Introduction
Osteosarcopenia is an entity relatively unknown to the medical sciences, but an old notion to the body composition analysis studies. In 1989, Zheng and Rosenberg first introduced the term “sarcopenia” in older persons, referring to the loss of skeletal muscle mass with aging based on a set of assessments . In 1996, Heber et al. recognized an entity called “sarcopenic obesity” by employing bio-impedance body composition analysis (BIA), and then concluded that “additional studies are needed to determine the metabolic and clinical significance of sarcopenic obesity.” .
It was not until 2014 that Professor J. Ilich introduced the term “osteosarcopenic obesity,” referring to the loss of bone mass along with the muscular muscle mass in the presence of obesity in older populations . And finally, Professor G. Duque, in 2015, coined the term “osteosarcopenia” in an older population with history of falling where loss of skeletal muscle and bone mass were present, along with frailty . Others have also shown that postmenopausal women with osteopenia and/or osteoporosis evaluated by DEXA had decreased fat, skeletal, and bone mass compared with normal bone density women, suggesting concordance in the change of these three organ masses in postmenopausal women , and in lean polycystic ovary syndrome patients of reproductive age .
From then, till now, many studies have been published about osteosarcopenia, whether accompanied by obesity or not. They all have concluded that osteosarcopenia is an independent risk factor of the human health status , while also demonstrating that osteosarcopenic phenotypes were part of the clinical presentation of many metabolic disorders such as metabolic syndrome (MetS) , polycystic ovary syndrome (PCOS) , osteoporosis , in the form of cachexia in the presence of neoplasias , and as a result of stress system imbalance, and thus, as a result of low-grade, subclinical inflammation .
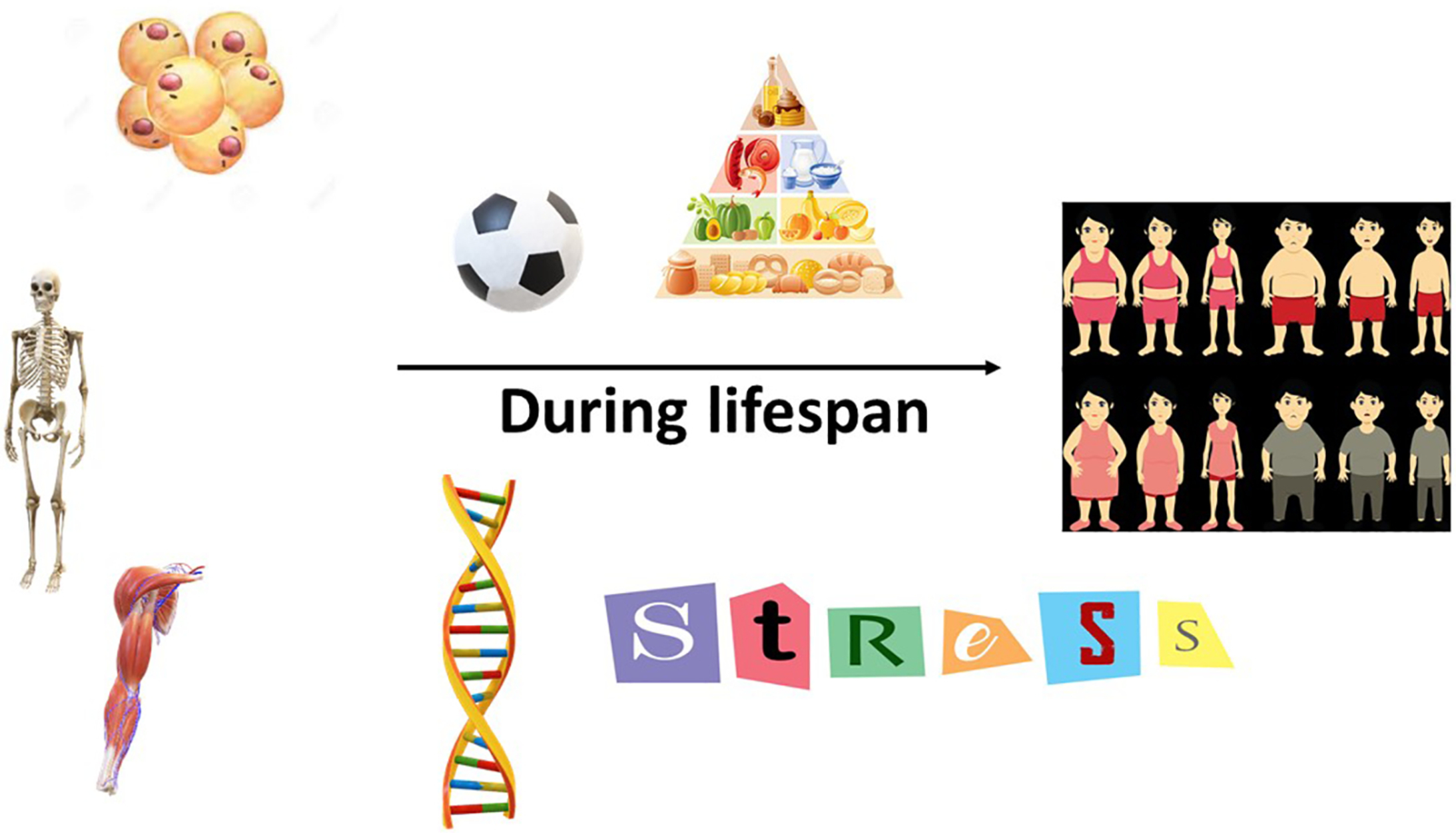
To date, very few studies have addressed the conundrum on the onset of this new condition. This chapter will focus on the osteosarcopenia as an entity during the human lifespan.
Definitions
There is no commonly used definition of the term “osteosarcopenia” just yet. Osteosarcopenia is regarded as a syndrome, characterized by progressive and generalized loss of bone and skeletal muscle mass and strength with a higher risk of adverse outcomes, such as physical disability, poor quality of life and death .
Regarding the definition of sarcopenia, several consensus papers have been published recommending different diagnostic approaches. The most commonly cited are those written under the auspices of the Second European Working Group on Sarcopenia in Older People (EWGSOP2) , the European Society for Clinical Nutrition and Metabolism Special Interest Groups (ESPEN-SIG) , and the International Working Group on Sarcopenia (IWGS) , respectively.
The aforementioned definitions proposed different diagnostic approaches. The presence of low skeletal muscle mass, and either low muscle strength or low muscle performance is diagnostic of sarcopenia, and when all three conditions are present, severe sarcopenia may be diagnosed (EWGSOP) . In contrast, a second definition (ESPEN-SIG) proposed diagnosing sarcopenia only with the presence of low skeletal muscle mass and low muscle strength (which they advised could be assessed by walking speed) . A third definition (IWGS) proposed the presence of low skeletal muscle mass and low muscle function, which they advised could be assessed by walking speed, and “that sarcopenia is associated with muscle mass loss alone, or in conjunction with increased fat mass” . Except for the latter, the first consensus, developed by the EWGSOP separated muscle strength, and muscle performance, and allowed for a slightly broader definition, providing a classification of a severe condition .
Moreover, the diagnosis of sarcopenia can then be carried out by assessing the following parameters:
- 1.
Measure walking speed in older persons (> 65 years): If walking speed is below 0.8 m/s at the 4-m walking test, measure the muscle mass.
- 2.
A low muscle mass, i.e., a percentage of muscle mass divided by height squared is below two standard deviations of the normal young mean (< 7.23 kg/m 2 and in women at < 5.67 kg/m 2 ) as defined using dual energy X-ray absorptiometry. If the walking speed at the 4-m walking test is higher than 0.8 m/s the handgrip strength should be tested; if this value is lower than 20 kg in women and 30 kg in man the muscle mass must be analyzed as described previously. In any of the aforementioned definitions, and when combined with a T-score in the BMD below − 1 SD in the femoral neck, osteosarcopenia could be identified in older persons as a newly described geriatric syndrome that takes its great toll in the health status of these populations . However, the variety of definitions for sarcopenia has limited consensus on how to define osteosarcopenia, a situation that also occurs in osteosarcopenic obesity. Nevertheless, the several features of these syndromes seem to be present in the youth also . Therefore, the burning questions are: Does osteopenia and/or sarcopenia exist in the young populations? Can we define osteosarcopenia in the young populations? and when, or how? Or, is it a strictly geriatric syndrome? .
Pathophysiology
Muscle, fat, and bone cell masses derive from mesenchymal stem cells (MSCs). The differentiation between muscle, fat and bone is influenced by numerous environmental cues, such as hormones . Sarcopenia implicates both loss of muscle mass and subsequent dysfunction, such as impairment of contraction, metabolic, and endocrine abnormalities. It affects metabolism, immune, and inflammatory responses, and includes parameters related to force, functional capacity, and the amount of body fat .
In subjects in development, such as children or adolescents, and in adult humans, appetite regulation and physical activity affect energy balance. More specifically, in children and adolescents, appetite regulation seems to be dysregulated in excess body fat mass, and certain types of exercise favor muscle health, depending on the age. In some individuals, inflammation induces anorexia and fat loss in combination with sarcopenia. However, in others, appetite is maintained, despite activation of systemic, subclinical low-grade inflammation, leading to sarcopenia with seemingly normal or increased fat content .
Sarcopenia is accompanied by infiltration of muscle tissue by lipids, leading to increased adipocyte number and lipid deposition within muscle fibers. Lipid deposition in muscle is called myosteatosis and seems to be the result of the reduced oxidative capacity of muscle fibers with aging. Elevated fat mass in combination with low muscle mass, or increased fat mass together with decreased muscle strength are termed as sarcopenic obesity . Sarcopenia is a diagnosis made by means of dual X-ray absorptiometry (DXA), bioelectric impedance (BIA), or cross-sectional imaging with CT or MRI. However, normative data for skeletal muscle mass are absent, especially in pediatrics. Last, but not least, studies of evaluation of skeletal muscle mass by cross-sectional imaging in children are limited .
Although mechanical forces clearly have a significant role in the pathogenesis of osteosarcopenia, more recent research suggests paracrine, or endocrine cross-talk is implicated. Important hormones mediating this crosstalk include growth hormone/insulin-like growth factor-1 (GH/IGF-1), gonadal sex hormones, and vitamin D, with age-related decreases contributing to the development of osteosarcopenia. Muscle and bone, also, secrete certain factors, known as myokines, and osteokines respectively, which aid the communication between muscle, and bone . An extensively researched myokine is myostatin, a member of the transforming growth factor beta (TGF-β) superfamily, which inhibits skeletal muscle growth, but also has effects on bone and tendon .
Bone-muscle crosstalk is mediated by several important signaling pathways. For example, the canonical Wnt-β-catenin signaling pathway controls osteoblastic activity and is, also, involved in muscle regeneration, the GH/IGF-1 axis is a key regulator of bone and muscle growth, mediating its effects via several signaling pathways. There is hope that exploiting these pathways will facilitate the development of new therapeutic agents in the future .
Genetic polymorphisms of various genes also contribute to the pathogenesis of osteosarcopenia. As reviewed by Kaji et al., these include androgen receptor, estrogen receptor, catechol- O -methyltransferase, IGF-I, vitamin D receptor and low-density-lipoprotein receptor-related protein .
Conclusively, the pathogenesis of osteosarcopenia is multifactorial, with an array of mechanical, biochemical, genetic and lifestyle factors all contributing to involution of the “bone-muscle unit” .
Osteopenia, osteoporosis, and sarcopenia in the young populations
Body composition analysis in the young populations drew interest of many researchers, during the last 10 years. Osteoporosis is defined as a skeletal disorder characterized by compromised bone density and strength, predisposing a person to an increased risk of fracture. Traditionally, osteoporosis is considered as a disease of aged populations. Nevertheless, it occurs in patients of all ages, and is seems to be increasingly identified in the pediatric populations. Patients, of both sexes, including children with chronic diseases, are at risk for bone fragility.
There are several forms of osteoporosis that implicate genetic factors and that should be identified at early stages to ensure adequate treatment. The diagnosis of osteoporosis in the young aged populations is tricky since their bone mineral density (BMD) is affected by growth and pubertal development. In addition to low BMD, an individual in development should present with a significant tendency to fractures before the osteoporosis diagnosis can be made.
Typically, primary osteoporosis is defined as a condition, characterized by global skeletal fragility that develops in association with menopause and advancing age. Secondary osteoporosis may be caused by specific disorders, including endocrinopathies, drugs and genetic diseases that cause low BMD, either by interfering with attainment of peak bone mass or by increasing rates of involutional bone loss . Osteoporosis in children and adolescents may be primary, or secondary ( Table 1 ) .
| Primary osteoporosis |
| Ehlers-Danlos |
| Homocystinuria |
| Marfan’s |
| Osteogenesis imperfecta |
| Idiopathic osteoporosis |
| Genetic osteoporosis |
| Secondary osteoporosis |
| JIA a |
| SLE b |
| IBD c |
| Cerebral palsy |
| Meningomyelocele |
| Myopathies |
| Malabsorption syndromes |
| Shwachman-Diamond |
| Cystic fibrosis |
| Gaucher disease type 1 or 3 |
| Niemann Pick A/B |
| Inborn errors of calcium and phosphorus homeostasis |
| Malnutrition |
| Leukemias |
| Thalassemia |
| Growth hormone deficiency |
| Hypogonadism |
| Turner’s |
| Hyperthyroidism |
| Hyperparathyroidism |
| Cushing’s |
| Vitamin D deficiency |
| Anorexia nervosa |
| Chemotherapy for malignancy |
| Chemotherapy following solid organ transplant |
| Glucocorticoids |
| Anticonvulsants |
| Heparin |
| Calcineurin inhibitors |
| Chronic kidney disease |
| Liver disease |
a Juvenile idiopathic arthritis.
b Systemic lupus erythematosus.
The definition for osteoporosis in children and adolescents includes: (1) A clinically significant fracture history (one or more of the following) (a) Long bone fracture of the lower extremities; (b) Vertebral compression fracture; (c) Two or more long-bone fractures of the upper extremities; (2) Low spinal or total body less head areal bone mineral density or bone mineral content, defined as a Z -score less than or equal to − 2.0 adjusted for age, gender and body size, as appropriate .
Skeletal muscle is a modifiable tissue that presents with plasticity and is capable of altering its structure and its metabolism. Though, the total number of muscle fibers seem to be set during fetal life, between the 6–8th and 8–18th week of pregnancy, as studies have shown . Postpartum, the mass of muscle fibers exhibit more hypertrophy than hyperplasia, meaning that they grow mainly in size and to a lesser degree in number . Thus, defects in muscle development, occurring during fetal development may be maintained postpartum throughout adult life . There are several factors affecting skeletal muscle mass development, such as intrauterine and genetic influences , dietary protein , physical activity , chronic diseases , and obesity , leading to sarcopenia in children and adolescents.
There are many studies that have demonstrated the susceptibility of IUGR, SGA children to reduced myoblast replication and thus, to the development of sarcopenia, later in life . Also, many patients with myopathies, or other neurologic diseases , apart from developing osteopenia and osteoporosis, are prone to sarcopenia, due to the defects in the function of the muscle mass innervation . Growing evidence suggests that osteosarcopenia and osteosarcopenic obesity is on the rise in the pediatric and adolescent populations in the developed countries, probably due to diminished intake of protein, which was below the highest acceptable macronutrient distribution range of 35% for an age/sex group .
Sedentary lifestyle, increased screen time and lack of physical activity and exercise lead to prompt underdevelopment of skeletal muscle mass in children and adolescents . Chronic diseases, such as liver, kidney and intestinal failure cause sarcopenia, due to disruption of ammonia metabolism, subsequent increased muscle mass inflammation, and impaired muscle growth, with grave implications in the prognosis . Obesity in children and adolescents complicate the clinical presentation of sarcopenia. Especially in the case of MetS and prediabetic patients , it seems that they seem to combine early elements of osteopenia/osteoporosis and sarcopenia, exhibiting a mixed phenotype of adult type osteosarcopenic obesity ( Fig. 1 ), as described in the next paragraph.