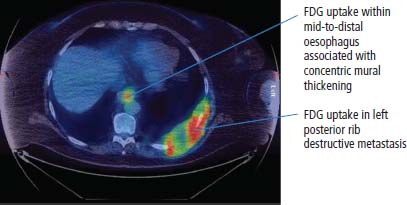
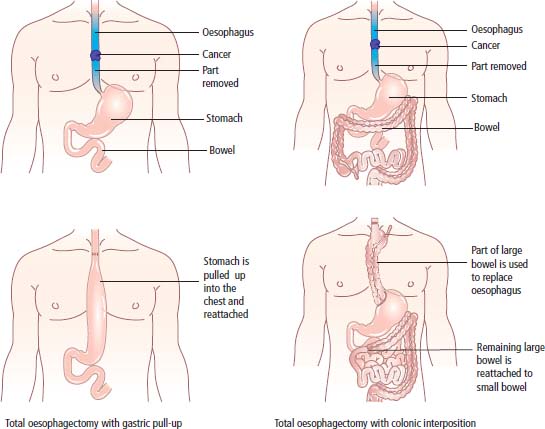
7 The British playwright Harold Pinter was diagnosed with cancer of the oesophagus and wrote the eloquent poem ‘Cancer Cells’, whilst undergoing chemoradiotherapy, which illustrates his understanding of the molecular basis of cancer. The poem can be read at: http://www.theguardian.com/books/2002/mar/14/poetry.haroldpinter. Cancer of the oesophagus is a relatively uncommon cancer in the United Kingdom with 8332 diagnoses and 7603 deaths in 2011, but the incidence is rising, at least in men (Table 7.1) and causes awful suffering. Oesophageal cancer is rare under the age of 45 and the incidence rises steeply with age. It is two to three times more frequent in men. Worldwide, oesophageal cancer is the sixth most common cause of death from cancer and it is 20–30 times more common in China than in the United States. Two-thirds of cases of oesophageal cancer are adenocarcinomas, typically of the lowest third of the oesophagus, whilst one-third of cases are squamous cell cancers occurring usually in the upper two-thirds of the oesophagus. The incidence of adenocarcinoma relative to squamous cancer is rising. Tobacco is a major risk factor for both histological types of oesophageal cancer, but the two types otherwise vary not only in their histology and anatomical distribution but also in their risk factors. Chronic irritation appears to be a major precipitant of squamous cell cancer and may be caused by alcohol, caustic injury, radiotherapy or untreated achalasia. The Plummer–Vinson syndrome (also known as Patterson–Kelly–Brown syndrome) of chronic iron deficiency anaemia, dysphagia and oesophageal web is associated with squamous cell cancer of the oesophagus, particularly in impoverished populations. Tylosis is an autosomal dominant abnormality, characterized by hyperkeratosis (skin thickening) of the palms and soles. It carries a 95% risk of squamous cell cancer of the oesophagus by the age of 70. Chewing betel quid or paan, a mixture of betel leaf, areca nut and slaked lime causes mild euphoria and stains your teeth red. It also increases the risk of both cancers of the oral cavity and squamous cell cancer of the oesophagus. Table 7.1 UK registrations for oesophageal cancer 2010 In contrast, the major precipitant of oesophageal adenocarcinoma appears to be gastro-oesophageal reflux disease (GORD). Related markers of reflux, such as hiatus hernia, obesity, frequent antacid and histamine H2 blockers, are also associated with an increased risk. Barrett’s oesophagus (named after Norman Barrett, a thoracic surgeon at St Thomas’ Hospital, London) is an acquired premalignant condition that develops in 5–8% of adults with reflux leading to metaplasia of the normal squamous epithelium of the lower oesophagus to columnar epithelium, which may become dysplastic, see Box 1.2. Other causes of distal oesophageal irritation such as hiatus hernia, achalasia and scleroderma can also lead to Barrett’s oesophagus and overall it affects 0.5–2% of the adult population. The annual rate of transformation from Barrett’s oesophagus to oesophageal adenocarcinoma is 0.12%, which is 11 times greater than the normal risk. The risk is highest for obese white men over 45 years old who smoke. Over the last three decades, there has been a radical shift in the histology of oesophageal cancer in the industrialized world, with a marked decline in squamous cell cancers and a rise in adenocarcinomas. This may reflect alterations in the number of smokers and in the obesity and nutrition of patients. Half of all cases of oesophageal cancer could be prevented by giving up smoking, drinking less alcohol and improving diet, substituting fresh fruit and vegetables for poorly preserved, high salt foods contaminated with nitrosamine carcinogens or microbial toxins. Endoscopic surveillance is recommended every 2–5 years for patients with Barrett’s oesophagus, but the evidence that screening is effective is absent. Low-grade dysplasia requires aggressive anti-reflux management, whilst multifocal or high-grade dysplasia should be treated by surgical resection. Patients present with dysphagia or odynophagia (pain on swallowing), weight loss and, less frequently, with haematemesis. At the time of diagnosis, more than half of the patients will have locally advanced, unresectable disease or metastases present. Left supraclavicular lymphadenopathy (Virchow’s node), hepatomegaly and pleural effusion are common features of metastatic dissemination. Rudolf Virchow is said to have described the association after diagnosing it in himself. He also challenged Bismarck to a duel with sausages but that is another story. The diagnosis is usually confirmed by upper gastrointestinal endoscopy (Figure 7.1) and barium studies (Figure 7.2). Figure 7.1 Endoscopic view of cancer of the mid-oesophagus. Figure 7.2 Oesophageal cancer. Gastrografin swallow image showing a long tight stricture of the distal third of the oesophagus with shouldering that encroaches on the gastro-oesophageal junction. This malignant stricture was due to adenocarcinoma of the oesophagus. Although CT or PET-CT staging is most helpful in defining operability and presence of nodal involvement (Figure 7.3), additional information can be obtained from using endoscopic ultrasound which is able to evaluate the depth of invasion. This allows the surgeon to have a better view as to the extent of the resection that is required. Figure 7.3 PET-CT scan of metastatic squamous cell cancer of the oesophagus. Only 40% of patients will have localized disease at presentation and are candidates for oesophagectomy with or without neoadjuvant or postoperative adjuvant chemoradiation. Oesophagectomy shortens the oesophagus so a section of the stomach is pulled up into the chest cavity (Figure 7.4). Adjuvant chemoradiotherapy, either prior to surgery (neoadjuvant), or following resection, appears to improve survival but the gain is likely to be modest. Surgery has a 5–10% mortality rate and may be complicated early by anastomotic leaks, and later by strictures, reflux and motility disorders. At diagnosis, 25% of patients will have local extension and are treated with palliative radiotherapy, which may cause oesophageal perforation and haemorrhage, pneumonitis and pulmonary fibrosis, as well as transverse myelitis (inflammation of the spinal cord leading to sensory, motor and sphincter deficits). The remaining 35% of patients will have metastases at presentation and are usually treated symptomatically or with palliative chemotherapy if they are fit. Although cancer of the oesophagus is sensitive to chemotherapy, the duration of response is typically short and may be measured in weeks. Cisplatin-based combination regimens have higher response rates, but this may be offset by their greater toxicity. Symptomatic relief from dysphagia in patients unsuitable for surgery may be achieved by endoscopically placed oesophageal self-expandable metallic stents or plastic stents (see Figure 3.5). Figure 7.4 Types of total oesophagectomy. Reproduced with permission of CancerHelp UK. Table 7.2 Five-year survival rates of patients with oesophageal cancer, according to stage at presentation Tis, carcinoma in situ; T1, invasion of lamina propria; T2, invasion of muscularis propria; T3, invasion of adventitia; T4, invasion of adjacent structures. The 5-year survival rates of patients with oesophageal cancer according to stage at presentation are detailed in Table 7.2. Case Study: An actuary with a leak.
Oesophageal cancer
Epidemiology and pathogenesis
Percentage of all cancer registrations
Rank of registration
Lifetime risk of cancer
Change in ASR (2000–2010)
5-year overall survival
Female
Male
Female
Male
Female
Male
Female
Male
Female
Male
Oesophageal cancer
2
3
13th
8th
1 in 110
1 in 56
–9%
+7%
12%
13%
Prevention
Presentation


Staging and grading
Treatment
T stage
N stage
M stage
(local
(nodal
(metastatic
5-year
Stage
tumour)
status)
status)
survival
0
Tis
N0
M0
>95%
I
T1
N0
M0
50–80%
IIA
T2–3
N0
M0
30–40%
IIB
T1–2
N1
M0
10–30%
III
T3–4
N0–1
M0
10–15%
IV
Any T
Any N
M1
<2%
Prognosis
 ONLINE RESOURCE
ONLINE RESOURCE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


