Keywords
Adenovirus, oncolytic, immunotherapy, patients, trials, ATAP, cancer, tumor, armed viruses
Overview of Oncolytic Adenoviruses
Gene therapy, as described in other chapters of this book, can be used in many different approaches for the treatment of cancer. This chapter discusses oncolytic adenoviruses, which infect tumors, replicate in them, and finally kill the tumor cells. Simultaneously, oncolysis generates antitumor immune responses, which seems to be important for the outcome. New progeny virions can further infect new tumor cells and circulate through the bloodstream even to distant metastatic tumors, provoking further immune responses. Treatment can be readministered multiple times, boosting the immune response. Using different viruses in a heterologous prime-boost scheme might further boost antitumor immunity while resulting in less antiviral immunity. The safety of adenovirus is good, as demonstrated by billions of infections of humans by wild-type adenoviruses and by thousands of patients treated with modified adenoviruses. The efficacy of the vectors can be further enhanced by adding, for example, immunostimulatory molecules to the virus DNA, which are then produced during virus replication. Adenoviruses have been one of the most popular vectors in gene therapy for reasons discussed later. Also in the field of oncolytic viruses, adenoviruses have been used in many different approaches. We begin this chapter by discussing the history of viruses, particularly adenovirus, and how they relate to cancer treatments. We then discuss why they have been so widely used. Then, we discuss different genetic modifications done to the virus to make it safer or a more potent oncolytic agent. Finally, we discuss ethics and how treatments can be applied to patients in Europe. We discuss the differences between clinical trials and patient treatments in the Advanced Therapy Access Program and include an overview of the program.
History of Viruses and Cancer treatment
The years leading up to the 20th century are traditionally considered as the beginning of modern medicine. Also in cancer therapy, new treatment modalities were introduced, prior to which basically the only cancer therapy was excision of the tumor by surgery. Anesthesia was becoming available, but surgery was still very primitive. Tumors that were superficial and easy to operate on could be removed, but relapses were often seen. As primitive chemotherapy, castor oil and arsenic were used. In 1895, radiotherapy was discovered and quickly adapted to the treatment of cancer. Despite these advances, cancer was seldom cured. Already at this time, it was occasionally observed that cancer patients who contracted an infectious disease experienced brief periods of clinical remission. During these same years, viruses were “discovered” as some agents that could pass through filters through which bacteria could not pass. Plaque assay was discovered in 1915, which gave some hints of the nature of viruses, and the first reports of electron microscopy are from 1939, initiating a period of better understanding. Ten years later, cell culture as a propagation method of viruses was becoming possible , and many viruses were shown to have an effect on tumors in rodent models . Since then, viruses in general and adenovirus in particular have been studied with a nearly unparalleled intensity, resulting in their biology now being understood more thoroughly than most other organisms in nature .
Observations
During the past 150 years, there has been a steady flow of case reports describing tumor regression of patients after natural virus infections (e.g., influenza, varicella, measles, hepatitis, and glandular fever) . These and other reports describe rare but sometimes dramatic responses in cancer patients recovering from viral syndromes. Most observations have been made with patients suffering from leukemia or lymphoma, known to be associated with significant immune suppression. Until recently, these were also the easiest tumors to diagnose and basically the only tumors for which treatment effects could be measured. Thus, these might be artificially overrepresented in historical case reports. Typically, the patients reported with responses have been young and the remissions have been short-lived, lasting for 1 or 2 months . These observations can be interpreted as follows: (1) Under the right conditions, certain viruses can destroy tumors without causing harm to the patient, and (2) in advanced disease, resistance can develop rapidly.
Implementation
On the basis of clinical observations, several viruses with low pathogenicity to normal tissue and high oncolytic capacity have been selected for clinical investigation . First attempts to treat cancer patients with viruses date back approximately 100 years . At this time, the virus was collected from heterogeneous and impure specimens from different plants, humans, or animals. During the first half of the 20th century, little was known of the biological nature of viruses, but still many viruses were used to treat cancer patients. The success and side effects of treatment varied, and the purity, quantity, and scientific standards were different from those of today.
Interest in the field has fluctuated, reaching an early peak in the 1950s and 1960s when clinical testing became more common and many different wild-type viruses (e.g., hepatitis, Epstein–Barr, West Nile, Uganda, dengue fever, and yellow fever) were used to treat different cancers. Intratumoral virus replication was often confirmed, but clear curative or survival-increasing responses were rare. After hundreds of clinical trials treating different cancers (e.g., with Egypt 101 virus—a type of West Nile virus—more than 150 trials against different cancer types ) with different wild-type viruses, it became clear that most wild-type viruses lacked efficacy or safety.
Some of the most promising results and acceptable side effects at this time were associated with adenoidal–pharyngeal–conjuctival (APC) virus , which is now known as the adenovirus. For example, in 1956, 30 women with advanced epidermoid carcinoma of the cervix were treated with adenovirus . The virus was administered via intra-arterial, intravenous, or intratumoral routes. In two-thirds of the cases, within 10 days, necrosis was observed, and most remarkably, it appeared to be restricted to the cancerous tissue. No safety problems were reported with the use of this wild-type virus. In the 1970s and 1980s, the regulatory aspects of clinical trials with living pathogens became stricter. More important, the arsenal of drugs based on chemistry was expanding exponentially, resulting in a belief that cancer would soon be cured. Thus, there seemed to be little need for difficult-to-handle and tricky-to-produce bugs, which might be one of the reasons why the field was nearly abandoned. For the past two decades, oncolytic viruses have again gained increasing interest as advances in molecular biology, tumor biology, immunology, and virology seem to suggest that oncolytic viruses might be an untapped resource in cancer therapy. The first marketing approval of an oncolytic virus, granted by Chinese regulators in 2005, was for the genetically modified oncolytic adenovirus H101, a relative of ONYX-015 tested previously in the West.
Adenoviruses in Cancer Gene Therapy
There are several reasons why adenoviruses are popular in gene therapy. As mentioned previously, adenoviruses were found to be naturally oncolytic, and even the wild-type replicating viruses were found to be safe in several human trials and live virus vaccinations after the isolation of adenovirus (Ad) serotypes in 1953 and 1954 . Subsequently, large doses of wild-type or modified adenoviruses have been administered to patients or volunteers, including multiple injection strategies, suggesting safety. Likewise, with mounting clinical experience, virus shedding or latent infections have not been a concern. During the past few decades, adenovirus has been examined in great detail. Its replication and effect on host cells as well as the effect on host immune systems have been reported in hundreds of publications. In molecular biology research, the virus has been used as a model organism to study DNA replication, apoptosis, oncogenic transformation, and mRNA processing . Adenovirus is known to be easily produced in large quantities, easy to manipulate, and genetically stable. Integration into the host genome is rare, which has been considered important for safety reasons. The biology of natural adenovirus infections in humans is reasonably well understood .
First-Generation, Replication-Deficient Adenoviruses
The first application of Ads in cancer gene therapy was their use as replication-deficient vectors to transfer specific transgenes to the malignant cells . This was found to be one of the most efficient ways to express transgenes compared to any other viral or nonviral vector. Adenovirus could transfect a wide variety of cells, both replicating (e.g., cancer cells) and nonreplicating (e.g., normal tissues and cancer stem cells). Transgene expression, however, was found to be transient and often insufficient to generate a significant therapeutic effect. Thus, there was a need for more potent vectors to treat cancer.
Second-Generation, Oncolytic Adenoviruses
Once tumor transduction was recognized as the critical obstacle to cancer gene therapy, the oncolytic platform gained in popularity due to the ability for intratumoral amplification and penetration. For safety reasons, oncolytic viruses are modified (or biologically selected) so that they preferentially replicate and lyse cancer cells. In theory, the virus would replicate and lyse the tumor cells, and the progeny virions would find new cancer cell hosts until no tumor was left. There are several ways of making a virus oncolytic, most of which utilize defects in certain signal transduction pathways: (1) Replace essential virus promoters with promoters that are active mainly in tumor cells (e.g., hTERT and E2F1); (2) delete parts of the viral genome (e.g., 24-bp deletion in the E1A) that are responsible for freeing E2F, necessary for driving infected cells into S-phase, which is a requirement for virus replication (this function is not necessary in tumor cells defective in the Rb/p16 pathway, including most, if not all, tumors); and (3) remove viral genes that prevent premature apoptosis of infected cells (these genes are commonly inactive in cancer cells). Oncolytic adenoviruses show generally efficient cell killing in vitro and good potency in vivo . In cancer patients, they have shown some signs of efficacy, but complete cures are rare.
Third-Generation, Oncolytic and Armed Adenoviruses
Because the safety and tolerability of oncolytic adenoviruses appear good compared to those of traditional cancer treatments (surgery, chemotherapy, and radiation) but the efficacy requires improvement, a need for more effective viruses has become clear. Scientists throughout the world have produced multiple approaches in arming the viruses with anticancer transgenes. Most commonly, these transgenes have been inserted either in E1 or in a deleted E3 region of the virus. An appealing variant of the latter strategy is placing the transgene under the native E3 virus promoter, resulting in transgene production in the early or late phase of Ad replication as defined by the alterative splicing of this area . With this approach, most E3 genes can be retained, which may be appealing from the standpoint of optimal oncolysis, spreading, and immunological aspects. As an option, the transgenes can be placed under a strong constitutive promoter (e.g., CMV), cancer-specific promoters (e.g., hTERT and E2F), or some inducible foreign promoters (e.g., tetracycline). The several therapeutic molecules can be grouped by function, as done here. Although many strategies have focused on potentiating direct cell killing by various methods, the authors believe that training the immune system to attack the malignancy is a more intelligent way to fight cancer.
Immunomodulatory Oncolytic Adenoviruses
In recent years, it has become clear that evading the immune system is one of the crucial tasks cancer must accomplish before it can thrive . Although the immune system plays a major role in destroying cancer cells, it also helps to pick the most suitable cancer cells to survive and helps establish conditions within the tumor microenvironment that facilitate tumor outgrowth . In this immunoediting process, cancer cells use multiple mechanisms. For example, they secrete immunosuppressive cytokines, recruit regulatory T cells, downregulate major histocompatibility class I molecules, and express Fas ligand to kill reactive cytotoxic lymphocytes. Thus, the tumor microenvironment is highly immunosuppressive and left unaffected by the immune system, even if the tumor presents potentially immunogenic antigens . There is increasing evidence that arming oncolytic Ads with certain immunomodulatory molecules may help break the tolerance acquired by the tumor . It seems that infection with Ads elicits a strong inflammatory immune response—a “danger signal”—that may overcome the immunosuppression ( Figure 11.1 ). Immunomodulatory molecules may enhance the antitumor immune reaction.
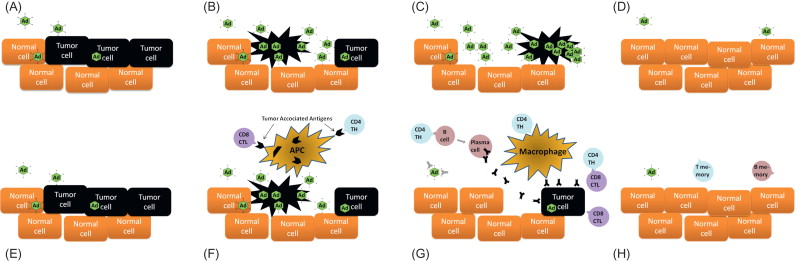
Granulocyte–macrophage colony-stimulating factor (GM-CSF) seems to be one of the most promising cytokines. For example, Ad5-D24-GMCSF (serotype 5 Ad-based oncolytic adenovirus coding for GM-CSF) was used to treat immunocompetent Syrian hamsters that had subcutaneous hamster pancreatic cancer. Tumors were eradicated, and antitumor immunity indicated that these hamsters did not grow new pancreatic tumors even after new cancer cell injections . Later, this virus was used in patients in the Advanced Therapy Access Program (ATAP) (described later) and demonstrated good safety and promising results.
Another immunostimulatory molecule-armed oncolytic virus used in patients codes for CD40L . Immunomodulatory viruses with promising in vitro and in vivo data include the following: aCTLA-4 activating cytotoxic T cells ; RANTES for recruiting immunological cells ; interferon (IFN)-α , IFN-β , and IFN-γ to induce proinflammatory effect; Fas ligand, interleukin (IL)-27, and hsp70 chaperone to assist antigen presentation ; and IL-24, IL-12, and B7-1 to enhance the immune response . Although many of these have not yet been tested in the clinic, the hsp70-expressing virus has recently been taken to a phase I trial .
Vector Spread Enhancing Oncolytic Adenoviruses
Clinical tumors are complex, and especially the stromal areas of the tumor pose several obstacles for effective virus penetration. To make the tumor microenvironment more permeable for Ads, a relaxin-producing Ad has been generated. Relaxin increases the production of certain matrix metalloproteases and decreases the production of collagen, helping virus spread . Also, Ads expressing ADP or Ads without the E3 gp19k gene have been made. These were shown to speed up the virus release from the Ads in vitro and in vivo . An interesting experiment engaged a fusiogenic protein from an enveloped virus that caused the infected cell to fuse with neighboring cells .
Prodrug-Converting Enzymes Producing Oncolytic Adenoviruses
These viruses produce enzymes (thymidine kinase, cytosine deaminase, and nitroreductase) that convert nontoxic prodrugs to active forms. In this way, the oncolytic activity is further enhanced by a bystander effect caused by the toxic product when the systemically given prodrug is administered. Thymidine kinase has been of special interest because its effect can also be seen by positron emission tomography (PET) or single-photon emission computed tomography . Timing of the administration of the prodrug is critical because it will typically destroy the virus and terminate the treatment. Administration of this “suicide gene” may also be regarded as a safety procedure. Ad5-CD/Tk rep is the first from this group to be tested in humans , and it is being evaluated in a randomized phase III trial in first-line treatment of prostate cancer in combination with radiation therapy .
Direct Antitumor Effect Producing Oncolytic Ads
Many oncolytic Ads coding for apoptosis-inducing genes such as TRAIL , TNF-α , and Fas ligand have been made. The secreted protein can kill uninfected cells, causing a bystander effect, but this may hinder the spread of the virus.
Anti-Angiogenic Oncolytic Ads
Tumor neovasculature is a hallmark of cancer . Ads are naturally targeted to newly formed blood vessels. Ample α v β 3 integrins are found in the neovasculature , and these are one of the coreceptors for Ads. Thus, some of the viruses used in ATAP also target integrins. The antitumor effect has been further enhanced by creating oncolytic anti-angiogenic Ads expressing anti-vascular endothelial growth factor (VEGF) or endostatin .
Other Ways of Enhancing the Potency of the Virus
Combination Therapy
Combining armed oncolytic Ads with existing and new treatment modalities seems to be a feasible approach. Multiple preclinical studies have been conducted to evaluate the best combinations of Ads and chemotherapeutics, radiation therapies, surgery, and antibody-based therapies. In addition, several clinical trials have been started or are being planned to assess this important question.
Using Different Cell Surface Receptors
Targeting Ads to different cell surface receptors is called transductional targeting. All species C (serotypes 1, 2, 5, and 6) Ads and most other Ads use coxsackie–adenovirus receptor (CAR) as a primary attachment receptor. The majority of research has been done with serotypes 5 and 2 Ads, which both use CAR as the primary receptor. CAR is expressed in a wide variety of cells, but in many advanced cancers it seems to be downregulated . Another conceptual issue with CAR is that it seems to be located below the tight junction, facilitating lateral spread, but it is not clear how Ad initially reaches CAR from the epithelial surface . In vitro , many other receptors (most of which are lower affinity) for adenoviruses have been found .
Some species B Ads have been of growing interest because they use other high-affinity receptors besides CAR, and these receptors seem to be widely expressed in advanced human tumors . Research performed during the past few years seems to indicate that these receptors are CD46 and DSG-2 (although CD80/86 have also been suggested ). Thus, the serotype 5 adenovirus knobs have been changed with serotype 3 knobs to make the Ad5/3 virus bind better to cancer cells . Many oncolytic forms of this construct have been used successfully in ATAP patients . Inspired by the positive results associating with this approach, an oncolytic adenovirus based on serotype 3 was made . Using an entirely new serotype offers escape from Ad5 antibodies and an alternative immunological response. After promising preclinical results, 25 advanced cancer patients were treated safely and with mild adverse events. More than two-thirds of the patients presented some objective evidence of anticancer activity —a result considered excellent for an unarmed virus.
Another approach, also used safely in patients, features arginine–glysine–aspartate (RGD) modification of the fiber to target α v β integrins highly expressed in advanced tumors. Also, other targeting modifications have been used in preclinical models .
Chemical modifications of Ads can result in altered tropism as well. Here, the virus is coated with a hydrophilic polymer, most often polyethene glycol (PEG) or poly- N -(2-hydroxypropyl)methacrylamine (pHPMA) . This shield protects against antibodies, and it can be further coupled with ligands for tumor-associated receptors (e.g., VEGF). However, progeny virions are left unshielded. Although several other serotypes, fiber knob modifications, Ads with specific peptide ligands in their capsid proteins, and coated Ads have been made, it has been difficult to predict their binding to desired cells . Also, no clinical data on these vectors exist.
Following intravenous delivery in mice, many adenoviruses feature mainly transduction to the liver. In contrast to in vitro data, in vivo coagulation factor X, and its binding to both Ad5 hexon and hepatocytes, seems more important than the “primary” receptors . With humans, liver toxicity has not been a problem, although large intravenous doses of oncolytic adenoviruses have been administered , suggesting key differences between different species. It is not known if humans display liver tropism similar to mice. If present, it might affect antiviral efficacy through virus clearance from blood. In summary, it seems that preclinical in vitro and in vivo receptor studies correlate poorly with the available human data.
Using Alternative Physical Delivery Methods
The complex architecture of the tumor prevents spreading of the virus through the tumor and therefore multiple ways to circumvent this problem have been tried. Performing multiple injections of the virus around the tumor is one way of helping the virus spread . Another way is to inject the virus to the artery leading to the tumor . Intravenous injection of adenovirus seems to be feasible as well, especially if the amount of neutralizing antibodies is low or the amount of virus is high . Intracavitary injection to treat bladder or ovarian cancer, for example, is also a good way to increase the local concentration of virus . Using mesenchymal stem cells as delivery vehicles is another way of transferring the virus to the cancer. These cells can be efficiently infected with Ads, and they have been shown to home to tumors after intravenous injection , although not all studies are in agreement .
Preventing the Antiviral Immune Response
It has become increasingly clear that the immune response is very important in oncolytic adenovirus treatments, and the Syrian hamster is becoming an increasingly popular model in the field. For unknown reasons, the human adenovirus can replicate to some degree in this immunocompetent model. Oncolytic effect can be potentiated by using immunosuppressed Syrian hamster models, but at the same time the ability to raise antitumor immunity is disabled and the net result might be negative. In general, there is lack of agreement regarding whether the immune response is friend or foe in the context of oncolytic adenovirus therapy, and it could be both or either, depending on the model, virus, transgene, and outcome variable. With regard to human data from ATAP, immunity seems to be important with regard to efficacy , but there are also case examples in which lack of neutralizing antibody induction coincided with the disappearance of tumors . Thus, the consequences of immune response may vary from patient to patient.
Bioselection of New Oncolytic Adenoviruses In Vitro
Gain-of-function mutations in the viral genome can lead to better anticancer agents. One way to do this is to amplify virus in the presence of mutagens or to pool different serotype viruses together and grow them at low multiplicity on different cancer cells. After serial passages, viruses with better anticancer abilities (in this in vitro cell line) outgrow other variants. One such experiment resulted in an Ad3/Ad11 chimera with promising oncolytic features , suggesting the potential of subgroup B viruses. Similarly, any oncolytic adenovirus could be incubated at low multiplicity on cancer cell lines, and viruses with attractive oncolytic abilities on these in vitro cells could be harvested. Whether such viruses correlate with clinical safety or potency obviously needs to be addressed, and this information may be obtainable only in humans.
Avoiding Overattenuation
Drastic modifications of the virus genome may seem appealing for enhancement of safety but could compromise potency. Building on the safety record of wild-type adenovirus injections performed in the 1950s , it has been proposed that using wild-type adenovirus (which has some innate tumor selectivity) or an armed virus without tumor selectivity mechanisms might be safe . The U.S. Food and Drug Administration (FDA) has permitted this hypothesis to be tested in a phase I clinical trial for intratumoral injection into solid tumors of any indication.
Evaluating the Efficacy of Oncolytic Viruses
A clear discrepancy in efficacy between tissue culture, animal experiments, and human patients has been observed as long as Ads have been used to treat cancer. Even when a particular virus effectively kills a given cell line, the results observed in vivo can be contradictory. Multiple factors are believed to cause this phenomenon :
- 1.
Lack of a primary Ad attachment receptor on tumor cells in situ.
- 2.
Partially unknown innate host defense mechanisms that recognize Ads as pathogens and shut down Ad replication in vivo , making tumors resistant to further virus injections .
- 3.
Virus spread in the tumor is limited due to the three-dimensional structure containing fibrotic stroma, necrotic, hypoxic, and low-pH areas of tumors as well as the epithelial phenotype containing tight and adherens junctions of cancer cells. Even the mere size of virus particles, compared to many chemical drugs, could present a problem for intratumoral spread.
- 4.
Regarding immunocompetent animals or patients, the adaptive immune system could also play a role in elimination of virus within weeks.
- 5.
Clinical treatments usually have been applied to terminal patients with advanced disease and a history of multiple rounds of cancer treatments. These cancers have evolved for years, developing thousands of mutations needed to avoid the multiple ways of the body to eliminate cancerous tissues. This is in great contrast with the cancers implanted in murine models and grown for a few weeks.
Thus, it has become clear that immunocompromised (e.g., SCID or nude mice) animal models with injected human cancer cell lines or immunocompetent animals (e.g., Syrian hamsters) with hamster cancer are poor prognostic models for advanced human cancers.
Clinical Studies with Oncolytic Adenoviruses
Despite remarkable advances in the prevention, diagnosis, and treatments of cancer, the incidence has been continuously increasing and cancer is now the most frequent cause of mortality in the Western world. With some exceptions, curative treatments are not available for most metastasized solid tumors. Many treatments result in only a minor increase in the time of survival, and many cause severe side effects. Every day, tens of thousands of people—some of whom are working age—die of this disease. Thus, it is obvious that there is an urgent need for new treatments. Oncolytic viruses present a strong rationale and an untapped approach for cancer therapy. Also, synergy with other treatment modalities has been suggested in numerous preclinical studies , and even some clinical data indicating synergy with other modalities are available.
Trials
The vast majority of clinical trials conducted with oncolytic Ads have been phase I dose-escalation studies designed to assess the safety of the treatment . Several oncolytic adenoviruses have appeared safe and no dose-limiting toxicities or maximum tolerated doses have been reached in most clinical trials. Instead, the highest dose used has typically been set as the maximum feasible dose for further studies. Also, adverse events have typically been mild and self-limiting, although the nonlinear toxicity of adenoviruses is given due respect in the field . Generally, it has been thought that the efficacy of the unarmed oncolytic Ads has been modest when used as a single modality. However, traditional size-based surrogate endpoints might not be good for evaluating the efficacy due to the swelling caused by inflammation resulting from virus replication and/or transgene expression . Also, efficacy has not been the primary endpoint in most trials because only a few trials higher than phase I/II have been performed. Here, we describe briefly some interesting phase I/II clinical trials, all of which have been performed with serotype 5 adenoviruses without capsid modifications. All of them suggest safety, and signs of efficacy can be noted in most.
ONYX-015 (Also Known as dl1520 or CI-1042; Similar Constructs Include H101 (Oncorine))
Originally described as dl1520 , a patient isolate, ONYX-015 was the first adenovirus identified in the second emergence of oncolytic viruses occurring during the 1990s. It was tested in a dozen phase I and II trials, but it was never included in a randomized study. It is a serotype 5-based oncolytic adenovirus for which several possible selectivity mechanisms have been proposed, including p53/p14ARF defects and aberrant late mRNA transport, both of which may relate to the absence of the E1B-55 K gene. Although the deletion of this gene provides attenuation and some specificity to tumors, it is by default also able to replicate in normal tissues because it was isolated from a non tumor-bearing host. ONYX-015 has gone though many phase I and phase II clinical studies in a variety of indications . The use of this adenovirus vector has been proven safe, even when high (3×10 11 plaque-forming units) intravenous injections were used. The efficacy data of these trials are moderate when evaluated by classical evaluation criteria. In part, this could be due to suboptimal criteria used in efficacy evaluation, but the attenuation of the virus could also contribute to low potency. In the original publication describing dl1520, the strain is reported as severely crippled in comparison to wild type .
Some of the most interesting data come from patients with colorectal liver metastases treated with an injection of ONYX-015 into the hepatic artery with the combination of 5-FU/leucovorin intravenously. This resulted in tumor regression in 46% of the patients, and the median survival increased to 19 months from the expected 4–6 months. Interestingly, some patients first showed enlargement of the tumors, whereas regression was seen later . This initial swelling is reported as progressive disease with classical evaluation criteria that might underestimate underlying therapeutic effects, as subsequently described for ipilimumab (anti-CTLA4 antibody) . In this particular ONYX-015 trial, the inside of these swollen tumors was reported to be necrotic, and this could be observed with PET/computed tomography (CT). This and other observations suggest that multimodal following is useful for oncolytic viruses. With regard to immunologically armed oncolytic viruses, this effect is probably even more prominent than with unarmed viruses or “passive” immunotherapy with anti-CTLA4 antibodies.
However, tumor size is only a surrogate endpoint (used in lieu of survival), and interpretation of nonrandomized data is famously difficult. Thus, it was satisfying to see Shanghai Sunway Biotech employ H101 (a closely related although distinct virus from dl1520) in a randomized phase III trial , which resulted in approval of Oncorine by the Chinese FDA in 2005 for the treatment of head and neck squamous cell carcinoma.
Ad5-CD/Tk rep
Ad5-CD/Tk rep is the first replication-competent adenovirus vector that expresses a therapeutic gene to be tested in humans . Ad5-CD/Tk rep is replication selective because it contains the same E1B-55K gene deletion as ONYX-015. The virus expresses a cytosine deaminase (CD) and herpes simplex virus thymidine kinase (TK) fusion gene to allow for therapeutic treatment with both 5-FC and ganciclovir. In a 5-year follow-up report of a phase I trial in human prostate cancer, the prostate-specific antigen (PSA) doubling time increased following the gene therapy from a mean of 17 to 31 months ( p =0.014). This postponed the salvage androgen suppression therapy (which is associated with high morbidity) by an average of 2 years with good safety. Thus, this approach may provide an attractive treatment option for patients experiencing PSA relapse following definitive therapy . This virus is now being tested in a randomized phase III study in first-line therapy of prostate cancer in combination with radiation .
CG7060 and CG7870 (Also Called CV706 and CV787)
CG7060 is a serotype 5-based PSA-selective replication-competent adenovirus indicated for use in prostate cancer. A single phase I clinical trial with CG7060 has been reported. In this trial, 20 patients in five dose cohorts (1×10 11 to 1×10 13 viral particles) were treated with an intraprostatic injection. All 5 patients who achieved 50% reduction in PSA were treated with the highest two doses of the vector. This treatment was found safe, and efficacy was suggested .
CG7870 is another serotype 5-based vector that is intended for use in prostate cancer. Previously, the vector was found safe and well tolerated in a phase I/II clinical trial of intraprostatic delivery for locally recurrent prostate cancer. Next, the CG7870 was administered as a single intravenous infusion in a dose-escalation design (1×10 10 to 6×10 12 viral particles) to 23 patients with hormone-refractory metastatic prostate cancer. Flu-like symptoms were commonly observed. No partial or complete PSA responses were observed; however, 5 patients had a decrease in serum PSA of 25–49% following a single treatment, including 3 of 8 patients at the highest dose levels .
Telomelysin (Also Called OBP-301)
Telomelysin is a human telomerase reverse transcriptase (hTERT) promoter-driven serotype 5 oncolytic adenovirus. One phase I clinical trial was conducted in patients with advanced variable solid tumors. A single intratumoral injection of telomelysin was administered to three cohorts of patients (1×10 10 , 1×10 11 , and 1×10 12 viral particles). All doses were well tolerated. One patient had a partial response of the injected malignant lesion. Seven patients (of the 16) fulfilled Response Evaluation Criteria in Solid Tumors (RECIST) definition for stable disease at 2 months after treatment. Postinjection biopsies performed on Day 28 on 4 of the patients with stable disease revealed necrosis of the tumor. One patient (No. 308) had a 33% reduction of injected lesion on Day 28 and 56.7% reduction of injected lesion on Day 56. Hence, antitumor activity was also indicated .
H103
H103 is a serotype 5-based oncolytic adenovirus similar to H101 and ONYX-015, but it expresses heat shock protein (HSP)70, which is suggested to be important in antigen presentation and activation of the immune system. A phase I clinical trial of intratumoral injection of H103 was conducted in 27 patients with advanced solid tumors. Injections were performed in a dose-escalation manner from a dose of 2.5×10 7 to a dose of 3.0×10 12 viral particles. Treatment was well tolerated. The objective response (complete response+partial response) to H103-injected tumors was 11.1% (3/27), and the clinical benefit rate (complete response+partial response+minor response+stable disease) was 48.1%. Partial transient regression of distant, uninjected tumors was also noted in 3 patients .
Advanced Therapy Access Program
ATAP was set up to offer oncolytic virus treatments to patients who did not have access to clinical trials ( Table 11.1 ) . It is based on the European Commission Advance Therapies Regulation (EC/1394/2007), which determines rules for patient-by-patient use of gene therapy and cell products. On the one hand, the goal was to apply regulation in an area where it had been absent previously. On the other hand, scientific and medical progress was encouraged. In ATAP, each patient is monitored for safety, efficacy, and survival. All data are reported in peer-reviewed journals and to the Finnish FDA (FIMEA). Although new drugs always entail a certain risk factor, ATAP attempts to balance this against the risk of death posed by incurable and progressing tumors.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Overall, 10 different viruses were used in a total of 290 patients who had disease that was incurable with current therapies. The typical patient had a tumor progressing after all routine therapies had been exhausted. Each of the 821 treatments was individually designed, typically employing intratumoral injection in ultrasound or computer tomography guidance. Intrapleural, intraperitoneal, and intravenous injection were also used depending on the location of each patient’s tumors.
Patients in ATAP
The patient population in ATAP resembles a typical phase I population in that patients have incurable advanced solid tumors progressing after routine treatments, and in fact most patients have gone through multiple regimens of chemotherapy ( Table 11.2 ). Patients sign informed consent. After treatment, patients are monitored 24 hr in the hospital and thereafter as outpatients. As required by the philosophy of individualized therapy, each patient was treated according to our best knowledge, taking into account what we knew about their disease, what we had learned about our viruses in the laboratory and in animals, and—probably most important—what we had learned from previous patients. Each patient taught us something, and sometimes one patient taught us more than 1000 mice. ATAP had two goals (in order of importance): (1) trying to help the patient and (2) allowing us to learn about the technology as we used it.
| Mean age | 60 years |
| Female | 14 |
| Male | 11 |
| Cancer type | |
| NSCLC | 7 |
| Breast | 5 |
| Sarcoma | 4 |
| Pancreatic | 3 |
| Prostate | 2 |
| Bladder | 1 |
| Neuroblastoma | 1 |
| Ovarian | 1 |
| Thyroid | 1 |
| WHO performance scale | |
| 0 | 1 |
| 1 | 15 |
| 2 | 8 |
| 3 | 1 |
| Median | 1 |
| Previous chemo regimens | |
| Range | 1–7 |
| Median | 3 |
| Previous oncolytic adenovirus treatments | |
| None | 12 |
| 1–2 treatments | 7 |
| 4–6 treatments | 6 |
a Shown are data from Ad3-hTERT-E1A-treated patients as reported by Hemminki e t al .
Viruses in ATAP
All viruses used in ATAP are designed to work in most tumors, and they are second- or third-generation viruses—hence replication competent—and some are also armed. Each virus was carefully tested preclinically before patient treatment ( Table 11.3 ). All of these viruses were designed so that replication takes place primarily in tumor cells (hTERT, Cox2, and E2F promoters or D24 deletion, or a combination thereof). These modifications make the viruses more safe . However, it was quickly discovered that the safety in patients with all constructs was good, and it also became clear relatively quickly that oncolysis alone was unlikely to cure patients with advanced tumors. Thus, improving selectivity seemed less critical than improving efficacy. Therefore, we rapidly moved to armed viruses and utilization of drugs such as low-dose cyclophosphamide—useful for counteracting regulatory T cells—to enhance efficacy.
| Virus | Serotype | Targeting | Tumor Specificity | Arming |
|---|---|---|---|---|
| Ad5-D24-GMCSF | 5 | CAR | 24-bp deletion in E1A b | GMCSF |
| Ad5-RGD-D24 | 5 | Integrins | 24-bp deletion in E1A b | No |
| Ad5-RGD-D24-GMCSF | 5 | Integrins | 24-bp deletion in E1A b | GMCSF |
| ICOVIR-7 | 5 | Integrins | E2F1 promoter and 24-bp deletion in E1A b | No |
| Ad5/3-Cox2L-D24 | 5 | Partly DSG-2 a | Cox2L promoter and 24-bp deletion in E1A b | No |
| Ad5/3-D24-GMCSF | 5 | Partly DSG-2 a | 24-bp deletion in E1A b | GMCSF |
| Ad5/3-hTERT-hCD40L | 5 | Partly DSG-2 a | hTERT promoter c | CD40L |
| Ad5/3-E2F1-D24-GMCSF | 5 | Partly DSG-2 a | E2F1 promoter and 24-bp deletion in E1A b | GMCSF |
| Ad5/3-D24-hNIS | 5 | Partly DSG-2 a | 24-bp deletion in E1A b | hNIS |
| Ad3-hTERT-E1A | 3 | DSG-2 | hTERT promoter c | No |
a In vitro studies suggest that changing only the serotype knob is not enough to get high-affinity binding to DSG-2 .
b Replication in cells with a deficient Rb/p16 pathway (a hallmark of cancer).
c Replication in cells with active telomerase (a hallmark of cancer).
Different modifications to the virus capsid were done to achieve better transduction of tumor cells because downregulation of CAR is suggested as a problem in oncolytic virus treatments . Some of the viruses were targeted to integrins and some to the Ad3 receptor by changing the knob of the Ad5 virus fiber to an Ad3 knob (Ad5/3 viruses). Integrins and serotype 3 receptors (DSG-2) are suggested to be abundant in patient tumor tissues, and thus better efficacy with these viruses was anticipated. Finally, a completely serotype 3 oncolytic adenovirus (Ad3-hTERT-E1A) was made to avoid anti-Ad5 immunity and to achieve stronger binding to DSG-2. Good results associated with this unarmed virus seem to suggest that Ad5 might not be the only feasible serotype for cancer therapy. A particularly attractive aspect of DSG-2 binding is the synergy with monoclonal antibodies . Our preliminary patient data seem to corroborate the notion that this would be interesting for formal testing (see Table 11.6 ; patients treated with concomitant trastuzumab).
Adverse Reactions
Adverse reactions of all treated patients were collected ( Table 11.4 ). Typically, the patients presented flu-like symptoms that alleviated by themselves within several days. Injection site pain and leukocytopenia were also commonly observed. The latter, and particularly “lymphopenia,” may in fact reflect redistribution of white blood cells from the blood to target organs including tumors, and it is thus not an adverse event but in fact part of the mechanism of the therapy. A mild decrease in hemoglobin observed on the next day was thought to relate to the fluids that the patients received after treatment. Another possible explanation is that the virus binds to erythrocytes and some of them are subsequently cleared by the reticular endothelial system . In contrast to high-dose administration in animal models, liver enzymes were seldom elevated. In general, treatments were found safe and well tolerated.