a half-life of 18 to 20 days and reflects nutritional status over the previous 1 to 2 months. Levels may decrease with acute stress, overhydration, trauma, surgery, liver disease, and renal disease. False increases occur with dehydration. This test is not a good indicator of recent dietary status or acute changes in nutritional status (less than 3 weeks) given its long half-life. Significantly reduced levels of serum albumin (<3.5 mg/dL) have been associated with increased morbidity and mortality in clinical studies.
- Serum transferrin Serum transferrin has a half-life of 8 to 9 days. Changes in serum transferrin levels are influenced by iron status, as well as by protein and calorie malnutrition. Results of this test reflect intake over the preceding several weeks.
- Serum prealbumin With a half-life of 2 to 3 days, serum prealbumin reflects nutritional status as well as protein and calorie intake over the previous week. Prealbumin levels may be falsely elevated with renal disease or, as with albumin, reduced with severe liver disease.
Assessment and Problem List: Medical Nutrition Therapy
The healthcare professional clinically assesses the individual patient based on his/her history, review of systems, physical examination, and laboratory data.
Active problems are listed in order of their importance. Inactive problems are also recorded. Evidence of a nutrition disorder should be considered primary if it occurs in patients with no other etiology that explains signs and symptoms of malnutrition. A primary nutrition problem is usually the result of imbalances, inadequacies, or excesses in the patient’s nutrient intake. Manifestations may include obesity, weight loss, malnutrition, or poor intake of vitamins or minerals such as iron, calcium, folate, vitamin D, or vitamin B12.
Patients having normal weight and no other risk factors should be encouraged to maintain their weight. Overweight patients with co-morbidities, such as diabetes, hypertension, or heart disease, should be advised to lose weight by increasing their physical activity level and reducing their total calorie and saturated fat intake, using smaller portion sizes, and selecting healthier foods. Referral to a registered dietitian for additional counseling and support has been shown to be effective.
Secondary nutrition problems occur when a primary pathologic process results in inadequate food intake, impaired absorption and utilization of nutrients, increased loss or excretion of nutrients, or increased nutrient requirements. Common causes of secondary nutritional disorders include anorexia nervosa, malabsorption, trauma, acute medical illness, and surgery. Malnutrition may occur as a result of a chronic condition or an acute episode complicating an underlying disease. After assessing each problem, medical nutrition therapy should be recommended that includes both a diagnostic component and a treatment plan. Patient education is an essential part of medical nutrition therapy. Key dietary issues by age and disease are summarized in Table 1-5.
Table 1-5 Key Dietary Issues by Age and Disease
Source: Lisa A. Hark, PhD, RD and Darwin Deen, MD, MS. 2014. Used with permission.
| Age/Disease | Key Dietary Issue |
|---|---|
| Infants | Fluoride, iron, calories, protein, fat for growth and development |
| Children | Fluoride, iron, calcium, calories, protein, fat for growth and development |
| Teenagers | Iron, calcium, calories, protein for pubertal development (screen for eating disorders) |
| Pregnancy | Folate, iron, calcium, vitamin D, protein, appropriate weight gain |
| Alcoholism | Folate, thiamin, vitamin B12, calories |
| Anemia | Iron, vitamin B12, folate |
| Ascites | Sodium, protein |
| Beriberi | Thiamin |
| Cancer | Adequate protein, calories, and fiber |
| Celiac Disease | B complex, vitamins, vitamin D |
| COPD, Asthma | Vitamin D, calcium, weight loss, calories |
| Diabetes | Carbohydrates, saturated fat, cholesterol, calories, fiber |
| Heart Disease | Saturated fat, monounsaturated fat, cholesterol, sugar, fiber |
| Hyperlipidemia | Saturated fat, monounsaturated fat, cholesterol, sugar, fiber |
| Heart Failure | Sodium |
| Hypertension | Sodium, calcium, potassium, alcohol, sugar, total calories |
| Kidney Stones | Calcium, oxalate, uric acid, protein, sodium, fluid |
| Liver Disease | Protein, sodium, fluid |
| Malabsorption | Vitamins A, D, E and K |
| Obesity | Total calories, portion sizes, saturated fat |
| Osteoporosis | Vitamin D and calcium |
| Pellegra | Niacin |
| Renal Failure | Protein, sodium, potassium, phosphorous, fluid |
| Rickets | Vitamin D and calcium |
| Scurvy | Vitamin C |
| Vegetarian diet | Protein, vitamin B12, iron, calcium |
Estimating Energy and Protein Requirements
Resting Energy Expenditure (REE)
The amount of energy required to maintain vital organ function in a resting state over 24 hours is referred to as the resting energy expenditure (REE). Basal metabolic rate (BMR) is the minimum calorie requirement for an individual at a neutral environmental temperature while fasting. BMR is generally impractical to measure. REE is approximately 10 percent above BMR. Thus, the REE is used clinically for estimation of BMR. REE accounts for approximately 65 percent of total daily energy expenditure and varies considerably among individuals with different height, weight, age, body composition, and gender. REE significantly correlates with lean body mass. Regular physical activity, especially weight-bearing exercises, can increase muscle mass, and thus increase REE. Since REE decreases as people age due to the loss of lean body mass over time, regular exercise can play a significant role in maintaining REE, especially in older adults. The energy produced by the oxidation of dietary macronutrients is shown in Table 1-6. The Mifflin–St. Jeor equation to estimate energy requirement is shown in Table 1-7. Activity factors are added to the REE as necessary to calculate total daily caloric needs, which vary for active and inactive patients. Total energy expenditure (TEE) is equal to the REE times the appropriate physical activity factor. The physical activity factor for hospitalized patients or those confined to bed is 1.2; for non-hospitalized, sedentary patients, 1.3.
Table 1-6 Definition of Energy/Calorie
| Energy is expressed in kilocalories (kcal) and is produced by the oxidation of dietary protein, fat, carbohydrate, and alcohol. |
|
| A calorie is the amount of heat required to raise the temperature of 1 gram of water by 1 degree Celsius. A kilocalorie is the amount of heat required to raise the temperature of 1 kilogram of water by 1 degree Celsius. |
Table 1-7 Mifflin-St. Jeor Equation to Estimate Energy Requirement
Source: Mifflin, MD, St. Jeor ST, Hill LA, Scott, BJ, Daughtery SA, Koh YO. A new perspective equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;(2):1241–-1247.
| Adults 19 years and older |
|---|
| Estimated Energy Requirement (kcal/day) = Total Energy Expenditure Men 10 × weight (kg) + 6.25 × height (cm) − 5 × age (y) + 5 Women 10 × weight (kg) + 6.25 × height (cm) − 5 × age (y) − 161 |
Protein Needs of Hospitalized or Critically Ill Patients
Protein requirements in a critically ill patient depend on the degree of catabolic stress the patient is experiencing. Guidelines are as follows:
- In unstressed well-nourished individuals, protein needs range from 0.8 to 1.0 g/kg body weight per day.
- In post-surgical patients protein needs range from 1.5 to 2.0 g/kg body weight per day.
- In highly catabolic patients (burns, infection, fever), protein needs can be over 2 g/kg body weight per day.
Malnutrition
According to the World Health Organization (WHO), malnutrition affects all age groups across the entire lifespan, from conception to older adults. Health consequences range from intrauterine brain damage and growth failure to reduced physical and mental capacity in childhood to an increased risk of developing diet-related chronic diseases later in life.
Insufficient food intake results in loss of fat, muscle, and ultimately visceral tissue. This reduction in tissue mass is reflected in weight loss. The smaller tissue mass reduces nutritional requirements, likely reflecting more efficient utilization of ingested food and reduction in work capacity at the cellular level. The combination of decreased tissue mass and reduction in work capacity impedes homeostatic responses, including responses to illness or surgery. The stress of critical illness inhibits the body’s conservation response to malnutrition. In addition, undernourished individuals experience nutrient deficiencies and imbalances that exacerbate the reduction in cellular work capacity. Malnutrition is also associated with a decrease in the inflammatory response and immune function. These alterations result in increased morbidity and mortality among undernourished patients. Adequate nutrition is essential for reversing these physiological effects. Aggressive nutritional support, instituted early in critical illness, may reduce the adverse effects of malnutrition in the critically ill patient.
Etiology/Causes of Malnutrition
Decreased Oral Intake Poverty, poor dentition, gastrointestinal obstruction, abdominal pain, anorexia, dysphagia, depression, social isolation, and chronic pain are some of the many possible causes of decreased oral intake.
Increased Nutrient Loss Glycosuria, proteinuria, gastrointestinal bleeding, diarrhea, malabsorption, a draining fistula, or protein-losing enteropathy can result in nutrient losses.
Increased Nutrient Requirements Hypermetabolism state or excessive catabolic processes can result in increased nutrient requirements. Common examples of situations that can dramatically affect nutrient requirements include surgery, trauma, fever, burns, hyperthyroidism, severe infection, malabsorption syndromes, cancer, chronic obstructive pulmonary disease (COPD), cardiac cachexia, critical illness, and HIV/AIDS. Pregnant women and children also experience increased nutritional requirements during growth and development.
Diagnosis of Malnutrition
Malnutrition is defined as a suboptimal or deficient supply of nutrients that interferes with an individual’s growth, development, general health, or recovery from illness. A BMI of less than 18.5 kg/m2 defines adults who are consistently underweight and at risk for malnutrition. Infants and children who fall below the 5th percentile for weight-for-age or BMI-for-age on the growth chart should also be evaluated further and followed closely. In acute malnutrition, a child’s weight-for-age percentile on the growth chart falls first, followed by a decline in height growth. In extreme cases of malnutrition or starvation, a child’s head circumference growth may also plateau. The importance of plotting pediatric growth parameters over time is paramount, as poor weight gain and/or weight loss are key to diagnosing malnutrition, failure to thrive, and other medical conditions associated with poor weight gain in the pediatric population, such as cystic fibrosis. Crossing growth percentile lines should always prompt close follow-up.
Marasmus results when the body’s requirements for calories and protein are not met by dietary intake. Marasmus is characterized by severe tissue wasting, excessive loss of lean body mass and subcutaneous fat stores, and weight loss. Decreased protein intake is usually associated with decreased calorie intake, but can occur independently.
Kwashiorkor describes a predominant protein deficiency. Kwashiorkor is characterized by lethargy, apathy, irritability, retarded growth, changes in skin (dermatitis) and hair pigmentation, edema, and low serum albumin. Both marasmus and kwashiorkor are associated with weakness, weight loss, decline in functional status (increased difficulties with activities of daily living), impaired immune function with increased susceptibility to infection, and increased risk of morbidity and mortality.
Prevalence of Malnutrition
Children, older adults, and hospitalized and nursing home patients are particularly prone to malnutrition. According to WHO, 99 million children (17 percent) under 5 years of age were underweight in developing countries in 2011. This number is estimated to have declined from 28 percent in 1990. Fifty percent of deaths among children less than 5 years of age in developing countries are associated with malnutrition. One in three people are affected by vitamin and mineral deficiencies and one in four pre-school children suffer from malnutrition. One in six infants are born at low birth weight in developing countries.
Some degree of malnutrition occurs during most hospitalizations regardless of the type of injury or illness. The prevalence of malnutrition in the out-patient population has not been clearly determined. Risk factors for malnutrition include chronic diseases, use of multiple prescription medications, poverty, inadequate nutritional knowledge, homebound and/or non-ambulatory status, poor social support structure, major psychiatric diagnosis, and alcoholism. Malnutrition in nursing home patients has been reported in up to 50 percent of residents.
Food insecurity is defined by the United States Department of Agriculture (USDA) as lack of access to enough food to fully meet basic needs at all times due to lack of financial resources. Households that are insecure, even when hunger is not present, have such limited resources that they may run out of food or cannot afford balanced meals. Hungry households have been defined as those that lack adequate financial resources to the point where family members, especially children, are hungry on a regular basis and the food intake of adults is severely reduced.
According to the USDA, an estimated 17 million (15 percent) of American households experienced food insecurity for at least some time during 2011. This represented 33.5 million adults and 16.7 million children. Approximately 8.6 million children (11.5 percent) lived in households in which one or more child was food insecure. Nationally, food insecurity was significantly higher for households with incomes near or below the Federal poverty line (35 percent), households headed by a single woman (37 percent) or man (24.9 percent), Black, non-Hispanic (25 percent) and Hispanic (26.2 percent) households, all households with children (21 percent) and households with children under age 6 (22 percent). Households with WIC-eligible incomes experience food insecurity more than those with higher income levels. Studies have shown that the federally funded WIC program is an effective means of decreasing rates of food insecurity while positively influencing nutrient intakes.
Unfortunately, with the shift from welfare to work, many low-income working families who are eligible for Federal assistance do not participate, leaving children more vulnerable to food insecurity than ever before. In 2011, 57 percent of food insecure households received assistance from one or more of the three largest Federal food and nutrition assistance programs. The Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program, provided benefits to 44.7 million people in the UnitedStates in 2011. This accounted for 40.1 percent of food insecure households.
Food insecurity and poor diet quality exist at unsettling levels throughout the United States despite attempts to create a food and nutrition safety net. Studies show that specific populations, including low-income women with children living in rural areas, are at increased risk for experiencing food insecurity. Providing nutrition education to all food assistance program participants, including information regarding the benefits associated with the recommended intake of fruits and vegetables as well as the availability and affordability of fresh produce, should be a priority.
Overweight and Obesity
Health Consequences of Overweight and Obesity
Obesity is a complex, multi-factorial disease that is becoming increasingly common among adults and children worldwide. Once considered a problem only in developed countries, overweight and obesity are now dramatically on the rise in developing countries as well, particularly in urban settings. Obese individuals have an increased risk of diabetes, coronary heart disease, hyperlipidemia, hypertension, stroke, gallbladder disease, sleep apnea, osteoarthritis, respiratory problems, and certain types of cancers (endometrial, breast, prostate, and colon), all of which increase their risk of mortality. According to the Centers for Disease Control and Prevention (CDC), seven out of ten deaths among Americans each year result from chronic diseases. Obesity-related conditions such as heart disease, type 2 diabetes, stroke, and certain types of cancer account for more than 50 percent of preventable deaths each year.
Recent studies show that overweight (BMI = 25.0–29.9) or class I obesity (BMI = 30.0–34.9) are not associated with excess mortality compared to normal BMI individuals (BMI = 18.5–24.9). However, class II/III obesity (BMI ≥ 35.0) is associated with significantly higher mortality, ranging from 40 percent among females to 62 percent among males relative to individuals with normal BMI. In considering attributable mortality risk, class II/III obesity (BMI ≥ 35.0) is responsible for approximately 4 percent of deaths among females and 3 percent among males. Obesity accounts for approximately 5 to 7 percent of national health expenditures in the United States. Recent studies demonstrate that across all payers, public and private, per capita medical spending for the obese was $1,723 higher per year (42 percent) than for an individual of normal weight and $266 higher per year for overweight individuals. The aggregate national cost of overweight and obesity was approximately $114 billion dollars in 2012. Other studies indicate that obesity-related expenditures are expected to increase to 16 to 18 percent of healthcare spending by 2030.
Etiology of Overweight and Obesity
The etiology of obesity is believed to be due to a combination of biological and environmental factors. Biological factors that have been identified include an individual’s genetic predisposition, the size and number of adipose cells, and REE. Environmental factors that have been identified as contributory to overweight and obesity include excessive caloric intake and inadequate physical activity. These are the most likely environmental factors associated with the significant increase in overweight and obesity seen in the United States. and developed countries over the past several decades. Recent research is examining the role of exposure to environmental toxins and the contribution of gut bacteria.
Genetics In humans, 426 variants of 127 different genes have been associated with obesity. According to the Human Obesity Gene Map, single mutations in 11 genes were strongly implicated in 176 cases of obesity worldwide. Additionally, 50 chromosomal locations have been mapped that contain genes that may be related to obesity. According to the CDC, “several independent population-based studies reported that a gene of unknown function, referred to as fat mass and obesity-associated gene (FTO), may be responsible for up to 22 percent of all cases of obesity. Interestingly, the FTO gene also shows a strong association with diabetes. The mechanism by which FTO operates is currently under investigation.”
Family history reflects genetic susceptibility and environmental exposures shared by close relatives. Genetic studies over the past several decades investigating adopted twins and their biological and adoptive parents show that adoptees’ weight correlates most strongly with their biological parents’ weight. Additional research has shown that children with one overweight parent have a 40 percent chance of becoming overweight as adults. This risk increases to 80 percent if both parents are overweight. Regardless of the strong evidence for genetic influences on human obesity, genetics accounts for no more than one-third of the variance in body weight. Experts agree that since there has been no change in the gene pool over the past three decades, the dramatic increase in the prevalence of obesity in both children and adults in the United States. likely reflects environmental influences (epigenetic).
Adipose Cell Size and Number The size and number of fat cells have been studied for many years and vary between normal, overweight, and obese individuals. During infancy, adolescence, and pregnancy, fat cells normally increase in number. With modest weight gain, fat cells increase in size, and with significant weight gain, fat cells increase in both size and number. With weight loss, fat cells decrease in size but not in number. The lack of reduction in fat cell number may help explain why it is difficult for obese individuals to maintain weight loss for an extended period of time after a significant weight loss.
Excess Caloric or Energy Intake
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree