CHAPTER 9
Organization of Diabetes Care
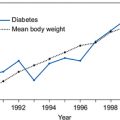
Diabetes is a chronic illness that requires continuing medical care and patient education to prevent acute complications and to reduce the risk of long-term morbidity and mortality. The care is complex and requires that many issues, beyond glycaemic control, are addressed. As a result people with diabetes form a significant part of the workload of healthcare providers and an estimated 10% of the entire National Health Service (NHS) budget (Baxter et al., 2006).
As outlined by the Management Of Diabetes for ExceLlence (MODEL) group, a national model of care is required that can increase the capacity of the healthcare system as a whole to meet the needs of the growing number of people with diabetes, with care provided in the right place at the right time and with the right amount of expertise (Vanterpool, 2008).
There is increasing emphasis for diabetes to be managed in primary care; NHS Diabetes, formerly the National Diabetes Support Team, state that ap-proximately 80% of diabetes care can be delivered in this setting. The level of responsibility for diabetes care expected by government from primary care providers has been formalized through service frameworks, which lay down the minimum standards for the prevention, diagnosis and management of diabetes, and by the Quality and Outcomes Framework targets for diabetes care set out in the General Medical Services contract. However, although a high level of care is delivered by many practices, there remains inequality with much higher rates of diabetes in some deprived areas of the UK compared with the national average. To provide effective diabetes care for all, ways of maximizing capacity at a local level are required.
Managing diabetes in primary care
For many people with diabetes, their GP and practice nurse, who has often completed extra training in diabetes care and does much of the routine checking and health promotion, will provide most of the help and advice they need. They will also have access to an expanded primary care team, which will include a podiatrist, dietician and optometrist. A key member of the multidisciplinary diabetes team is the diabetes specialist nurse whose role has expanded and developed to meet the needs of the ever-growing diabetes pop-ulation and government directives (Box 9.1). The patient with diabetes has many different learning needs relating to diet, monitoring and treatments. Di-abetes specialist nurses provide many of these needs, aiming to help people self-manage their condition. Diabetes specialist nurses generally cover a primary care trust, but work closely with primary care teams. Effective use of specialist nursing provides the patient with a constant point of contact and saves on valuable GP time.
- Education and skill development so individuals with diabetes can manage their condition to the best of their ability.
- Specialist advice and support to individuals with diabetes.
- Education, advice and support to professional and non-professional staff, who care for people with diabetes.
- Group education for people starting on insulin or changing their insulin.
- Crisis management advice and support for people with diabetes or their carers (such as at times of illness and hypoglycaemia).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree