Oral health is intimately associated with general health and well-being.
Poor oral health negatively affects nutrition and systemic health.
Dental caries and periodontal disease are preventable.
Xerostomia can have devastating effects on the health of the hard and soft tissues of the oral cavity.
Root surface dental decay, often a secondary effect of xerostomia, has an increased incidence in older adults.
Medications with xerostomic side effects should be avoided when possible.
Diagnosis of orofacial conditions in elderly persons may be confounded by coincident medical and dental conditions, multiple medications, and vague histories.
The 5-year survival rate of oral cancer has not improved over the past 30 years. Early diagnosis is crucial.
Proper oral hygiene in older adults prevents several life-threatening systemic conditions.
Follow current recommendations regarding antibiotic prophylaxis and anticoagulant therapy as they relate to dental procedures.
teeth, and weakness of the orofacial musculature can all inhibit the intake of nutrients and impact the general health of an individual. Compromised oral health has been linked to cardiovascular and cerebrovascular disease, pneumonia, and diabetes. In addition, feelings of social well-being and self-image, quality of life, life satisfaction, and psychological well-being are directly related to an individual’s oral health.
Lips. Pale pink, homogeneous in color, well-defined border with skin. Bidigital palpation performed to identify uniform submucosal consistency and thickness (see Figs. 35.1 and 35.2).
Common Abnormalities: Ulcerations, irregular surface, white thickenings, recurrent herpetic lesions.
Buccal Mucosae. Uniformly pink/red in color; visualize Stensen duct and check for normal salivary flow. Bidigital palpation to rule out submucosal thickenings or tumors (see Fig. 35.3).
Common Abnormalities: Biteline hyperkeratosis, fibromas, candidiasis.
Buccal Vestibule. Located at the junction of buccal mucosae and alveolar process. Examine for elevations or depressions. Palpate at height/depth of vestibule to identify tenderness or swelling (see Figs. 35.4 and 35.5).
Common Abnormalities: Inflammatory lesions associated with dental abscesses.
Hard Palate. Utilize direct visual inspection. Uniform pink color. Evaluate rugae, palatal raphe, palatine papilla, and maxillary tuberosities (see Fig. 35.6).
Common Abnormalities: Maxillary torus, candidiasis, papillary hyperplasia.
Soft Palate:. Utilize direct vision/mouth mirror; depress tongue if necessary. “Ah” for elevation, which should be
bilaterally uniform. Evaluate uvula for size, color, and texture (see Fig. 35.7).
Common Abnormalities: Candidiasis, swelling, ulcerations, nicotine stomatitis.
Oropharynx. Depress tongue and have patient say “ah.” Evaluate tonsils (usually atrophic in elders) and posterior wall of pharynx (see Fig. 35.8).
Common Abnormalities: Erythema, exudate, asymmetry.
Tongue. Have patient extrude tongue and wrap tip with gauze to properly visualize lateral borders. Assess ventral, lateral, and dorsal surfaces, including papillae, lingual frenum, and vasculature (see Figs. 35.9 and 35.10).
Common Abnormalities: Ulcerations, fibromas, “brown/black hairy tongue” (especially in smokers), geographic tongue. Posterior one third of lateral border is most frequent site of oral cancer.
Floor of Mouth. Visualize as tongue is elevated. Uniform red color. Evaluate Wharton ducts for salivary flow. Bidigital palpation to evaluate submandibular salivary glands, lymph nodes, symmetry (see Fig. 35.11).
Common Abnormalities: Ulcerations, varicosities, mucocele.
Gingivae. Observe color (pink), frenal attachments, and recession.
Common Abnormalities: Inflammation secondary to periodontal disease, recession, hyperplasia, fistulae (see Fig. 35.12).
Teeth. Number present/absent, gross decay, plaque/calculus, mobility, discoloration, and occlusion (Fig. 35.12).
Common Abnormalities: Decay, mobility, gingival abrasion, fractures, lost/fractured restorations, ill-fitting prosthesis.
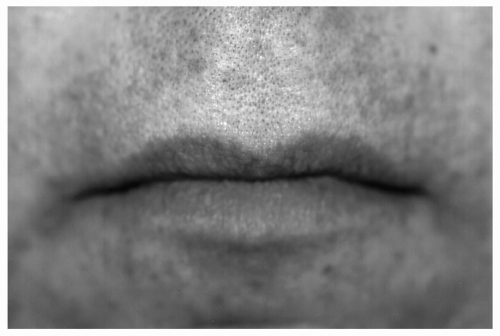 Figure 35.1 Normal appearance of lips. (See color insert.) |
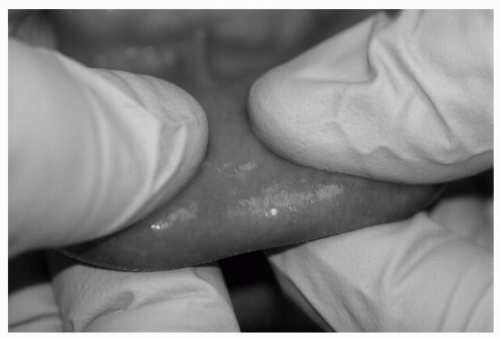 Figure 35.2 Bidigital palpation on lower lip. (See color insert.) |
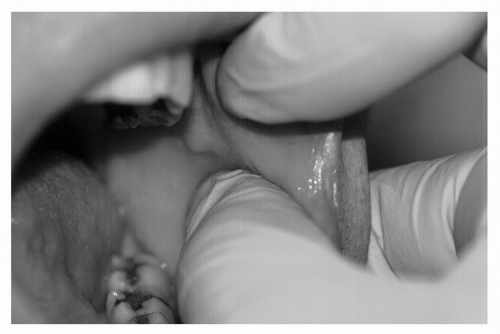 Figure 35.3 Bidigital palpation of buccal mucosa. (See color insert.) |
 Figure 35.4 Visual examination of anterior buccal vestibule, mandibular arch. (See color insert.) |
 Figure 35.5 Visual examination of posterior buccal vestibule, mandibular arch. (See color insert.) |
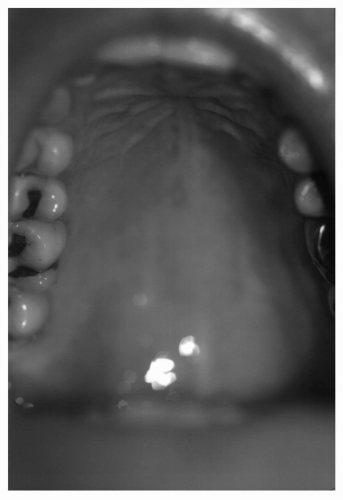 Figure 35.6 Visual examination of hard palate. (See color insert.) |
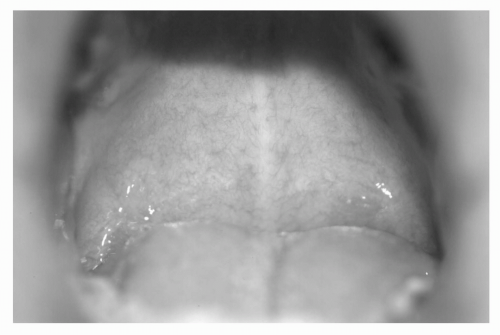 Figure 35.7 Visual examination of soft palate. (See color insert.) |
 Figure 35.8 Visual examination of oropharynx. (See color insert.) |
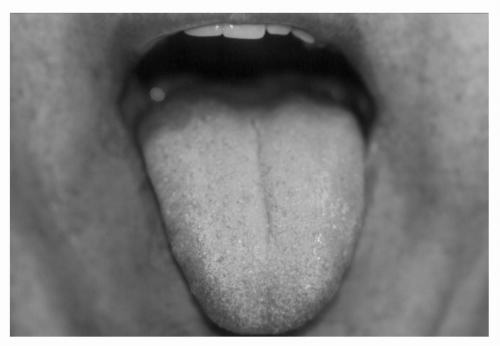 Figure 35.9 Visual examination of dorsal surface of tongue. (See color insert.) |
 Figure 35.10 Visual examination of lateral surface of tongue, including lingual tonsil. (See color insert.) |
patient was placed on daily topical fluoride treatments and instructed to use sugarless lemon drops and frequent sips of water, not sugar-containing beverages, to reduce the feeling of dry mouth. Mr. K. was subsequently placed on a 3-month examination interval. No additional carious lesions have formed and Mr. K. no longer has the feeling of dryness in his oral cavity.
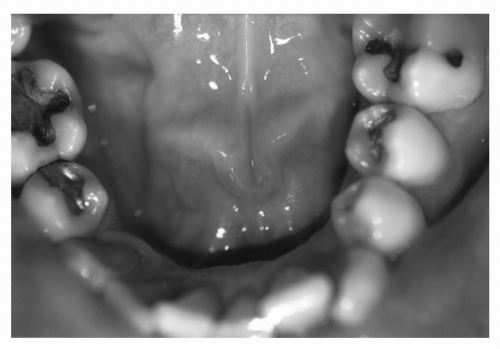 Figure 35.11 Visual examination of floor of the mouth, including Wharton ducts. (See color insert.) |
 Figure 35.12 Visual examination of anterior gingival and teeth. (See color insert.) |
A tooth surface (enamel and/or dentin)
A fermentable substrate (i.e., sugar)
Bacteria that metabolize fermentable substrates into acids.
 Figure 35.13 Root surface caries. (See color insert.) |
The mechanical removal of dental plaque through proper brushing and flossing;
The reinforcement of the composition of enamel through fluoride treatments;
Diet modification;
The use of antimicrobial rinses;
Early attention to salivary dysfunction; and
Professional prophylaxis and intervention at appropriate intervals.
TABLE 35.1 MEDICAL MANAGEMENT OF ORAL CONDITIONS | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




