and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Introduction
The conjunctiva, anterior segment, retina, retinal vessels, choroid and optic nerve are all susceptible to damage due to the effects of SCD, with the possible consequences of transient or permanent visual impairment.
Proliferative and Non-proliferative Retinopathy
Definitions
Retinopathy is the most common opthalmological complication seen in SCD. It is classified into two subtypes.
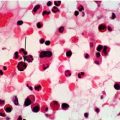
Non-proliferative retinopathy (NPR) is common, but does not lead to visual loss and does not need intervention. Features on retinoscopy include salmon patches (intra-retinal hemorrhage) schisis cavities (retinal deficits left after resolution of intraretinal hemorrhage), iridescent spots, black sunbursts (choroidoretinal scars from pigmentation around vessels), angioid streaks (breaks in Bruch’s membrane) or macular remodelling.
Proliferative Retinopathy (PR) The progressive clinical features are described in the Goldberg staging scheme (Table 10.1).
Table 10.1
Goldberg staging scheme for proliferative retinopathy
Stage
Clinical Findings
Stage I: Peripheral arteriolar occlusions
Early stages of vaso-occlusion. Vessels are initially dark red but later become ‘silver wires’
Stage II: Vascular remodelling, formation of arteriovenous anastomoses
Blood diverted from occluded to adjacent vessels
Stage III: Peripheral retinal neovascularization
‘Sea fan’ formation- neovascular tufts. These can grow and gain fibrous envelopes (elevated ridges)
Stage IV: Vitreous hemorrhage
Stage V: Retinal detachment
The fibrous sea fans and residual organised blood clot from vitreous haemorrhage pull on the retina leading to detachment.
Pathophysiology
Retinopathy is due to vaso-occlusion of the retinal vessels. The arteriolar occlusion and subsequent loss of capillary perfusion leads to ischemia, and release of growth factors which stimulate new vessel formation (neovascularization). These fragile new vessels grow out from the surface of the retina and have a tendency to bleed (vitreous hemorrhage). Intra-ocular blood is degraded, but repeated hemorrhage leads to fibrous tissue accumulation which contracts and pulls on the underlying retina resulting in retinal holes and detachment. There is a balance between pigment epithelium-derived factor (PEDF) which is anti-angiogenic, and vascular endothelial growth factor (VEGF). An increase of VEGF relative to PEDF is associated with neovascularization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree