Fig. 5.1
View onto the medial aspect of a pancreatoduodenectomy specimen. Note the ovoid-shaped pancreatic transection margin with a dilated main pancreatic duct (MPD). The groove of the superior mesenteric vein (black arrows) is slightly curved and has a shiny surface. In contrast, the surface facing the superior mesenteric artery (Sma) is rough and fibrous
5.2.1.2 External Examination
In many instances, the presence of a pancreatic cancer may not be visible on external inspection of a pancreatoduodenectomy specimen. Occasionally, however, the tumour may cause bulging of a surface or irregularity of the duodenal mucosa or papilla of Vater. In particular, narrowing of the SMV groove or irregularity of its surface may indicate the presence of a tumour. In a similar way, the presence of an adherent segment or sleeve resection of a vein (SMV or portal vein) or artery (e.g. the hepatic artery) indicates tumour infiltration. Palpation will usually confirm the presence of an indurated tumour mass.
External examination can also reveal a variety of other pathological conditions, such as a tumour of the papilla or ampulla of Vater, dilatation of the papilla with oozing of mucus in case of intraductal papillary mucinous neoplasia or a rare annular pancreas that surrounds the entire duodenal circumference.
5.2.2 Distal Pancreatectomy Specimens
Orientation of distal pancreatectomy specimens is straightforward, especially as cancer specimens always include the spleen. Further helpful with specimen orientation is the presence of the splenic vessels, which run along the superior border of the pancreatic body and tail (Fig. 5.2).
Fig. 5.2
View onto the posterior aspect of a distal pancreatectomy specimen following laparoscopic procedure. Note the staple lines on the pancreatic transection margin (Panc TM) and the transection margins of the splenic artery (Spl a TM) and vein (Spl v TM)
5.3 Specimen Fixation
5.3.1 Specimen Handling Prior to Fixation
To allow biobanking of fresh tissue samples, pancreatic resection specimens must be received unfixed, on ice, transported directly from surgical theatres (see also Sect. 5.10). The distal stomach and/or duodenum are opened longitudinally with scissors and rinsed. To avoid transection of a periampullary tumour, the duodenum should be opened along its antimesenteric aspect after careful probing with a finger. The gallbladder is opened longitudinally and rinsed. The specimen should not be pinned on a cork plate, as this is unnecessary and delays fixation.
5.3.2 Specimen Fixation
Fixation in buffered formalin should be approximately 48 h. The centre of the pancreatic head may not be fully fixed after 48 h; however, longer fixation of the specimen risks extensive autolytic change. Therefore, it is better to dissect the specimen after 48 h and leave the cassetted tissue samples in formalin for a few hours, which will complete the fixation process swiftly. Focal opening of a large cystic lesion, allowing the cyst content to drain and formalin to enter the cavity, will expedite fixation and ensure better preservation of the cavity-lining tissue.
5.4 Inking of the Specimen Surface
Inking of the specimen surfaces serves a dual purpose. It helps with orientation during macroscopic and microscopic examination, and it allows unequivocal microscopic identification of the true specimen surface, which is important for accurate margin assessment.
Inking is easiest done after specimen fixation, because inks stick better to fixed than fresh tissue surfaces. So-called bleeding of colours can be reduced by spraying 10% acetic acid onto the freshly applied ink. Should inking of a fresh specimen be required, the use of ground dry pigment dissolved in acetone may be considered. The use of acetone as a dissolvent ensures rapid drying of the dye, which reduces bleeding of colours.
The various specimen surfaces should be inked in different colours according to a locally agreed colour code. In pancreatoduodenectomy specimens, five different surfaces are discerned, whose identification and examination is part of the margin status assessment (Fig. 5.3) [9–11]. The surfaces of the pancreatic head are – as outlined in Sect. 5.2.1.1 – the anterior and posterior surface, the SMV groove and the SMA surface. Although the anterior surface is not a true resection margin but an anatomical surface that faces the lesser sac, inclusion of this surface in the assessment is important, as involvement of this surface increases the risk of cancer recurrence [12]. A further margin consists of the circumferential surface of the extrapancreatic common bile duct. Examination of the various specimen surfaces and resection margins is discussed in detail in Sect. 5.9.
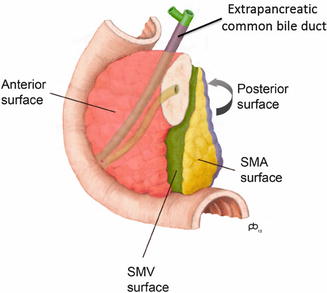
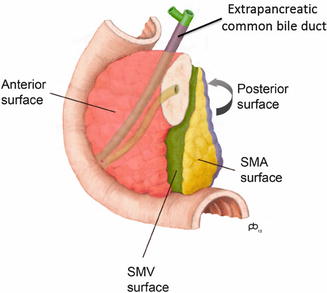
Fig. 5.3
Circumferential resection margins of pancreatoduodenectomy specimens are inked in different colours: red, anterior; green, facing the superior mesenteric vein (SMV); yellow, facing the superior mesenteric artery (SMA); blue, posterior; purple, around the extrapancreatic common bile duct (With permission of Springer, Pathology of the pancreas – a practical approach, [10], Fig. 3. 4, p. 31)
In distal pancreatectomy specimens, two surfaces are discerned and inked: the anterior and posterior surface [10, 11]. If the transection margin of the splenic vessels is of particular concern (Fig. 5.2), this small area may also be inked in a separate colour, such that it can be easily identified during specimen dissection, tissue sampling and microscopic examination.
Pancreatic specimens resulting from an extended resection include one or more additional structures or organs, e.g. a part of the SMV, (meso-)colon or small bowel in extended pancreatoduodenectomy specimens, and the left adrenal gland, part of the stomach or left colon in extended distal pancreatectomy specimens. In such instances, additional surfaces or resection margins must be inked, depending on the individual case.
For practical purposes, it is best to carefully remove without tissue disruption any surgical sutures, clips or staples prior to inking, as the presence of these may render specimen dissection difficult.
5.5 Specimen Dissection
Specimen dissection takes a central place in the macroscopic examination process. Its purpose is to reveal lesions and display them in a way that is conducive to accurate description and assessment as well as optimal tissue sampling. Currently, three dissection techniques are being used worldwide: the bi- or multivalving technique, the bread loaf slicing approach and the axial slicing technique [9, 10]. The principal difference between these three dissection techniques is the plane of sectioning. In the bi- or multivalving technique, the specimen is sliced along the plane that is defined by probes inserted in the main pancreatic duct and common bile duct (Fig. 5.4). According to the bread loaf slicing technique, the specimen is sliced along a plane that is parallel to the transection margin of the pancreatic neck (Fig. 5.5). With the axial slicing technique, pancreatoduodenectomy specimens are serially sliced in the axial plane, i.e. along the plane that is perpendicular to the longitudinal axis of the descending part of the duodenum (Fig. 5.6). It is the same plane as the one that is used for computerized tomography (CT) imaging of the pancreas. The following sections will provide a detailed description of the axial slicing technique for pancreatoduodenectomy specimens and discuss the advantages of this technique compared to other approaches. Dissection of distal, total and extended pancreatectomy specimens will be discussed separately.
Fig. 5.4
Bi- or multivalving of pancreatoduodenectomy specimens. The specimen is sliced along the plane defined by the pancreatic and common bile duct. The resulting specimen slices are large and usually require further dissection, e.g. in a plane parallel to the pancreatic transection margin (With permission of Elsevier, from: Verbeke [9], Fig. 2)
Fig. 5.5
Bread loaf slicing technique of pancreatoduodenectomy specimens. The specimen is serially sliced along the plane that is parallel to the transection margin of the pancreatic neck (With permission of Elsevier, from: Verbeke [9], Fig. 3)
Fig. 5.6
Axial specimen dissection of pancreatoduodenectomy specimens. The specimen is serially sliced in a plane perpendicular to the longitudinal axis of the descending duodenum. The resulting specimen slices at various levels have a characteristic configuration (With permission of Elsevier, from: Verbeke [9], Fig. 4)
5.5.1 Axial Slicing of Pancreatoduodenectomy Specimens
Dissection according to this technique does not require any further specimen preparation, and, in particular, the main pancreatic duct or distal common bile duct should not be probed or opened. If a metal stent is present in the common bile duct and it cannot be removed by gentle pulling, the metal mesh should be opened by cutting several wires, following which wires can be extracted individually using small pliers. Plastic stents can remain in situ as they do not hinder specimen dissection. Slicing of a fixed specimen in the axial plane is technically easy; hence, specimen slices can be thin (3 mm), and a pancreatoduodenectomy specimen will result in at least 10, often 12–14 or more slices. Using a long dissection knife and pulling it steadily across the specimen with long violin bow strokes ensure that the cut surface of the specimen will be smooth and even. Specimen slices are laid out in sequential order, the inferior side facing upward (as on CT imaging), as illustrated in Fig. 5.7.
Fig. 5.7
Axial specimen slices of a pancreatoduodenectomy specimen are laid out in sequential order, from cranial (top left) to caudal (bottom right). Fourteen thin specimen slices provide detailed views on the local anatomy. Abbreviations: AMP ampulla, ANT anterior surface, CBD common bile duct, DUO duodenum, MPD main pancreatic duct, NECR necrosis, POST posterior surface, SMA superior mesenteric artery, SMV superior mesenteric vein, TU tumour (With permission of Springer, Pathology of the pancreas – a practical approach, [10], Fig. 3.10, p. 33)
5.5.2 Advantages of the Axial Slicing Technique
Compared to the bi- or multivalving and bread loaf slicing techniques, axial specimen slicing has the following advantages:
Technical ease: slicing in the axial plane is easy to perform, especially because the duodenum is transected cross-sectionally (in contrast to the bread loaf slicing technique, according to which the duodenum is sliced longitudinally).
Universal applicability: all pancreatoduodenectomy specimens can be dissected by axial slicing, irrespective of the pathology – neoplastic or nonneoplastic – they contain. This is important, as the correct diagnosis is often unknown preoperatively.
Standardized display: as the plane of dissection (axial) is fixed, the local anatomy of the pancreas and adjacent structures is always displayed in the same fashion. This allows straightforward identification of pathological changes and recognition of anatomical variation, which is not uncommon in this area. In contrast, because the plane of sectioning of the bi- or multivalving technique is defined by probes in the common bile duct and pancreatic duct, and the position of these varies between individual patients, dissection varies between specimens. As a consequence, it is more difficult to compare findings between various cases. By using a single fixed plane – the axial plane – macroscopic findings in axial specimen slices are as easily and universally “readable” by pathologists from different centres as findings on CT imaging can be interpreted by radiologists worldwide.
Thin specimen sections: as axial slicing is easy to perform, numerous thin specimen slices can be cut, which allow detailed views on local anatomy and pathological changes throughout the pancreatic head and adjacent structures.
Detailed display of the periampullary region: thin axial specimen slices allow detailed examination of the minute structures of the major ampulla and papilla, the junction with the main pancreatic duct and common bile duct and the adjacent duodenum (see Sect. 5.6.1). Unlike the bi- or multivalving technique, which requires “releasing cuts” through the periampullary area [13], there is no need for additional dissection when using the axial slicing approach.
Comprehensive and accurate margin assessment: in each axial specimen slice, all circumferential margins of the pancreatic head can be inspected. As such, the relationship of the tumour to the margins can be evaluated at multiple levels along the entire craniocaudal length of the pancreatic head. Multiple studies and a recent meta-analysis have shown that the detection of margin involvement is more accurate when using the axial slicing technique than any other dissection method [4, 14–16].
Easy tissue sampling: because axial specimen slices are thin, tissue samples can be excised from the slices and directly transferred to the tissue cassettes without the need for further dissection.
Communication with clinical colleagues: because the axial specimen slices display the local anatomy and pathological changes in the same way as they appear on CT imaging, findings are readily understandable by surgeons, oncologists and radiologists (Fig. 5.8).
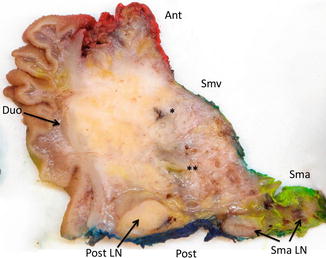
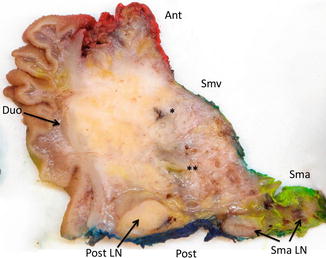
Fig. 5.8
Axial specimen slices of pancreatoduodenectomy specimens provide a view on the local anatomy that is similar to that seen on CT images. Note the main pancreatic duct (*) and distal common bile duct (**), which are partially involved by tumour. Abbreviations: Ant anterior surface, Duo duodenum, Post posterior surface, Post LN posterior pancreatoduodenal lymph node, Sma surface facing the superior mesenteric artery, Sma LN lymph nodes in the adipose tissue facing the superior mesenteric artery, Smv surface facing the superior mesenteric vein
5.5.3 Dissection of Distal and Total Pancreatectomy Specimens
Distal pancreatectomy specimens are dissected by serial slicing in the sagittal plane [5, 6, 8, 10, 11, 17]. Longitudinal opening of the main pancreatic duct is not recommended, because it may be technically difficult, it disrupts the specimen surface (and thus interferes with margin assessment) and does not result in a better display of lesions than by sagittal slicing. Total pancreatectomy specimens are best dissected by a combined axial and sagittal slicing technique. The point of change from axial to sagittal slicing may be moved towards the pancreatic body, depending on the site of a centrally located tumour and the involvement of resected segments of artery or vein.
5.5.4 Dissection of Extended Pancreatectomy Specimens
Dissection of these specimens may require deviation from the standard protocol, although in almost all instances, the pancreatic part of the extended resection specimen will be dissected as described in Sects. 5.5.1 and 5.5.3 (Fig. 5.9).
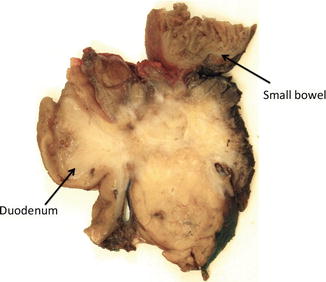
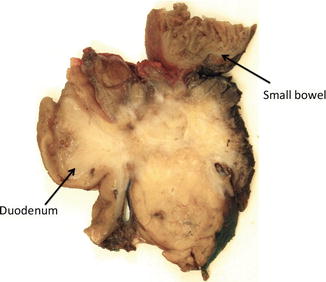
Fig. 5.9
Specimen resulting from an extended pancreatoduodenectomy with resection of a loop of small bowel that is adherent to the anterior surface of the pancreatic head. Note that the bowel wall proper is clear of tumour
5.6 Macroscopic Examination
The aim of the macroscopic examination of dissected specimens is to obtain an accurate record of the tumour: the appearance of the tumour, its size and extent, and its exact location and relationship to anatomical structures, specimen surfaces and margins. Furthermore, assessment of the relationship of the tumour to anatomical structures other than those of relevance for T-staging of pancreatic cancer [18, 19] is of particular interest to surgical and radiology colleagues regarding the preoperative assessment of resectability and patient selection. Equally important, the exact location of the tumour with respect to the bile duct, ampulla and duodenum is crucial for the identification of the cancer origin. Indeed, the distinction of pancreatic ductal adenocarcinoma from cancer of the common bile duct, ampulla or duodenum is primarily determined by the localization of the centre of the tumour mass, a finding that is appreciated macroscopically and confirmed microscopically [3]. The following sections provide guidance for the identification of such anatomical structures.
5.6.1 Identification of Anatomical Structures in Pancreatoduodenectomy Specimens
The intrapancreatic common bile duct runs obliquely through the posterior aspect of the pancreatic head. It can be distinguished from the main pancreatic duct by its thicker wall (1–2 mm), the possible presence of green-stained bile and/or a stent in the lumen, the absence of communicating branch ducts and its more posterior position within the pancreatic head (Fig. 5.10).
The main pancreatic duct lies medial to the common bile duct and has a thin, membranous, cream-coloured wall. Occasionally, communication with branch ducts may be visible macroscopically, if the latter are dilated (Fig. 5.10).
The ampulla of Vater is an olive-shaped firm nodular structure that straddles the duodenal wall. The slightly elevated duodenal mucosa surrounding the draining ampullary channel is the papilla of Vater. The junction of the ampulla with the main pancreatic duct lies a few millimetres caudal to the junction with the common bile duct (Fig. 5.11).
The minor ampulla is a similar, albeit much smaller nodular structure across the duodenal wall (Fig. 5.12). The overlying minor papilla is often no more than a 2–3 mm large elevation of the duodenal mucosa, which is typically located 10–20 mm proximal to the papilla of Vater. It drains the Santorini duct, which is very small (ca. 1 mm in diameter) and therefore not often seen (Fig. 5.12).
The gastroduodenal artery is the larger of both arteries that are included in a standard pancreatoduodenectomy specimen. It runs through the anterior peripancreatic adipose tissue before dividing into pancreatoduodenal branches (Fig. 5.11, see also Fig. 5.14). On external examination, the artery may be visible as a very short stump, often with a surgical suture, at the superior aspect of the pancreatic head.
The inferior pancreatoduodenal artery is the smaller of both arteries contained in a standard pancreatoduodenectomy specimen. It can been seen in the peripancreatic adipose tissue facing the SMA in axial specimen slices through the caudal half of the pancreatic head (Fig. 5.13). The artery forms often a small plexus with two or more vascular lumina.
In case of an extended surgical procedure with resection of the SMV or portal vein, the venous segment will obviously be found adherent to the SMV groove (Fig. 5.14).
In case of resection of the hepatic artery, the arterial segment will be found on the cranial aspect of the pancreatic head, close to the gastroduodenal artery (Fig. 5.15).
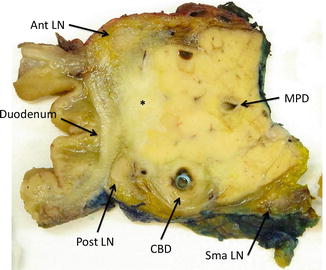
Fig. 5.10
Compared to the main pancreatic duct, the common bile duct has a thicker wall and lies more posterior in the pancreatic head. Note the presence of a plastic stent in the bile duct. Abbreviations: Ant LN anterior pancreatoduodenal lymph node, CBD common bile duct, MPD main pancreatic duct, Post LN posterior pancreatoduodenal lymph node, Sma LN lymph node in the adipose tissue facing the superior mesenteric artery
Fig. 5.11




The junction of the main pancreatic duct and common bile duct at the ampulla of Vater seen in three sequential (cranial to caudal) axial specimen slices (a–c). (a) Note the thicker wall of the common bile duct compared to the main pancreatic duct. (b) The distal common bile duct joins the ampulla, which is a slightly nodular structure. Note that the main pancreatic duct at this level has not yet joined the ampulla. (c) The main pancreatic duct joins the ampulla at a level that lies just caudal of the junction between the ampulla and common bile duct (as depicted in b). Note the dilatation of the main pancreatic duct due to a small ampullary tumour. Abbreviations: AMP ampulla of Vater, AMP TU ampullary tumour, CBD common bile duct, GDA gastroduodenal artery, MPD main pancreatic duct
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree