In 2009, the projected incidence for colon and rectal cancers in the United States was 106,100 and 40,870, respectively, and approximately 75% of these patients were treated with curative intent. Surveillance or follow-up after colon and rectal cancer resection serves multiple purposes; however, the primary argument supporting the validity of surveillance is the detection of metachronous and recurrent cancers amenable to curative treatment. The surveillance may provide some comfort for cancer survivors who can be informed that they have no evidence of disease.
In 2009, the projected incidence for colon and rectal cancers in the United States was 106,100 and 40,870, respectively, and approximately 75% of these patients were treated with curative intent. Despite significant improvements in screening and treatment, the 5-year survival ranges from 64% to 90% primarily because of a 30% to 40% incidence of recurrence. Therefore, the annual additional burden of colorectal cancer survivors available for surveillance for recurrence is approximately 110,000 patients. Despite significant efforts in refining staging modalities with imaging and even proteogenomics, the American Joint Committee on Cancer (AJCC)/tumor-node-metastasis (TNM) staging system remains the gold standard for recurrence risk stratification. This article attempts to review the current status of the evidence related to surveillance strategies after curative colorectal cancer.
Surveillance or follow-up after colon and rectal cancer resection serves multiple purposes; however, the primary argument supporting the validity of surveillance is the detection of metachronous and recurrent cancers amenable to curative treatment. A secondary benefit is that data from the surveillance protocols provide outcomes-based data for the ongoing assessment of prior, current, and experimental treatment modalities. Finally, the surveillance may provide some comfort for the cancer survivors who can be informed that they have no evidence of disease. There is pressure to define which surveillance strategies are cost effective. Most of the available data indicate that early identification of recurrent disease at a curative stage may be illusory.
Current guidelines for postoperative follow-up defined by the stakeholder medical societies vary in intensity of evaluation; however, all guidelines focus on a combination of clinical examination, laboratory testing, imaging, and colonoscopy. Despite evaluation of the same evidence-based data, the expert opinions and recommendations can be inconclusive and disparate. There are currently (at the time of this article’s submission) 8 published randomized trials assessing different regimens for follow-up of patients with colorectal cancer operated for cure. Pietra and colleagues reported an increase in 5-year survival (58.3% vs 73.1%; P <.02) with intense follow-up aimed at discovering local recurrence for colon and rectal cancer. Local recurrences were significantly more frequent in rectal cancer (36.7%) versus colon cancer (15%), and the survival advantage was likely related to an enhanced opportunity for curative management of those recurrences. The only other randomized controlled trial (RCT) that has demonstrated statistical improvement in survival resulting from intense follow-up was by Rodríguez-Moranta and colleagues. This group assessed stage II and stage III colorectal cancers and reported longer survival in patients with stage II tumor (hazard ratio [HR] = 0.34; 95% confidence interval [CI], 0.12–0.098; P = .045) and in those with rectal cancer (HR = 0.09; 95% CI 0.01–0.81; P = .03). The investigators’ strategy compared a simple surveillance strategy of clinical evaluation and serum carcinoembryonic antigen (CEA) monitoring versus intensive strategy in which abdominal computed tomography (CT) or ultrasonography, chest radiograph, and colonoscopy were added. The remaining studies failed to report statistically significant survival advantage based on studies powered to detect a 15% to 20% survival advantage. The follow-up meta-analyses of these studies similarly failed to confirm a reduction in cancer-related mortality with intense follow-up, although there have been benefits in overall survival and earlier detection of recurrence leading to higher incidence of resections of recurrent disease. The recent changes in improved surgical technique and greater use of neoadjuvant and adjuvant chemotherapy and radiation therapy have further confounded the data because of shifts in local and regional failure rates with primary therapy. There are 2 ongoing prospective randomized studies in Europe that may provide clearer information regarding the value of intense surveillance, which are the follow-up after colorectal surgery (FACS) trial and the Gruppo Italiano di Lavoro per la Diagnosi Anticipata (GILDA) trial.
Further complicating the analysis of administrative data sets is not only the diversity of recommendations but also the significant variation in compliance with the recommended surveillance guidelines. A postal survey of active members of the American Society of Colon and Rectal Surgeons (ASCRS) in 2007 demonstrated a wide variation in the frequency of follow-up and the specific diagnostic modalities used. In fact, only 50% of surgeons followed the recommended guidelines as published by the ASCRS. Alternatively, an assessment of follow-up for patients with rectal cancer failed to demonstrate any stage-based differences in patient surveillance strategy. Similarly, a survey conducted from the Netherlands of gastrointestinal departments found that 52% of respondents advised shorter interval assessments than advised by national recommendations. This finding was confirmed in a population-based study by Cooper and Doug Kou, which assessed 9426 patients over 12 months and identified significant variation in compliance between geographic areas and race, with 22.7% of patients receiving more investigations than recommended.
There is clearly a significant gap in the evidence to fully guide an appropriate strategy and a set of investigations capable of defining the frequency and duration of surveillance after curative colon and rectal cancer surgery. In the current era of limited resources, there is an urgent need to define a cost-effective strategy that encompasses effective early identification of recurrence while simultaneously limiting cost and complications from evaluation and treatment. One potential area of improvement is enhanced staging and accurate prediction of the potential for recurrence, thus allowing providers to focus on intense surveillance protocols in the highest-risk patients. These components are discussed later in this article.
Risk assessment
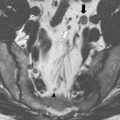
At this point in time, risk assessment for recurrent colorectal cancer is primarily guided by the initial histopathologic stage and the likely sites for metastatic spread (local, liver, lung). Although various putative molecular markers have been proposed, no formal and validated pattern of genetic alterations has been confirmed. The higher risk of local recurrence for rectal cancer compared with colon cancer has led to imaging strategies for the pelvis, whereas colon cancer imaging strategy focuses on the liver and lung. Most treatment failures occur in the first 24 months after surgical treatment for colorectal cancer, which suggests more intensive early surveillance program. The aggressiveness of surveillance must also be tempered by an assessment of the comorbidities limiting tolerance of reoperation or pharmacologic or radiologic treatment of even minimally recurrent disease. Although palliative chemotherapy or radiation therapy may improve the quality of life and possibly the chance of survival, the identification of this population can be based on symptoms rather than surveillance.
Locoregional and distant recurrence
As mentioned previously, the risk of recurrence increases with advanced primary AJCC/TNM staging, with the highest risk for stage IIb to stage III lesions. The proposed combination of biochemical and imaging modalities is designed to identify locoregional and distant recurrence at a curative stage. Because rectal cancer carries a higher rate of local failure than colon cancer, but with a similar rate of distant metastatic disease, the strategies should be modified for imaging. Another confounder is the absence of data on the impact of adjuvant treatment on timing and pattern of recurrent disease, which may affect the benefit of surveillance and intervention for recurrence. Galandiuk and colleagues evaluated 818 patients (Dukes B2 [stage IIb] and Dukes C [stage III]) managed by 3 different adjuvant treatment protocols and found recurrence rates of 40% for colon and 52% for rectal cancer. The median time to recurrence for all patients was 16.7 months (range 0.5–98 months). Histologic grade and aneuploidy predicted a higher risk of recurrence; however, the timing of recurrence was unaffected. Perforation, adhesion, and invasion to adjacent organs led to earlier recurrence in stage III cancers, whereas adjuvant therapy delayed recurrence but did affect the overall rate of recurrence. Similar findings were noted in a single-institution study by Obrand and Gordon of stage I to III colon and rectal cancers with recurrence rate also related to site of lesion, stage, adjacent visceral invasion, and perforation. The median time to recurrence was 17 months, but ranged from 18 months for local disease to 34 months for distant disease. However, 93% of all recurrences occurred within 48 months from index surgery, indicating a time limit for surveillance. A population-based study on management of colon and rectal recurrences over a 28-year time frame found that over time, there was an increase in 5-year survival of patients older than 75 years that correlated with increase in curative-intent surgery for recurrences of locoregional and metastatic disease ( P <.0001). The long time frame was biased by significant changes in patient selection for resection for recurrence; however, the rate of surgery for symptomatic recurrence dropped significantly over time (74.9% to 37.5%; P <.001). Investigators attributed an increase in 5-year survival to a more favorable stage at the diagnosis of recurrences. Kobayashi and colleagues compared recurrence rates for 5230 colon and rectal cancers and confirmed recurrence risk by stage (I, 3.7%; II, 13.3.%; III, 30.8%: P <.0001), and although most recurrences occurred within 3 years (80%) and virtually all recurrences by 5 years (95%), the rate of recurrence was much faster for stage II and III disease, whereas stage I disease was gradual over a 5-year time frame. A German population study raised concerns about the benefit of resection of recurrent disease in a group with a 30.6% rate of recurrence and a 24% rate of R0 resection. Only 2% of patients were alive with no evidence of disease at 2 years after curative re-resection. Harris and colleagues reviewed local recurrences across all stages of colon cancer during a 13-year time frame and reported a 3.1% rate with no primaries at stage I or well differentiated histologically. Once again, tumor fixation, perforation, and fistulization were the primary drivers of local treatment failure in colon cancer, and these features were associated with a short time to recurrence (13 months [range 2–71 months]). Goldberg and colleagues assessed the rate of recurrence for stage II and III recurrences in an adjuvant chemotherapy trial patient population (n = 1247) with 44% of patients recurring; however, 41% of the recurrences had salvage surgery. The patients demonstrated acceptable 5-year, disease-free survival for hepatic, liver, and locoregional recurrences (32%, 27%, and 27%), and postoperative mortality of 2%. Despite an aggressive and expensive intensive follow-up strategy, Goldberg and colleagues reported only a 3.4% absolute increase in cure rate for patients identified during follow-up with either recurrent disease (28 patients) or metachronous lesions (14 patients). Recurrences within the first year from index operation were particularly ominous.
The significant advances in surgical technique and the broader use of neoadjuvant radiation therapy or neoadjuvant chemoradiotherapy have significantly reduced the frequency of local failure in rectal cancer. The Swedish Adjuvant Radiation Trial reported a significant reduction in recurrence with radiotherapy plus surgery versus surgery alone (28% vs 38%; P <.001). The benefit was primarily the result of lower local failure (5% vs 13%) rather than distant recurrences (19% vs 14%). Sauer and colleagues reported similar advantages in association with preoperative chemoradiotherapy, and found this approach to be superior to postoperative chemoradiotherapy in terms of complications and local recurrence. These studies also confirmed that rectal cancer recurrence is uncommon after 5 years with or without neoadjuvant therapy. Guillem and colleagues assessed the natural history of locally advanced rectal cancer (T3–4 or N1) after treatment with neoadjuvant chemoradiation and total mesorectal excision (n = 297), and although 23% developed local or distant recurrence, only 1.3% recurred greater than 5 years after surgery. Local failure and survival were affected by pathologic response greater than 95%, lymphovascular invasion, and/or perineural invasion and positive lymph nodes.
Locoregional and distant recurrence
As mentioned previously, the risk of recurrence increases with advanced primary AJCC/TNM staging, with the highest risk for stage IIb to stage III lesions. The proposed combination of biochemical and imaging modalities is designed to identify locoregional and distant recurrence at a curative stage. Because rectal cancer carries a higher rate of local failure than colon cancer, but with a similar rate of distant metastatic disease, the strategies should be modified for imaging. Another confounder is the absence of data on the impact of adjuvant treatment on timing and pattern of recurrent disease, which may affect the benefit of surveillance and intervention for recurrence. Galandiuk and colleagues evaluated 818 patients (Dukes B2 [stage IIb] and Dukes C [stage III]) managed by 3 different adjuvant treatment protocols and found recurrence rates of 40% for colon and 52% for rectal cancer. The median time to recurrence for all patients was 16.7 months (range 0.5–98 months). Histologic grade and aneuploidy predicted a higher risk of recurrence; however, the timing of recurrence was unaffected. Perforation, adhesion, and invasion to adjacent organs led to earlier recurrence in stage III cancers, whereas adjuvant therapy delayed recurrence but did affect the overall rate of recurrence. Similar findings were noted in a single-institution study by Obrand and Gordon of stage I to III colon and rectal cancers with recurrence rate also related to site of lesion, stage, adjacent visceral invasion, and perforation. The median time to recurrence was 17 months, but ranged from 18 months for local disease to 34 months for distant disease. However, 93% of all recurrences occurred within 48 months from index surgery, indicating a time limit for surveillance. A population-based study on management of colon and rectal recurrences over a 28-year time frame found that over time, there was an increase in 5-year survival of patients older than 75 years that correlated with increase in curative-intent surgery for recurrences of locoregional and metastatic disease ( P <.0001). The long time frame was biased by significant changes in patient selection for resection for recurrence; however, the rate of surgery for symptomatic recurrence dropped significantly over time (74.9% to 37.5%; P <.001). Investigators attributed an increase in 5-year survival to a more favorable stage at the diagnosis of recurrences. Kobayashi and colleagues compared recurrence rates for 5230 colon and rectal cancers and confirmed recurrence risk by stage (I, 3.7%; II, 13.3.%; III, 30.8%: P <.0001), and although most recurrences occurred within 3 years (80%) and virtually all recurrences by 5 years (95%), the rate of recurrence was much faster for stage II and III disease, whereas stage I disease was gradual over a 5-year time frame. A German population study raised concerns about the benefit of resection of recurrent disease in a group with a 30.6% rate of recurrence and a 24% rate of R0 resection. Only 2% of patients were alive with no evidence of disease at 2 years after curative re-resection. Harris and colleagues reviewed local recurrences across all stages of colon cancer during a 13-year time frame and reported a 3.1% rate with no primaries at stage I or well differentiated histologically. Once again, tumor fixation, perforation, and fistulization were the primary drivers of local treatment failure in colon cancer, and these features were associated with a short time to recurrence (13 months [range 2–71 months]). Goldberg and colleagues assessed the rate of recurrence for stage II and III recurrences in an adjuvant chemotherapy trial patient population (n = 1247) with 44% of patients recurring; however, 41% of the recurrences had salvage surgery. The patients demonstrated acceptable 5-year, disease-free survival for hepatic, liver, and locoregional recurrences (32%, 27%, and 27%), and postoperative mortality of 2%. Despite an aggressive and expensive intensive follow-up strategy, Goldberg and colleagues reported only a 3.4% absolute increase in cure rate for patients identified during follow-up with either recurrent disease (28 patients) or metachronous lesions (14 patients). Recurrences within the first year from index operation were particularly ominous.
The significant advances in surgical technique and the broader use of neoadjuvant radiation therapy or neoadjuvant chemoradiotherapy have significantly reduced the frequency of local failure in rectal cancer. The Swedish Adjuvant Radiation Trial reported a significant reduction in recurrence with radiotherapy plus surgery versus surgery alone (28% vs 38%; P <.001). The benefit was primarily the result of lower local failure (5% vs 13%) rather than distant recurrences (19% vs 14%). Sauer and colleagues reported similar advantages in association with preoperative chemoradiotherapy, and found this approach to be superior to postoperative chemoradiotherapy in terms of complications and local recurrence. These studies also confirmed that rectal cancer recurrence is uncommon after 5 years with or without neoadjuvant therapy. Guillem and colleagues assessed the natural history of locally advanced rectal cancer (T3–4 or N1) after treatment with neoadjuvant chemoradiation and total mesorectal excision (n = 297), and although 23% developed local or distant recurrence, only 1.3% recurred greater than 5 years after surgery. Local failure and survival were affected by pathologic response greater than 95%, lymphovascular invasion, and/or perineural invasion and positive lymph nodes.
Metachronous colon and rectal neoplasms
Metachronous neoplasms arise from mucosa at a separate site from the primary cancer or anastomosis in a patient with a personal history of previous colon and rectal cancer. Balleste and colleagues in conjunction with the Gastrointestinal Oncology Group of the Spanish Gastrointestinal Association followed 353 patients with colon and rectal cancer for 24 months to define the factors associated with metachronous lesions. All patients had a colonoscopy between years 1 and 2, and the incidence of metachronous neoplasms correlated with familial, pathologic, and molecular characteristics. The incidence of adenomas was 25%, and the metachronous cancer rate was 1.9. Univariate analysis demonstrated that metachronous neoplasms were associated with personal and previous history of colorectal cancer (odds ratio [OR] 5.58; 95% CI 1.01–31.01) and presence of previous or synchronous adenomas (OR 1.77; 95% CI 1.21–3.17). Two large studies have further evaluated metachronous neoplasm rates. The US Multisociety Task Force on Colorectal Cancer reported a 1.5% rate of metachronous cancers amongst 9029 patients, with about half of the lesions occurring within 2 years from initial resection. A French population-based study, which extended over 27 years, reported that long-term risk for metachronous colorectal cancer was 1.8% at 5 years, 3.4% at 10 years, and 7.2% at 20 years, arguing for the value of long-term colonoscopic follow-up in this at-risk population. The existence of a synchronous colorectal cancer also significantly increases the incidence of early-stage metachronous colorectal cancer, which can be managed curatively. Therefore, a strategy for adoption of a structured colonoscopic screening program that is focused on eradication of adenomatous polyps may prove to be beneficial. The National Polyp Study demonstrated that patients who have undergone a high-quality colonoscopy with adenoma removal have a very low risk of colon cancer diagnosis at 1 year. This strategy should be applicable to patients surgically managed for colon and rectal cancer, whereby performance of a colonoscopy within 1 to 2 years’ postresection should identify any missed synchronous lesions from the index colonoscopy and then allow screening for true metachronous neoplasia. Hyman and colleagues support this contention based on the identification of clinically significant neoplastic lesions found on 1-year follow-up colonoscopy, which occurred primarily in patients who did not have index colonoscopy performed by their operating surgeon. It is unclear whether metachronous cancers actually possess different and more aggressive biologic characteristics as opposed to the possibility of a congenital or acquired increased risk for colonic neoplasia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree