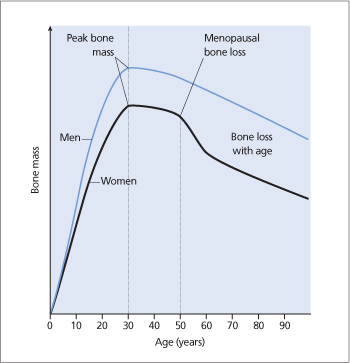
Bone mineral density (BMD) changes with age (Fig. 27.2). The maximum BMD (‘peak bone mass’) is achieved by the age of 30–40 years. Thereafter, bone is lost in both men and women at a rate of about 1% per year. Women experience a phase of accelerated bone loss for 3 years after the menopause. A decrease in spine BMD of 1 standard deviation (or 12%) doubles the risk of fracture. Box 27.1 summarizes the factors that increase the rate of bone loss.
Clinical presentations
Osteoporosis does not cause pain or deformity per se but increases the risk of fractures that can then result in pain, deformity, increased dependence and mortality. Osteoporosis-related fractures associated with minor trauma tend to occur at sites comprising more than 50% trabecular bone (i.e. less than 50% cortical bone). These sites include the:
- vertebral bodies: these fractures result in backache that usually subsides after 3 months. Chronic pain may occur due to secondary osteoarthritis. Vertebral fractures also result in kyphosis, loss of height and abdominal protrusion. Vertebral fractures may appear as wedge deformity (loss of anterior height), end-plate deformity (loss of middle height) or compression deformity (loss of anterior, posterior and middle height)
- proximal femur: mortality is increased by 20% in the first year following a hip fracture
- distal radius (Colles’ fracture).
Figure 27.2 Changes in bone mass with age in men and women.
Investigations
Diagnosis
In patients presenting with osteoporosis-related fractures, BMD is measured using dual-energy X-ray absorptiometry (DEXA). It is worthwhile measuring BMD in patients with low-trauma fractures and those with strong risk factors, for example taking long-term corticosteroids.
Low doses of X-rays of two different energy levels are directed toward areas of interest (lumbar spine, proximal femur, distal radius) and are absorbed to different extents by bone and soft tissue. This principle is used to calculate bone density in g/cm2.
The T-score compares the patient’s BMD with that of a young reference population. The World Health Organization (WHO) has selected a T-score of –2.5 or less to define osteoporosis in healthy postmenopausal women and men aged 50 years and older. The diagnosis of osteoporosis is made by DEXA using the lowest T-score of the lumbar spine (L1–L4), proximal femur or distal radius. A T-score of between –2.5 and –1.0 is referred to as osteopenia.
The Z-score compares the patient’s BMD to that of an age-matched reference population. In premenopausal women and younger men, the relationship between BMD and risk of fracture is not well established. For premenopausal women and men under age 50 years, Z-scores rather than T-scores should be used. In these patients, a clinical diagnosis of osteoporosis may be made in the presence of a fragility fracture, or when there is low BMD and risk factors for fracture, such as longterm steroid therapy or hyperparathyroidism.
Secondary causes
Patients with osteoporosis-related fractures resulting from minor trauma should be investigated to look for secondary causes (Box 27.2).
Other investigations
Markers of bone turnover are not useful in the diagnosis of osteoporosis as there is substantial overlap in normal subjects and patients with osteoporosis. Bone biopsy is rarely used but can be in unusual forms of osteoporosis in young adults. It may provide information about the presence of rare secondary forms of osteoporosis (e.g. systemic mastocytosis).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








