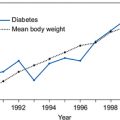
The controversy continues as not all studies have replicated the findings of ACCORD, ADVANCE and VADT. The UKPDS-80 trial, a follow-up of the original UKPDS, found that intensive glycaemic control was beneficial when initiated in newly diagnosed patients, with a continued reduction in risk of microvascular complications and reductions in risk for myocardial infarction and death from any cause that emerged during 10 years of post-trial follow-up (Holman et al., 2008). Contrasting findings have also been reported in a recent meta-analysis of five large randomized clinical trials, including UKPDS, ADVANCE, VADT, ACCORD, and the PROspective pioglitAzone Clinical Trial in macroVascular Events (PROactive) (Ray et al., 2009). Although there was no effect on stroke or all-cause mortality, a 17% reduction in myocardial infarction and a 15% reduction in the risk of coronary heart disease events were reported.
Current consensus on glycaemic control targets
The general consensus is that the ACCORD findings should not deter healthcare providers from helping patients achieve recommended glycaemic targets (Skyler et al., 2009). Rather, the results further illustrate the need to tailor HbA1c targets and treatments to individual patients. The ACCORD results show that intensive treatment of hyperglycaemia may not be beneficial in high-risk patients with a long history of type 2 diabetes. Long-term UKPDS results show there are benefits of intensive care at an early stage of the disease. The potential risks of intensive glycaemic control may therefore outweigh its benefits in some patients, such as those with a very long duration of diabetes, known history of severe hypoglycaemia, advanced atherosclerosis, and advanced age/frailty. NICE cautions against intensive efforts to get below current treatment targets recognizing that successful control of diabetes cannot be measured by setting HbA1c targets that are independent of the patient and their personal health factors and lifestyle.
Pros and cons of existing non-insulin antidiabetes therapies
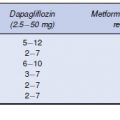
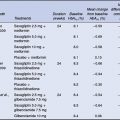
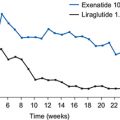
Despite the value of diet and lifestyle measures, most patients with type 2 diabetes will also require pharmacotherapy to achieve glycaemic goals. There are now eight classes of non-insulin antidiabetes therapies for treating type 2 diabetes (metformin, sulphonylureas, meglitinides, thiazolidinediones, alpha-glucosidase inhibitors, amylin analogues, glucagon-like peptide-1 (GLP-1) receptor agonists, and dipeptidyl peptidase 4 (DPP-4) inhibitors. These agents act at different sites in the body to improve insulin secretion or improve insulin action (Table 2.1). Antidiabetes agents can be used alone or in combination to provide therapy for type 2 diabetes. A number of factors need to be considered when deciding on the choice of drug or drug combination to use in an individual (Table 2.2).
Table 2.1 Classes of non-insulin antidiabetes therapies for the treatment of type 2 diabetes
| Antidiabetes therapy | Primarymechanism ofaction |
| Metformin | Inhibition of hepatic gluconeogenesis and increase in hepatic insulin sensitivity |
| Sulphonylureas | Stimulation of insulin secretion |
| Meglitinides | Stimulation of insulin secretion |
| Thiazolidinediones | Increase in muscle, liver and adipose tissue insulin sensitivity |
| Alpha-glucosidase inhibitors | Delay in glucose absorption |
| Amylin analogue | Inhibition of gastric emptying and glucagon release, reduces food intake |
| GLP-1 receptor agonists | Stimulation of glucose-dependent insulin secretion and inhibition of glucagon release |
| DPP-4 inhibitors | Stimulation of glucose-dependent insulin secretion and inhibition of glucagon release via increase in endogenous GLP-1 |
Metformin
Metformin is recognized as the first-line treatment for type 2 diabetes in patients not achieving adequate glycaemic control with diet and lifestyle interventions, particularly in individuals who are overweight, and can also be prescribed as adjunct therapy to virtually every other antidiabetes agent currently available (Nathan et al., 2006; NICE 2008; NICE, 2009). Metformin has no direct effects on beta cells, but reduces blood glucose levels by suppressing hepatic glucose production, increasing the sensitivity of muscle cells to insulin, and decreasing absorption of glucose from the gastrointestinal tract (Strack, 2008).
Table 2.2 Factors influencing target HbA1c goal and choice of antidiabetes therapy
| • Severity of hyperglycaemia |
| • Risk of hypoglycaemia |
| • Weight/body mass index |
| • Stage of disease – recently diagnosed – long duration |
| • Cardiovascular risk profile |
| • Medical conditions – renal function – oedema – heart failure – osteoporosis |
| • Medication side-effects |
| • Occupation – driving/flying/working at heights |
| • Practical issues – eyesight/manual dexterity/cognitive function – likely adherence to frequency of dosing |
| • Patient preference |
| • Social e.g. patient living alone |
| Benefits | Disadvantages |
| • HbA1c reductions of up to 1.5% as monotherapy | • Gastrointestinal side-effects common |
| • No weight gain | • Very rare risk of lactic acidosis when renal clearance limited (Bodmer et al., 2008) |
| • Low risk of hypoglycaemia | |
| • Non-glycaemic benefits include improvements in atherogenic lipid profiles and reduction in cardiovascular event rates and mortality (UKPDS 34, 1998) |
Sulphonylureas
For people in whom metformin is contraindicated or not tolerated, guidelines generally recommend a sulphonylurea as a suitable first-line alternative if the person is not overweight (NICE, 2009). A sulphonylurea is also generally added as second-line therapy when blood glucose control remains or becomes inadequate with metformin. The sulphonylureas reduce blood glucose levels by increasing insulin secretion from beta cells and therefore they work only in patients who have sufficient remaining beta-cell function.
| Benefits | Disadvantages |
| • Rapid onset of action and almost immediate effects on blood glucose | • Weight gain common |
• HbA1c
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|