Fig. 1
Anterior tissue biopsy should be performed to obtain tissue along the anterior capsule. For random biopsy, a needle should be advanced about 1.5 cm from the anterior capsule
In recent years, multiparametric MRI has been shown to detect prostate cancer previously not found by random needle biopsy. Those lesions are commonly located at the anterior part of the gland [10–12]. Urologists are asked to biopsy the anterior lesion more and more based on MRI findings (Figs. 2 and 3). Anterior cancer is commonly located along the capsule of the prostate. In order to obtain a useful sample of the anterior lesion, the biopsy needle must be advanced up to the edge of the lesion prior to triggering the automated biopsy device button. The biopsy needle is designed to take 15 mm tissue from the tip of the needle. However, it advances 23 mm from the needle tip. Biopsy of the anterior lesion, especially when located at the base of the gland, frequently results in the needle penetrating through the bladder wall due to the extra needle advancement (Fig. 4). This may result in significant hematuria. Careful observation of the biopsy site often shows the extent of the bladder wall bleeding. Mild oozing without pulsating bleeding seen by ultrasound generally stops by itself. However, persistent pulsating and pumping bleeding seen on ultrasound may need attention (Fig. 5). If bleeding persists after a few minutes of observation, a Foley catheterization with mild traction may be necessary to monitor and control the bleeding.

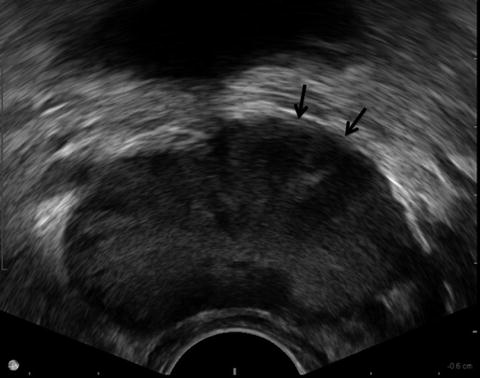

Fig. 2
A 57-year-old man with PSA of 17. Two previous biopsies showed no evidence of cancer. T2 weighted MR image showed a low signal intensity area suspicious for cancer at left anterior base of the prostate (arrows)
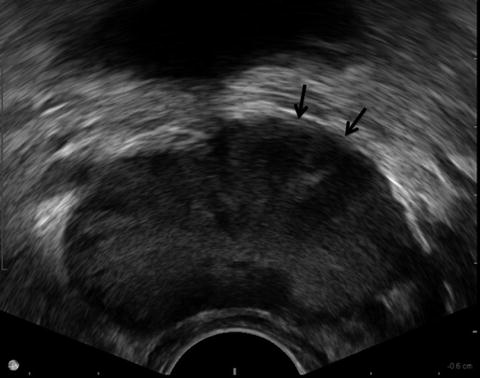
Fig. 3
Same patient on TRUS, a hypoechoic area was seen at left anterior base (arrows)
Fig. 4
In order to take an anterior base lesion, a biopsy needle has to be advanced just before the target area. Generally, the biopsy needle advances beyond the capsule and often results in penetration of the bladder wall
Fig. 5
Observation of the puncture site of the bladder wall by TRUS after biopsy is important. Pulsating bleeding can be seen if a small artery is injured
Midline Lesion Biopsy
A midline lesion may be missed by random biopsy, since a biopsy is commonly not taken from midline tissue. However, cancer can be found over the midline (Fig. 6). Biopsy of the midline, especially at the apex, is delicate because the biopsy needle may penetrate the urethra in a sagittal plane biopsy. In this setting, biopsy can be performed in transverse view and the biopsy needle can be obliquely inserted in the midline apical nodule in order to prevent urethral injury (Fig. 7). The same strategy can be used for anterior midline lesion found on TRUS or MRI. Again, biopsy of the anterior midline lesion in sagittal view requires the needle to penetrate the urethral lumen. In order to avoid urethral injury, biopsy should be done in transverse view to avoid the needle entering into the urethral lumen (Fig. 8).
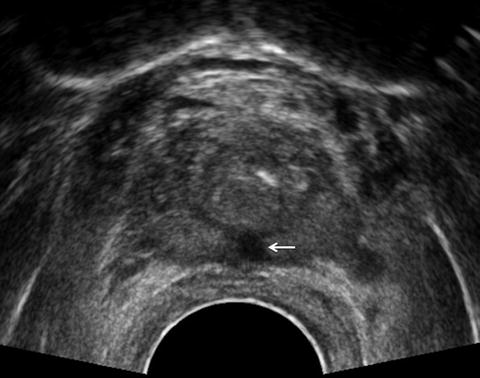
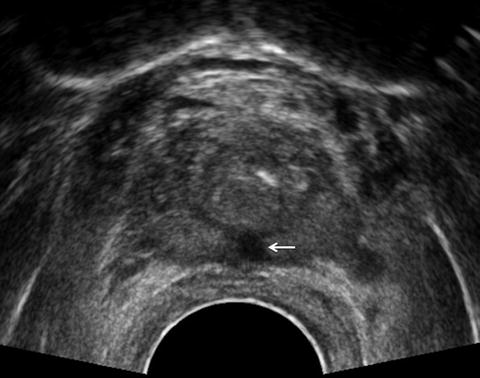
Fig. 6
A 55-year-old man with previous biopsy by referring urologist showing 1 mm focus of Gleason grade 3 + 4 cancer. TRUS revealed a hypoechoic area over the midline at apex (arrow)
Fig. 7
A hypoechoic area over the midline at apex can be biopsied in transverse view in order to avoid urethral puncture
Fig. 8
A lesion anterior to the urethra can also be biopsied in transverse view in order to avoid urethral penetration
Extraprostatic Tissue Biopsy
Seminal Vesicle Biopsy
Routine seminal vesicle biopsy is usually not necessary. However, patients with significant disease found at the base of the prostate or abnormal seminal vesicle appearance should undergo seminal vesicle biopsy. Seminal vesicle abnormality is not apparent in patients previously treated with radiation therapy, but risk of seminal vesicle invasion is high for patients with local failure after radiation therapy [13]. In this population, seminal vesicle biopsy should be performed regardless of findings. In order to obtain a meaningful pathology specimen, the base of the seminal vesicle near the junction of the prostate should be biopsied, since tumor invasion always occurs from the base. In order to avoid confusion between cancer in the prostate next to seminal vesicle and seminal vesicle invasion, the needle tip must be advanced against the seminal vesicle base before taking the biopsy (Fig. 9).
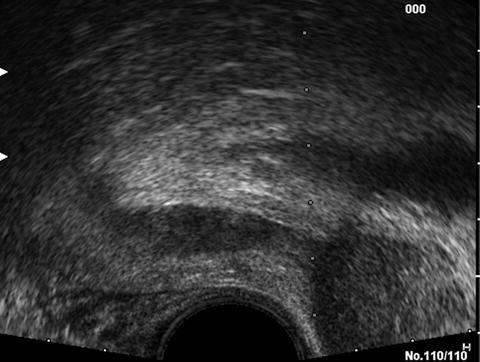
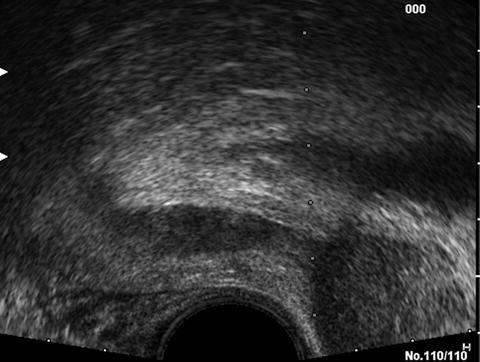
Fig. 9
Biopsy of the seminal vesicle should be aimed at the base of the seminal vesicle. Biopsy of the base of the prostate should be avoided
Bladder Neck Biopsy
In patients with locally extensive disease or patients with local recurrence after radiation therapy, bladder neck invasion can be observed on TRUS. If histological confirmation is necessary, the tissue diagnosis can be made by TRUS-guided biopsy of the bladder neck rather than cystoscopic biopsy (Fig. 10). A needle must be advanced right up to the suspicious tissue at the bladder neck; then the biopsy gun should be triggered. As with a base anterior lesion biopsy, the needle always penetrates the bladder mucosa. Careful observation of bladder wall bleeding from the biopsy site by TRUS is necessary.
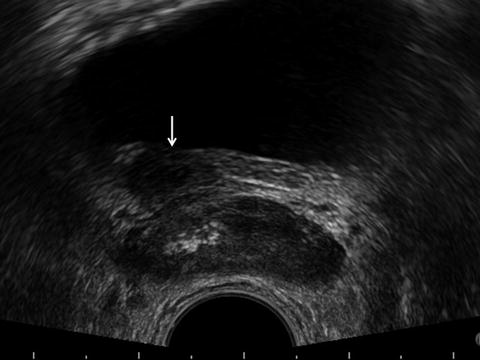
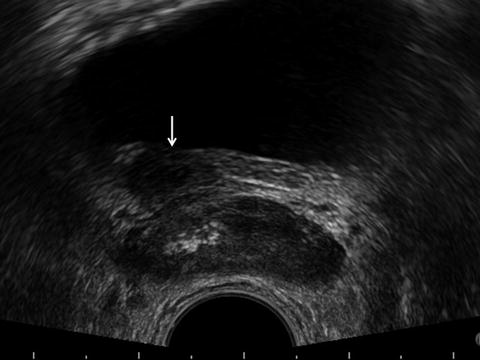
Fig. 10
A 49-year-old man status post radiation therapy for Gleason grade 4 + 5 cancer 3 years ago presented with rising PSA. TRUS revealed a mass extending from the right lobe of the prostate to the bladder neck (arrow). In order to biopsy this tissue, a needle has to be advanced beyond the prostate gland
Periprostatic or Rectal Lymph Node
For advanced disease or post radiation patients with biochemical failure, sometimes enlarged lymph nodes can be seen in the perirectal space or periprostatic tissue. If it is noted, biopsy of the lymph node can be performed (Figs. 11 and 12). However since large pelvic vessels may be nearby laterally, only lymph nodes in a safe area, such as anterior to the prostate or posterior to the rectum, should be biopsied transrectally.

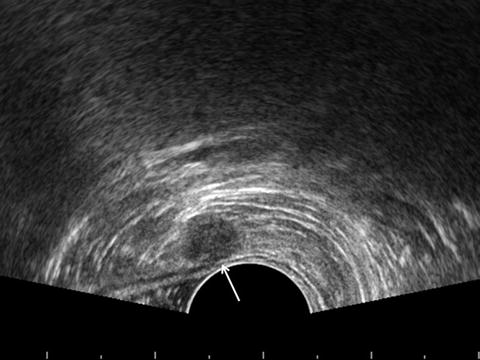

Fig. 11
A 78-year-old man status post high-dose rate radiation therapy for Gleason grade 4 + 4, PSA 22.3 ng/ml cancer 11 years ago presented with rising PSA to 1.398 ng/ml. CT scan revealed a 9 mm perirectal lymph node (arrow)
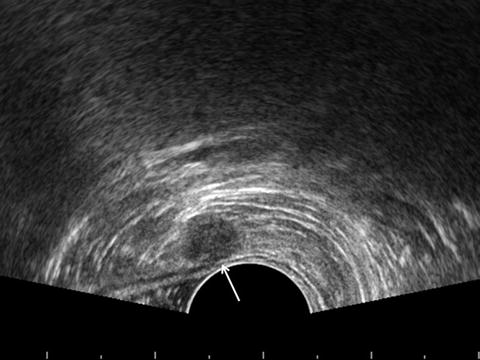
Fig. 12
Same patient. The perirectal lymph node was visualized by TRUS (arrow). Biopsy of the prostate and seminal vesicles did not show any evidence of local recurrence. However, biopsy of the lymph node revealed metastatic adenocarcinoma Gleason grade 4 + 4
Mass Anterior to the Prostate
During TRUS, abnormal tissue anterior to the prostate may be encountered. Biopsy of those lesions frequently requires a needle completely traversing through the prostate tissue to get to the anterior aspect of the prostate gland (Fig. 13).
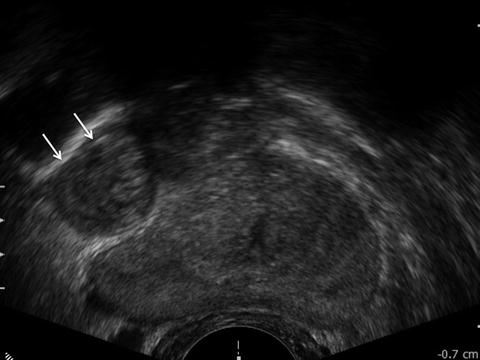
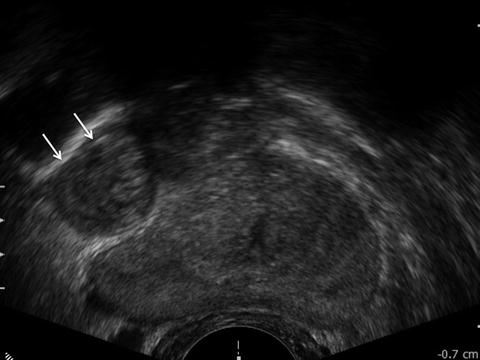
Fig. 13
A 62-year-old man with elevated PSA of 8.7 was found to have a round mass anterior to the right lobe of the prostate (arrows). Biopsy of the mass showed degenerated prostatic stroma only
Prostate cancer may recur in the rectal wall due to cancer cell seeding by previous biopsy (Fig. 14). Malignancy unrelated to the prostate gland can be also encountered in the rectal wall (Fig. 15). Needle biopsy of such lesions may be necessary. Of course, biopsy of the rectal wall requires the needle tip to be advanced shallowly just before the lesion prior to triggering the biopsy gun.
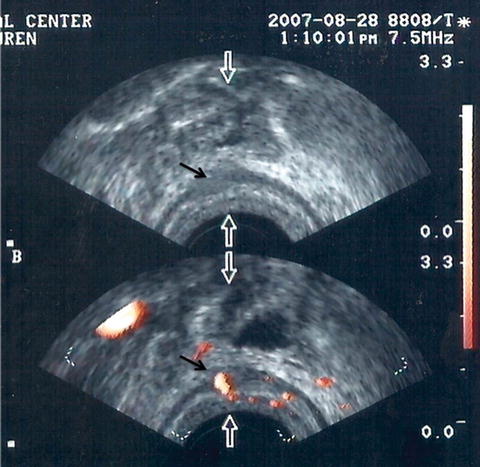
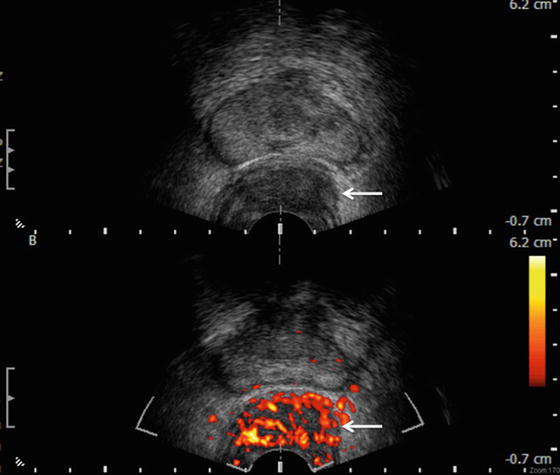
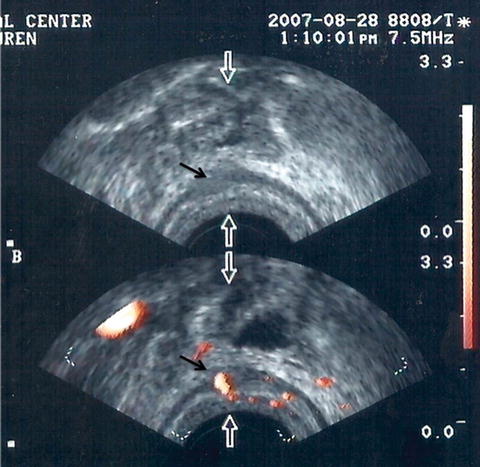
Fig. 14
A 65-year-old man status post radical prostatectomy was found to have a palpable nodule in the prostatic fossa with elevating PSA. TRUS showed a mass in the rectal wall (black arrows). Biopsy of the mass revealed Gleason grade 4 + 4 adenocarcinoma of the prostate
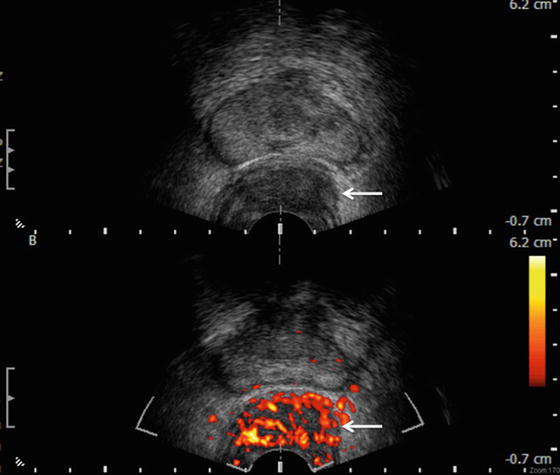
Fig. 15
A 45-year-old HIV positive man was found to have a rectal mass. Biopsy of the mass under proctoscope revealed only normal rectal mucosa. TRUS showed a hypervascular submucosal mass in the rectal wall. Biopsy revealed low-grade squamous cell carcinoma
Biopsy of Local Recurrence After Radical Prostatectomy
Biochemical failure with detectable PSA after radical prostatectomy can be seen in 30–40 % of cases in follow-up. Patients with a slow PSA rise and evidence of a positive surgical margin at the time of radical prostatectomy are more likely to have local recurrence. Biopsy in this setting is not generally considered mandatory prior to radiation therapy. However, confirmation of pathology and fiduciary marker placement may help to improve outcome.
Anatomy of Anastomotic Site After Radical Prostatectomy
Recognition of TRUS-based anatomy of the anastomotic site is important in order to accurately take a biopsy. On a sagittal view in the midline the anastomotic site is clearly identifiable as the area where the low echogenicity of the membranous urethra suddenly changes to a more echogenic tubularized segment of the bladder neck (Fig. 16) [14]. Local recurrence is commonly located proximal to this area and on the side or posterior aspect of the tabularized segment of bladder neck (Fig. 17) [15]. Identifying the membranous urethra, as described in the normal transrectal prostate biopsy section, also helps orient the true midline of the patient.
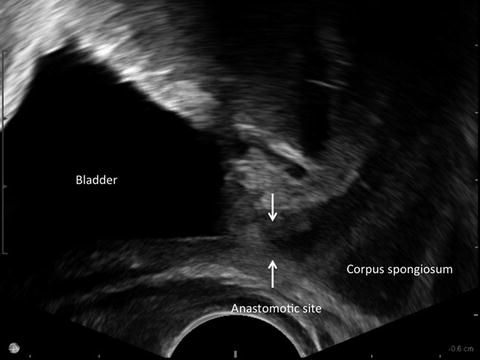
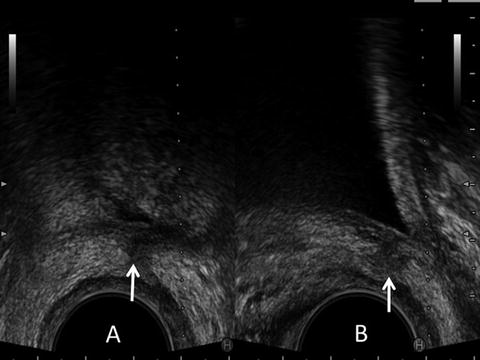
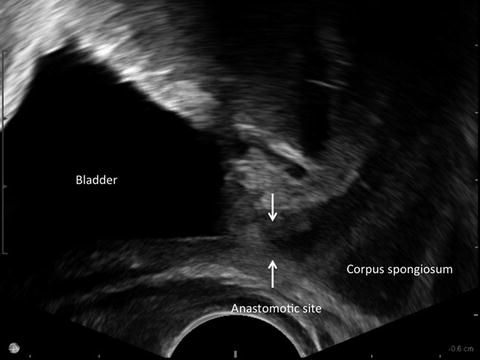
Fig. 16
Typical sagittal TRUS image of post radical prostatectomy patient. Anastomotic site is identifiable by the area where echogenicity changes from echogenic bladder neck to hypoechoic membranous urethra (arrows)
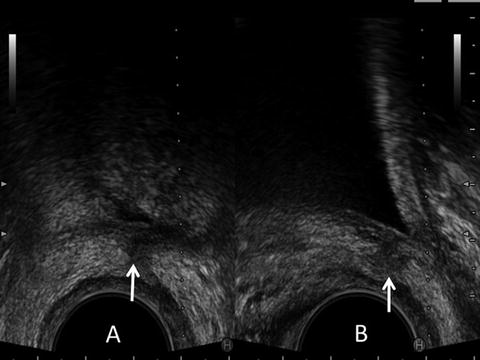
Fig. 17
A 61-year-old man status post radical prostatectomy with gradual rise of PSA to 0.52 ng/ml. TRUS showed a hypoechoic tissue suspicious for local recurrence at the posterior aspect of the bladder neck over midline (arrows). (a) Transverse view, (b) sagittal view
Biopsy Technique
On the TRUS image, the bladder neck tissue can be seen as a tubularized segment. A local recurrence is frequently seen on the side or posterior aspect of this tubularized segment of the bladder neck as hypoechoic tissue. When the probe is slightly tilted to obtain an off midline image, hypoechoic tissue can be seen isolated from the bladder neck. This finding is very suspicious for local recurrence. Some lesions can be seen as an asymmetrical thickening of the tissue around the anastomotic site or behind the bladder on a transverse image. Occasionally, benign prostatic tissue that persists after radical prostatectomy can be seen as isoechoic tissue (Fig. 18). Local anesthesia is usually not necessary, since only a few samples are taken. However, similar to the apex biopsy, a needle can stimulate the proctocanal when this area is biopsied. The needle tip can easily penetrate through the bladder wall in this population. Observation of the bladder wall by TRUS as described before to confirm the degree of hematuria after biopsy is always necessary for this procedure, since bladder wall bleeding is quite common.
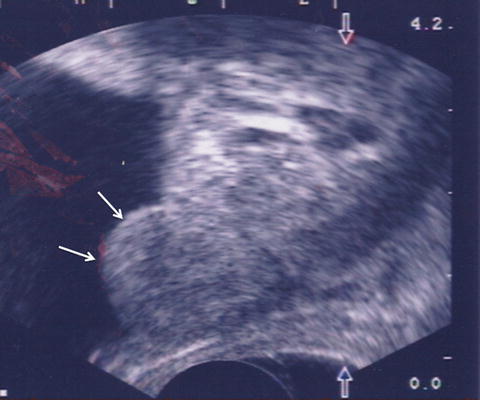
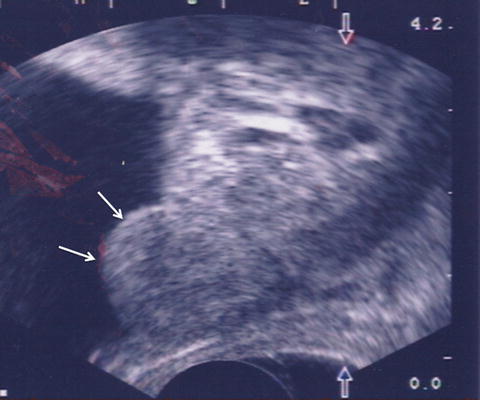
Fig. 18
A 62-year-old man status post radical prostatectomy with detectable PSA of 0.43 ng/ml. TRUS revealed tissue resembling residual median lobe of the prostate (arrows). Biopsy of the tissue showed benign prostatic tissue
Biopsy of Prostate for Patient Without Anus or With Severe Anal Stricture
Patients that have undergone abdominoperineal resection of the rectum (APR) have no access to the rectum. Digital rectal examination or transrectal ultrasonography cannot be performed, and often prostate cancer diagnosis can be delayed. PSA is the only tool for screening prostate cancer in this population. Transperineal ultrasound-guided prostate biopsy can be performed [16]. Generally, the procedure is performed with the patient in the left lateral decubitus position as in a regular TRUS procedure. In order to visualize the urethra and bladder clearly, placement of Foley catheter in advance is recommended. Intra-prostatic information is very difficult to obtain by transperineal ultrasound. The more important task of ultrasound in this procedure is localization and delineation of the prostate itself. For this purpose, an end-fire probe with a lower frequency setting, 5–6 MHz, is ideal for scanning, since better penetration and visualization of deeper tissue is required. After preparation of the skin with antiseptic solution, a probe is applied on the previous anus location that is frequently identifiable by a small skin dimple. Once the Foley catheter is identified, follow the catheter to identify the balloon. At this point, the prostate is seen next to the balloon. The prostate can be visualized either in a longitudinal or cross-sectional image (Figs. 19 and 20). Local anesthesia is given to the perineal skin, pelvic floor, and all the way to the prostate gland by ultrasound guidance. Care must be paid not to inject air during anesthesia, since this will significantly disturb the visualization of the prostate gland. Prostate biopsy can be done either with a sagittal or coronal view. The needle is advanced until it reaches the prostate capsule, as confirmed by ultrasound and a tactile sensation. After the needle tip reaches the prostatic capsule, the biopsy specimen is taken. Extended sextant biopsy of 12 samples can be obtained. Seminal vesicles are frequently biopsied as a staging purpose whenever it is visible, since the local staging cannot be performed by either digital rectal examination or transrectal ultrasonography. For a patient with severe anal stricture due to previous surgery or sphincter spasm, the TRUS probe can be applied over the anus and local anesthesia applied to the perianal tissue anterior to the anus. The prostate gland can be visible in this position and biopsy can be done as in the post-APR patient (Fig. 21).
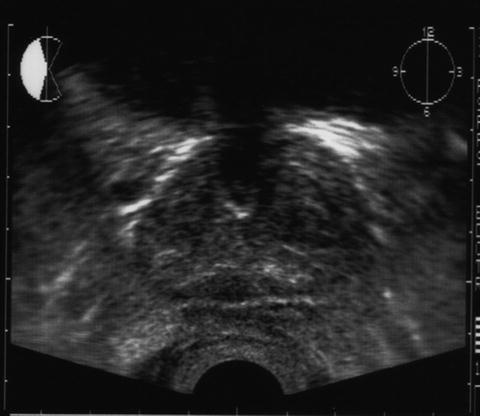

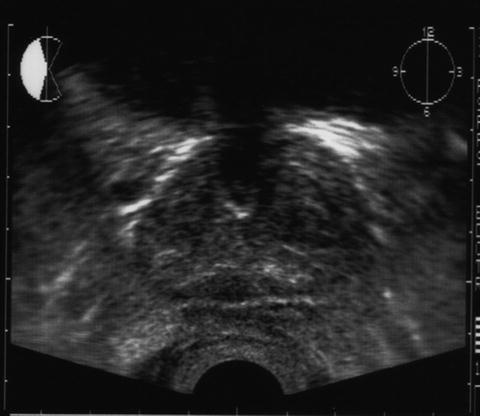
Fig. 19
A 64-year-old man status post abdominoperineal resection of rectum from ulcerative colitis was found to have an elevated PSA of 5.6 ng/ml. Transperineal ultrasound revealed clear image of the prostate gland in transverse view

Fig. 20




Same patient in sagittal view in midline. A Foley catheter and a balloon were identifiable
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree