Fig. 17.1
(a) Hemorrhagic orbital cellulitis in a patient with neutropenic fever, thrombocytopenia with proptosis, ophthalmoplegia. and optic nerve dysfunction. (b) Computed tomography scan showing ethmoid sinusitis with strands in the soft tissue in the orbit and an obvious proptosis
Cancer patients with orbital cellulitis, especially those with sinusitis, are admitted for broad-spectrum antimicrobial coverage with close monitoring of the infection. If surgery is deemed necessary for sinusitis owing to its extent or impact on the ocular structures, urgent surgical debridement is performed, after which intravenous antimicrobial treatment may be used depending on culture findings and sensitivity resulting from the debridement. Commonly involved organisms are those typically found in the nasal passages: Staphylococcus and Streptococcus species followed by Haemophilus influenzae, Klebsiella pneumoniae, and fungi (Schell et al. 2008; Chaudhry et al. 2008; Epstein and Kern 2008; Durand 2008). The infectious disease service should be involved in guiding the treatment regimen, particularly for patients who are severely immunocompromised during chemotherapy or immunosuppressed after allogeneic transplantation.
If the sinusitis is not controlled and leads to worsening ocular symptoms, repeated debridement may be necessary. Frequent ophthalmologic evaluations are important in monitoring optic nerve function (vision check, visual field, pupillary response, and color tests), eye motility, and proptosis level. Once the condition appears to stabilize, follow-up may be decreased until the patient can be discharged. The optimal approach to management of orbital cellulitis, especially in patients with acute or chronic sinusitis, is for the primary team to work in a multidisciplinary fashion with the ophthalmology (oculoplastics in particular), infectious disease, and head and neck surgery services (Schell et al. 2008; Durand 2008).
Corneal Ulceration and Perforation
Corneal ulcers in patients with infections or nonhealing corneal wounds can lead to corneal thinning and perforation, which is an ocular emergency. The cornea is composed of highly innervated avascular tissue that is approximately 0.5 mm thick with unique, complex wound-healing properties. When the corneal epithelium does not heal, the corneal stroma can continue to thin, leading to perforation. Chemotherapy, allogeneic transplantation, irradiation of the ocular region, and surgery that distorts the eyelid and/or orbit position can have many side effects on the ocular surface and/or cornea, such as chronic dryness, inflammation, corneal thinning, exposure keratopathy (the eyelids do not close completely), and neurotrophic keratopathy (corneal sensation is diminished, predisposing the cornea to decreased wound-healing capacity and infections). These conditions can predispose the cornea to microabrasions or large epithelial defects where infection ulcers can occur; given the immune status of cancer patients, such infections are often severe. Irradiated eyes are particularly susceptible to ocular surface diseases and infections (Chaques et al. 2000; Yoshida et al. 2006). Often, these patients also have globe and eylid position malformation, particularly patients with head and neck cancer requiring surgery followed by chemoradiation, which increases the patient’s risk of ocular infections (Fig. 17.2).


Fig. 17.2
Status of a patient with hypoglobus, enophthalmos, and exposure and neurotrophic keratopathy with a corneal ulceration after maxillectomy and radiotherapy
Patients with corneal ulceration may experience redness, discharge, blurred vision, and the appearance of opacity on the cornea, often without pain in a neurotrophic cornea (Fig. 17.3). Patients using contact lenses harbor worse microbial flora and experience worse corneal infections than do patients who do not wear them. This is an important consideration for cancer patients, who should avoid wearing contact lenses during their treatment, as the lenses can serve as sources of severe corneal ulceration. Workup for a moderately sized corneal ulcer includes gently scraping the cornea for Gram staining and culture. A wide spectrum of microbes (bacterial, fungal, and, less likely, viral) can infect the cornea, but the typical infecting organism is either Gram-positive or -negative (Durand 2008). Treatment with fortified topical broad-spectrum antibiotic drops is performed around the clock along with frequent lubrication. Topical antifungal treatment is usually started only when the index of suspicion for infection is high (according to the pattern of infection on the cornea, a Gram-positive stain, or a positive fungal culture after cornea scraping, which can take up to several weeks) (Schell et al. 2008). Typically, patients receive therapy in an outpatient setting and are observed daily until their condition improves. For a nonhealing corneal ulcer with persistent epithelial defects, especially in a patient with a neurotrophic cornea, surgical intervention, such as temporary tarsorrhaphy and an amniotic membrane patch graft, may be required to promote epithelial healing. If the cornea continues to thin despite these measures, corneal perforation may occur (Fig. 17.4).
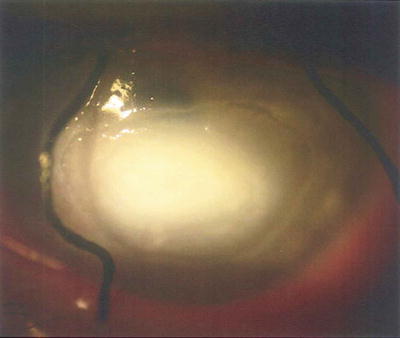

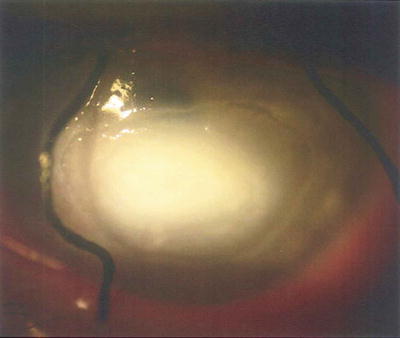
Fig. 17.3
A corneal ulcer with dense white infiltration and corneal thinning. Sutures on the lids are for opened temporary tarsorrhaphy performed to protect and promote a neurotrophic cornea

Fig. 17.4
Eye of a patient with abnormal eyelid closure and a neurotrophic cornea after maxillectomy. Of note is the central hole in the cornea (corneal perforation) with corneal scarring inferiorly from the area of chronic exposure keratopathy
Perforation of the cornea is a serious ocular emergency, as it is an opened globe, requiring immediate closure. Patients with corneal perforation are admitted to the hospital for intravenous administration of antibiotics to prevent endophthalmitis (an infection inside the eye) and should undergo surgery as soon as possible. The primary goal of treatment is to re-establish the integrity of the eye by closing the open wound via any measure necessary, with visual rehabilitation being the secondary goal. The surgical approach depends on the location and degree of the perforation. Unlike the conjunctiva, the cornea cannot be closed with sutures alone when tissue loss such as ulceration or corneal melt occurs. Microperforations can be managed urgently in the clinic with cyanoacrylate glue and a bandage contact lens (Fig. 17.5) in preparation for surgical repair, which may include a multilayer amniotic membrane with a patch graft if the perforation is small. For larger corneal perforations, urgent penetrating corneal transplantation may be needed (Schell et al. 2008; Durand 2008; Azuara-Blanco et al. 1999).
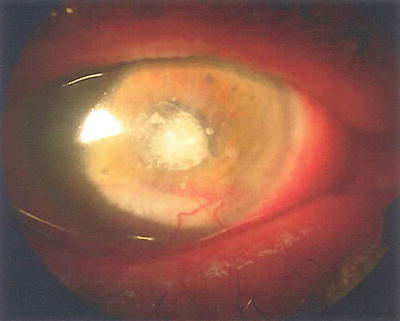
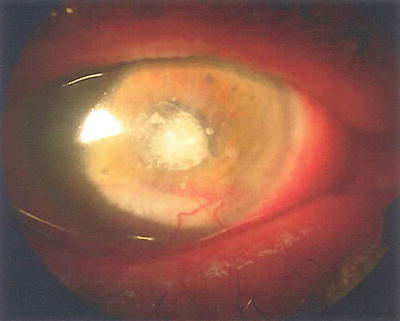
Fig. 17.5
Use of cyanoacrylate glue for closure of a corneal perforation covered with a bandage contact lens
Acute Graft-Versus-Host Disease (Stage IV)
Graft-versus-host disease (GVHD) can occur in a patient who undergoes allogeneic stem cell transplantation (SCT) when the graft, in this case, the donor cells (peripheral blood stem cells or bone marrow cells obtained from either a related or unrelated matched donor or stem cells obtained from cord blood), react to the patient (the host). GVDH is one of the greatest impediments to successful SCT (Wolf et al. 2012). Acute GVHD typically occurs early after SCT (no more than 100 days) and can affect the skin, liver, gastrointestinal tract (including the mouth), lungs, and eyes. Grade IV GVHD is a severe form of acute systemic GVHD involving multiple organs in which the patient may experience significant bullar formation, skin desquamation, liver abnormalities, and gastrointestinal dysfunction. Patients with acute GVHD are admitted as inpatients and given multiple modalities of immunosuppressive therapy. Acute stage IV ocular GVDH can occur as an ophthalmologic emergency in this setting (Kim et al. 2008).
Stage IV ocular GVHD is a rare form of GVHD in which the bilateral corneal epithelium can slough completely off in a patient with intense conjunctival inflammation having pseudomembranous and membranous keratoconjunctivitis, lacrimal gland dysfunction, and ulcerations (Fig. 17.6). The sloughing of corneal epithelium requires evaluation and treatment, as an exposed cornea with a large epithelial defect can result in corneal thinning, infection, ulceration, and perforation (Jabs et al. 1989). Patients with stage IV ocular GVHD experience intense eye pain, as the cornea is the most sensitive part of the body with the highest density of sensory nerve fibers, as well as discharge, debilitating photophobia, and blurred vision. In addition, patients typically are unable to fully open their eyes owing to their discomfort. Often, patients with stage IV ocular GVHD must be examined at the bedside because their condition does not allow for transfer from a hospital room to the clinic for evaluation. Stage III ocular GVHD (pseudomembranous/membranous conjunctivitis without corneal epithelial sloughing) also requires aggressive treatment to prevent both progression to stage IV disease and scarring of the palpebral conjunctiva. Stage III ocular GVHD is not as severe as stage IV disease because the corneal epithelium remains intact.
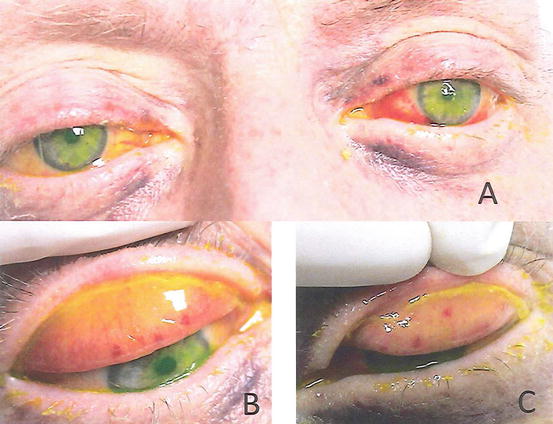
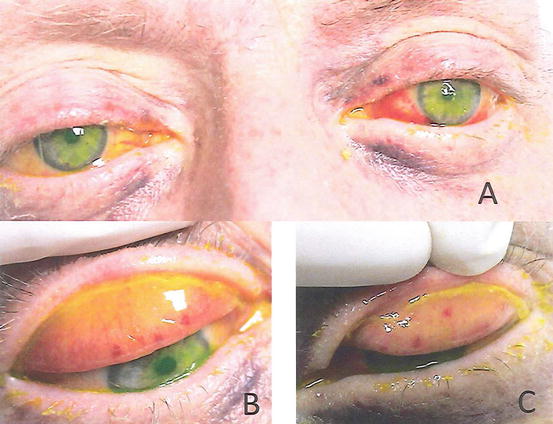
Fig. 17.6
(a) Stage IV ocular GVHD in a patient with stage IV systemic GVHD after SCT. (b and c) Everted upper eyelids exhibiting pseudomembranous/membranous keratoconjunctivitis requiring debridement. The yellow coloration is the fluorescein uptake of denuded corneal epithelium
Examination of acute ocular GVHD is typically difficult owing to its severity, and topical anesthetic drops are used to aid in the evaluation. Workup should include a viral swab and/or culture to rule out a concomitant viral infection, which can have a presentation similar to that of GVHD. Optimal treatment of systemic GVHD is required. However, once it becomes steroid-refractory, acute GVHD is challenging to manage, requiring the use of a variety of immunomodulating agents and photopheresis. Furthermore, management of ocular GVHD is equally challenging for both the patient, who is very ill, and the physician, who may have to perform ocular procedures at the bedside (Kim et al. 2008).
At MD Anderson, stage IV ocular GVHD is treated with debridement of the necrotic ocular tissue (pseudomembranes/membranes on the palpebral conjunctiva) (Fig. 17.7) with or without amniotic membranes (which can be achieved via insertion of a commercially available amniotic membrane ring device). Hourly application of a topical steroid is often needed in addition to that of topical prophylactic antibiotics and copious lubrication. Punctal occlusion with silicone plugs is important in not only addressing a lack of tearing but also increasing the topical medication on the ocular surface by prohibiting its drainage into the nasolacrimal duct. Patients must be monitored closely for recurrence of pseudomembrane and/or membrane formation, which can often necessitate repeated debridement, and for re-epithelization of the cornea. The prognosis for stage IV ocular GVHD can be surprisingly encouraging if treated expeditiously, although the visual outcome depends on the rate at which the cornea heals. The danger of a persistent corneal epithelial defect is its accompanying risk of perforation, which may lead to endophthalmitis, loss of vision, or loss of the eye, all of which underscores the importance of close follow-up for patients with stage IV ocular GVHD. The prognosis for stage IV systemic GVHD is related to whether it responds to the use of systemic steroids, and it can be guarded for patients whose disease is refractory to steroids (Kim et al. 2008).
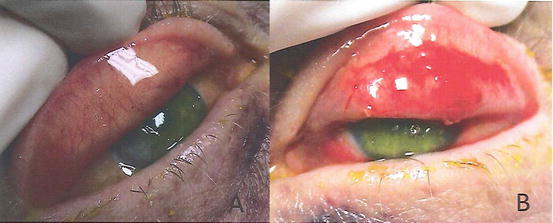
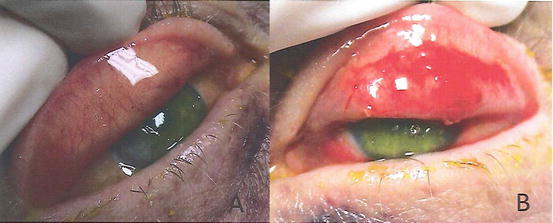
Fig. 17.7
Postsurgical debridement of the (a) right upper eyelid and (b) left upper eyelid for treatment of stage IV ocular GVHD
Herpetic Disease
Herpes reactivation is common in cancer patients. Patients often undergo prophylaxis with antiviral medications (either acyclovir or valacyclovir) during their cancer treatment. Herpes zoster infection can involve the eye with V1 distribution of the trigeminal branch (herpes zoster ophthalmicus) (Fig. 17.8), whereas herpes simplex virus infection can present as patient-described conjunctivitis. An ophthalmologic consultation is performed when a patient presents with herpes zoster ophthalmicus, has vesicles characteristic of herpes simplex virus infection around the eye and/or eyelids, or has disseminated herpes (Johnson 2008).
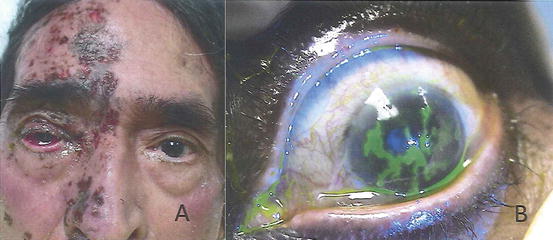
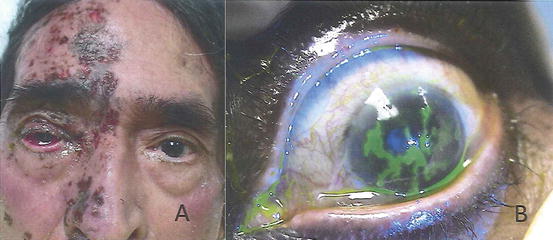
Fig. 17.8
(a) V1 distribution of herpes zoster virus infection (herpes zoster ophthalmicus ). (b) Classic corneal dendritic keratitis caused by herpes simplex virus
Symptoms of herpetic disease range from ocular irritation and epiphora to severe pain, photophobia, discharge, redness, and blurred vision. Both herpes simplex virus and herpes zoster infection can cause classic dendritic keratitis, which affects the corneal epithelium (Fig. 17.8). They may also cause conjunctival inflammation, significant scarring and cicatricial conjunctivitis, corneal stromal keratitis, iritis, uveitis, and trabeculitis (inflammatory glaucoma) (Johnson 2008; Kaufman 2008; Knickelbein et al. 2009). Development of a herpetic infection involving the retina is an ophthalmologic emergency. Although rare, herpetic retinitis can lead to irreversible vision loss and other intraocular complications in cancer patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree