There are many things that a doctor, on his first visit to a patient, ought to find out either from the patient or from those present. For so runs the oracle of our inspired teacher: “When you come to a patient’s house, you should ask him what sort of pains he has, what caused them, how many days he has been ill, whether the bowels are working and what sort of food he eats.” So says Hippocrates in his work AFFLICTIONS. I may venture to add one more question: what occupation does he follow?
—
Bernardino Ramazzini 1713 (1)
The men and women of the aerospace industry, both those on the ground and in the air are exposed to hazards of injury and illness beyond that that is unique to the flying environment. Occupational injuries and exposures are all too common in the workplace and aerospace presents numerous hazards. This chapter provides an opportunity for the student or casual reader to become familiar with the policies and procedures in the United States that have been developed to prevent or manage workplace morbidity and mortality.
Similar policies and procedures are at work to prevent or reduce the harm to the public that is present because of aviation activities. Such risks include transmission of disease by a large fast-flying vector—the aircraft or spacecraft. Arthropods, infectious carriers, and formite transmission have all been transported by aircraft. To some the aircraft becomes a potential hazard to the environment because of the jet or rocket exhaust. This chapter is presented in two major sections: occupational hazards and environmental concerns.
SECTION ONE: OCCUPATIONAL MEDICINE
The American Board of Preventive Medicine defines occupational medicine as that specialty which focuses on the health of workers, including the ability to perform work; the physical, chemical, biological, and social environments of the workplace; and the health outcomes of environmental exposures. Practitioners in this field address the promotion of health in the workplace and the prevention and management of occupational and environmental injury, illness, and disability (
2).
In 2005 Paul A. Schulte, PhD a researcher at the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC), published an article regarding the national burden of occupational injury and disease on the nation. His research demonstrated that the burden of occupational injury and illness is substantial among America’s workforce. In 2002, the Bureau of Labor Statistics (BLS) reported more than
5,500 fatal work injuries, 4.4 million nonfatal injuries, and 294,500 illnesses. In the same year, NIOSH estimated that 3.6 million occupational injuries and illnesses were treated annually in U.S. hospital emergency rooms. His research further addressed a $72.9 billion expense to employers for worker’s compensation premiums with a total direct and indirect cost estimated to be in the range of $128 to $155 billion (
3).
Each year there is a survey of occupational injury and illness across the United States. This is a federal/state program in which the employer reports are collected from private industry. The survey measures nonfatal injuries and illness and excludes self-employed. farms with fewer than 11 employees, private households, federal government agencies, and the national data system employees in state and local government agencies. The survey provides estimates of the incident rates of the injuries and illnesses based on logs kept by the industry employers during the year. The most current data available (2005) is summarized by industrial sector beginning with the highest incident rate of illness and injury. These data are summarized in
Table 21-1. The overall national incident rate was 4.6 cases per 100 equivalent full time workers during 2005.
The census of fatal occupational injuries is also a part of the BLS Occupational Safety and Health statistics program compiled for the United States each calendar year. The data set contains information about each workplace, worker characteristics, equipment being used, and the circumstances of the fatal event.
In his preface to the
Occupational Medicine State of the Art Review titled The Aviation Industry, Dr. Kendall Green commented that occupational aviation medicine is an amalgam of two specialties of preventive medicine: occupational medicine and aviation medicine (
4). He further noted that as a part of preventive medicine, occupational and aviation medicine include the public health and epidemiologic perspectives in addition to the perspectives of “what’s best for my patient” commonly seen in clinical medicine.
Aerospace medicine and occupational medicine are part of international coalitions of specialty medical practice. In much of the world, the term
occupational medicine is better translated in the broader term of occupational health. The World Health Organization (
WHO) in 1950 undertook to define “occupational health” as follows:
Occupational health should aim at the promotion and maintenance of the highest degree of physical, mental, and social well-being of workers in all occupations; the prevention among workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological equipment; and to summarize, the adaptation of work to man and of each man to his job.
In more modern times, the gender bias has been removed and it is well recognized that we have people of both genders actively participating in the workplace.
It was within the context of this definition that the specialty of occupational medicine became formalized. In 1955, a certification program in occupational medicine was established by the American Board of Preventive Medicine. As of 2007, a total of 3,609 physicians have been certified in occupational medicine as compared to 1,423 in aerospace medicine (
5).
A key element of both occupational and aerospace medicine is their focus on prevention. Many of the tools used by the profession are those that address illness and injury prevention as well as the clinical topics involved with treatment and management of afflictions, impairment, and disability. Service is provided to a workforce with a demographic characteristic that remains predominantly male in the age-group between 18 and 65. Because of the requirements of employment, most workers are in better health than the general population and enjoy a middle class living standard. In epidemiologic studies that address this population, a term identified as the healthy worker effect is important in studying cohorts that are compared with worker populations. Workers in general are in better health with less morbidity and lower mortality when compared to the general population even when gender and age adjusted because they are an employed cohort.
The workplace in the aerospace industry incorporates many of the materials, processes, and operations common to manufacturing in general: airplane repair and maintenance that includes drilling, riveting, screwing, fastening, welding, painting, aluminum layout, template work, subassembly, fuselage fabrication, manipulating large units, replacing of motors, engines, propellers, turbines, wing sections, electronics and avionic equipment, and the inspection of planes, equipment, and machine tool repair. Further, it is often the aviation industry that introduces new machine processes such as the fabrication of titanium structures and
the buildup of metal and carbon fiber composites. Common work-related medical problems occurring in the aerospace industry are enumerated in
Table 21-2 (
6).
Specialists in aerospace medicine must develop and maintain sufficient orientation and knowledge in the fields of occupational and environmental medicine (OEM) to assist management in obtaining and using the consultation necessary to prevent and solve problems that involve potential toxic hazards arising out of planned operations, products, and waste. In this way, aerospace medicine is better able to encompass the total program of preventive medicine in support of this national industry that is so critical to the economy and national defense.
HISTORY
The relationships of types of work to illness were first addressed by Hippocrates. Centuries later, Ramazzini in his treatise
Disease of Workers described a constellation of afflictions that befall workers in more than 50 occupational settings (
1). As the book was published in the 1700s, it would be surprising if it mentioned anything regarding the aviation industry. Early in the last century, Alice Hamilton, a professor at Harvard’s College of Public Health began to visit American industries in the eastern United States documenting her observations and making recommendations to improve the lot of the worker. Her autobiography
Exploring the Dangerous Trades details some of her experiences with American industry (
7).
More recently, Dhenin, a leader in aviation medicine in the United Kingdom observed that aviation medicine is a branch of occupational medicine developed from the need to adapt humans to the hostile environment of the air (
8). Although within the United States this observation may be considered controversial by some, it does have its advocates. This recognizes the close relationship between aerospace medicine and occupational medicine, particularly when considering commercial airline and military operations. In 2005 among the major airlines in the United States, only 20% of employees were flight deck personnel and flight attendants, whereas the remaining 80% were classified as ground personnel. Although flight personnel are potentially exposed to many of the hazards unique to flight as described in detail in several chapters of this text, they are also susceptible to occupational illnesses and injuries similar to their ground personnel cohorts.
The U.S. Department of Labor annually publishes labor statistics that include the aviation industry.
Table 21-3 lists the type and number of workers in various categories divided roughly into airline operations and aviation manufacturing and maintenance. These figures provide a glimpse of the complexity of the workforce and its distribution in specialties across the industry (
9).
To provide a different perspective, the classification of the workforce for a large U.S. international airline hiring approximately 100,000 workers is given in
Table 21-4 (
10). In recent years, there has been a considerable downsizing of many of the U.S commercial airlines resulting from cost pressure. The head count has become very sensitive to the
bottom line. For example, in 2003 Delta Air Line’s head count was 70,600 employees with a fleet of 833 planes and a cost of 9.36 cents/mi. In 2006, the employee numbers had dropped to 51,000 with a fleet of 625 planes and a cost per seat mile of 6.91 cents (
11).
ESTABLISHING AN OCCUPATIONAL AND ENVIRONMENTAL MEDICAL PROGRAM
First and foremost, occupational medicine is a specialty of medicine that is a discipline within preventive medicine. The major goal is to prevent injury and disease and should this not be entirely effective, to prevent death and disability, returning the employee to work as soon as is feasible within the bounds of good health and work capability. This service is far more complex than simply suturing a laceration or performing a preplacement physical examination. The complexities of this practice are complicated by strong regulatory and legislative influences potentially involved with the practice. Physicians have responsibilities that extend beyond the usual clinical situation. A comprehensive program will provide many of the services listed in
Table 21-5 (
12).
There are many settings and situations in which these services are provided. These range from the office of a family physician to acute care clinics, including multispecialty group practices, hospital-based services, occupational medicine clinics, corporate medical services, and consulting practitioners. The full list of services cited in
Table 21-5 will typically be available only in the larger, more comprehensive programs.
The consultant provides a focused service to the aviation industry. Frequently this involves a particular field of expertise, such as toxicology, ergonomics, wellness, or managerial skills, which is available to the industry on a time-limited, but intense, basis. The services of the consultant are usually focused around problem-solving issues and recommendations may include both short-term corrections and long-term solutions.
The types of aviation and space industrial sites where workers are employed are listed in
Table 21-6.
SCOPE OF PRACTICE
In 2004, the American College of Occupational and Environmental Medicine’s (ACOEM) executive board approved a document entitled “Scope of Occupational and Environment Health Programs and Practice.” This document provides an excellent summation of the composition and complexities of an occupational medicine practice whether housed in industry, medical centers, and clinic or private offices. It was noted that the role of the occupational physician had expanded in recent years to enhance the productivity of the worker with absent management and increased emphasis on the wellness of the worker. Recently it has been recognized by organizations and regulatory agencies that such trained physicians have expertise in the analysis and development of programs and policies that protect the worker. The doctor may design programs and management health services directed toward defined populations as well as engaging in clinical care of the individual (
13). With expansion of the global economy, the American workforce becomes more involved as an integrated member of a global workforce. This requires the physician to understand the needs of the international worker in the local community and ensure that occupational safety and health care in those communities are encouraged toward the best practices. The complexity of the occupational medicine programs in aviation and space requires intellectual and practical skills beyond the clinical arena. Broad-based practices in this industry require professional teamwork and it becomes necessary to enlist and collaborate with the skills and talents of a large number of colleagues in such areas as industrial hygiene, toxicology, occupational health nursing, safety engineering, industrial relations, health physics, engineering, personnel management, biomechanics, law, public policy, and of course health education. Occupational health programs and their practitioners are advancing the field of health and productivity. To accomplish this it is necessary to incorporate a wide spectrum of activities to include occupational health, safety, loss and risk management, absence and disability management, health promotion, disease management, injury prevention, hazard control, and management of health care benefits. A number of these programs are specifically addressed in the following paragraphs.
THE WORK PLACE ENVIRONMENT
Centuries ago, Ramazzini reminded physicians that in order to know the employment circumstances of a worker, one must go to the work site. In aviation manufacturing or flight control operations, the complexities of the work environment can only be understood through direct observation. Recognition, evaluation, and control of hazards posed by chemical, biological, and physical agents, as well as ergonomic stresses and safety risks, require occasional on-site visits. Areas for consideration when providing these services will be discussed further.
Process Descriptions
These are necessary for routine repetitive functions and for special projects that include identification of raw materials, description of processing equipment and conditions (such as temperature and pressure), description of work activities involved, and a description of feedstock, product and intermediaries, by-products, and waste.
Hazard Communications
A chemical inventory is required by the Occupational Safety and Health Administration (
OSHA) as detailed in the Hazard Communications Standard. The inventory must be comprehensive and include components of mixtures and identification of chemical constituents of trade name products, and it must remain current. For each chemical in use, information must include chemical and physical properties, as well as toxicity features of animal and human exposure at levels thought to be safe for occasional and daily exposure. Material safety data sheets (MSDS) are required for each chemical that is used at the industrial site as directed by the Hazard Communications (right to know) regulation. In addition to toxicologic information, there is additional information and other precautions to be observed in handling, storing, and emergency control measures in cases of spills. Names and phone numbers of individuals to contact for additional information or assistance are listed. From a medical information point of view, the MSDS provides instructions to emergency responders on how to initially manage a worker who has been exposed at a high enough level to cause adverse symptoms.
Listing of Employees
A list of each employee with consecutive job titles and work assignments as well as some method for identifying potential chemical exposures should be available. Personnel or environmental monitoring of levels of chemicals or physical agents must be recorded and indicate sampling strategies, procedures, and dates. Ideally, there should be a cross-indexing of workers, job titles, work areas, and projects to allow for comprehensive review of potential past exposures. This is frequently needed for comprehensive medical surveillance of employee exposure. It is not uncommon to find similar listing but only for the current job held by the employee. Because of the issue of long intervals between exposure and appearance of adverse health
effects such as cancer the entire work history combined with exposure history is important.
Reports of Occupational Injury and Illness
Such reports are frequently listed in the
OSHA 300 Log, a separate listing of injuries and illnesses that occur in the workplace, and identify the injured worker, the circumstances of the injury, and the degree of medical intervention. This record is helpful in identifying workplace problems so that solutions can be identified and implemented. The log is used to notify federal agencies of the occurrence of accidents and injuries. Such data may be used to establish periodic inspections of the workplace by such state or federal entities.
Control Measures
For controls to be effective requires interdisciplinary cooperation between medicine, engineering, industrial hygiene, and management. The implementation of control technologies is most effective and economical when they become a part of the original design and installation. Removing the hazard through control procedures is by far the best preventive medicine action. When solvents or other feedstocks are considered, a product toxicologic review of the material before its procurement may lead to a far safer item than trying to institute control measures after the fact.
EMPLOYEE TREATMENT, EVALUATION, AND EDUCATION
Employee treatment, evaluation, and education are occupational medicine services that at one time were commonly provided by the employer on site, but have become a part of the “sizing” of American industry and have frequently been outsourced. These types of services, whether in-house or not, have both medical and nonmedical components. Providing treatment for occupational injury or illness is the obligation of the employer. Such treatment should be handled either by on-site medical personnel or be referred. Complicating health care management is the insurance system that exists in all states and federal agencies known as Worker Compensation to be discussed further.
Work Placement
Work placement may depend on the nature and extent of limitations of function caused by medical conditions. Evaluation of such limitations when preplacement medical examinations are performed may influence the proper placement of potential employees. The occupational medicine physician needs to become familiar with the Americans with Disability Act (ADA). This federal program was put in place to ensure that an employee is not discriminated against unfairly when seeking a job. Since its implementation in 1992, it has been more precisely defined through the courts.
Medical Surveillance
The program of medical surveillance provides information on “target organs” that may be adversely affected by a particular hazard or multitude of unknown agents. Surveillance programs help to assess the adequacy of protective measures. Medical surveillance includes the development of a baseline health inventory followed by periodic reevaluation. Medical surveillance is not intended to be the sole method for control of exposures to such chemicals. Its intention is to be used as a check on control policies and procedures within the workplace.
Epidemiological Surveillance
This type of surveillance can help detect possible work-related adverse health effects. Prudence dictates epidemiologic evaluation of health indicators for those worker populations with potential exposures to possible health hazards.
Education
Employee and supervisor education that addresses workplace health factors is vital in preventing illness and injury. There are also significant ethical, legal, regulatory, and employee relations reasons for programs to educate the workforce.
Training
Employee and supervisor training in proper work practices and in the use of personal protective equipment may be required or appropriate. Special training is frequently necessary for employees to meet the emergency, first aid, and cardiopulmonary resuscitation needs of the facility. In certain situations, the
OSHA Hazard Communication Standard requires employee training and education.
Employee Assistance Programs
The Employee Assistance Programs (EAP) provides vitally important services for troubled employees and their families. The comprehensive approach, which may include counseling on marital, financial, and interpersonal issues, is generally more effective than simply limiting such intervention to the traditional alcohol and drug abuse problem. Opportunities for self-referral and confidentiality are important program considerations.
Health Promotion
Wellness programs dealing with nonoccupational health situations such as smoking cessation, nutrition, fitness, and other lifestyle issues are increasingly important, and their value to both the worker and industry are now well documented (
14,
15).
REGULATORY AND ADVISORY AGENCIES
As in many fields of endeavor in which humans engage in an industrial society there are regulations, rules, laws, and policies. In the field of OEM, there are a number of entities at both state and federal level that provide advice, recommendations, training, and research as well as serve as regulatory agencies with police power. An efficient and effective occupational health program must comply with regulations and seek out and use educational and advisory information. A number of these agencies, administrations, and institutes are described in subsequent text.
Occupational Safety and Health Administration
The passage of the Occupational Safety and Health Act in 1971 created the
OSHA and the NIOSH. The primary regulatory agency for occupational safety and health is
OSHA. Its standards have the weight of law throughout the United States and its compliance officers can inspect the workplace at anytime to determine the status of health and safety. If a serious safety violation is found that could result in immediate harm to workers, the establishment can be closed. The agency can use the power of a court order citation or fine to enforce compliance. States may elect to have their own programs and half have done so. The state program must, as a minimum, meet all the regulations and other requirements established by federal
OSHA. This is an agency of the Department of Labor and as such develops regulations, which are announced through the Federal Register.
One of the early standards established permissible exposure limits (PELs) for hundreds of chemicals. To accelerate the standards-setting process
OSHA was permitted to adopt as a consensus standard the threshold limit values (TLVs) established by the American Conference of Governmental Industrial Hygienists (
ACGIH). In an agreement signed on August 7, 2000
OSHA and the Federal Aviation Administration (
FAA) pledged to work together to improve the working conditions of flight attendants while aircraft are in operation. As a first step the two agencies formed teams to review
OSHA standards on record keeping, blood-borne pathogens, noise, sanitation, hazard communication, and access to employee exposure and medical records. Previously
OSHA enforced standards for maintenance and ground support personnel in the airline industry while the
FAA provided assessment of hazards related to flight deck personnel (
16).
Currently both the
OSHA PELs and the
ACGIH TLVs are operative. Each year the
ACGIH publishes TLVs for chemical substances and physical agents as well as biological exposure indices. This small handbook, which readily fits into a briefcase, makes readily accessible many of the hazardous exposure levels that should be avoided in the workplace. The nature of the standards-setting process makes the modification of current or the introduction of new PELs extremely cumbersome. The altering or adding new TLVs, although discussed and at times controversial, is far more expeditious and therefore may represent the more current scientific thought. To add further complication to these values is the NIOSH recommended exposure values (REVs). These levels are believed to be low enough that they would constitute levels with no adverse health effects for any worker.
National Institute for Occupational Safety and Health
NIOSH is an arm of the Department of Health and Human Services and is housed at the CDC. Like
OSHA, NIOSH has the authority to conduct inspections and to question employees and employers and even to include the use of warrants to acquire information on workplace conditions. However, it is not a regulatory agency and cannot levy penalties and this fact enhances its ability to serve as a consultant. Further, it serves the occupational and environmental health community as an educational resource providing not only material but also financial support for educational programs such as residencies in occupational medicine. Funding support is also provided to research projects in the field of OEM.
Environmental Protection Agency
The Environmental Protection Agency (EPA) was created to enforce the Toxic Substance Control Act (TSCA) as well as other regulatory functions. It is responsible for regulating the quality of water and air and addresses numerous environmental problems such as hazardous waste sites. When it comes to the workplace, EPA must take a backseat to
OSHA until hazardous waste, air or water pollution, or other
hazardous substances leave the plant site. The EPA works with other agencies in serving as an educational and training source as well as collecting and disseminating information on hazardous materials. Like
OSHA, EPA is a regulatory agency and has all the powers necessary for enforcement.
Assisting EPA in the same way that NIOSH provides recommendations for regulatory activity to
OSHA is the Agency for Toxic Substances Control Registry (ATSDR). Two publications which are the responsibility of ATSDR that are of value to physicians are the “Toxic Profile” series on individual hazardous chemicals and the “Case Studies in Environmental Medicine” series using case studies as a method to educate physicians.
WORKPLACE HAZARDS
The aviation industry has the potential of exposing the workforce to numerous hazards that may result in adverse health effects. To assist in the systematic review of the major hazards of concern, they are categorized as chemical, physical, biological, and ergonomic.
Chemical Hazards
In many respects, to define a substance as a toxic chemical is redundant. Essentially all chemicals are toxic, given a specific route of exposure or an excessive dose. A gallon of water becomes toxic when inhaled; oxygen can induce convulsions when breathed under hyperbaric conditions; 500 g of table salt taken orally at one setting will have serious adverse effects on metabolism. The topic of toxicology is complex and still evolving.
Chemical hazards are harmful substances that may be encountered anywhere in the workplace and have been classified in various ways. Such a classification would include the physical characteristics such as dust, fumes, mist, vapors, gases, and liquids. Another classification can address the chemical class of the hazard and would include acids, bases, solvents, metals, petroleum products, and geologic derivatives such as silica, asbestos, coal, and petroleum. The toxic manifestation of the chemical is related to the steps it undergoes in its interaction with the body. These include uptake, distribution, metabolism, storage, and excretion. To fully understand the toxic manifestations of the chemical, one is required to study these steps in order to understand the adverse effects produced by these interactions. Further information is available in
Chapter 9.
Threshold Limit Values
The intent of TLVs set by consensus within the ACGIHs
TLV committee is to provide reliable benchmarks to aid plant engineers, both in designing new facilities and in renovating old ones, so that the possibility of toxicity occurring in the workforce is minimized (
17). In this way, other protective measures such as personal protection, limiting exposure time, and special-purpose occupational medical examinations and tests could either be minimized or better still, documented as being unnecessary. The basic premise involved in industrial hygiene controls below a permissible (safe) exposure level is that repeated exposures over an 8-hour day, 5 days a week for a working lifetime of approximately 40 years could be allowed for most unprotected employees without harm. Although a few susceptible individuals in the workforce might develop evidence of harm, these persons would be detected by close occupational medical surveillance and removed or protected from further exposure before sustaining irreversible impairment or disability. The individuals who are sensitive or allergic to the chemical in question fall outside the proposed permissible limit, as there may be no safe limit.
Unfortunately, the facts that would help place matters of environmental and occupational health into proper perspective are not being communicated adequately to many of our citizens. As a result, a climate exists now in which the adverse effects on productivity and the economy are disregarded while sensationalistic, science fiction-type coverage in the media of environmentally induced illness claims are encouraged and even rewarded. The concept of absolute assurance appears to be the rule that it is reasonable to expect absolutely no risk to the individual, the community, or to the environment from activities of commerce. This tendency toward zero-exposure levels for many chemicals is cost prohibitive and may be without scientific merit. The attitude of some that industries must prove the nonevent, that is that a chemical is absolutely safe, violates the established and well-recognized limitations of epidemiology. There needs to be greater assurance that appropriate instruction in environmental and occupational health occurs at all levels within the biomedical community. For more information on toxic chemicals and toxicology generally, the reader is referred to
Chapter 9.
Biological Monitoring
Where environmental surveys cannot document adequacy of hazard control below a limiting federal standard (usually half the PEL), special purpose occupational medical examinations and biological monitoring may be required, even if proper protection is worn. Biological monitoring, for example, is required when there is asbestos or benzene exposure beyond the regulated levels. Conversely, where environmental data confirm the adequacy of hazard containment, only a preplacement baseline value may need to be established. To accomplish biological monitoring on a routine basis in the absence of potential hazardous exposures is unjustified due to the administrative burden, the cost of the tests, and the deviation of the worker away from his or her task.
Physical Hazards
Physical hazards are defined by Wald as hazards that result from energy and matter, and the relationship between the two (
18). Operationally, these hazards as they exist in the workplace can be organized into worker-material interfaces, the physical environment, and energy and electromagnetic radiation. Each of these is present in the aviation industry. Physical agents are formless and essentially weightless, but
may produce hazards to exposed workers by the transfer of energy of various types, resulting in rather specific bioeffects when permissible occupational standards are exceeded. Among the most important potentially harmful physical agents where there is a transfer of energy are (a) oscillatory motions, including noise and vibration; (b) extreme occupational temperature variations in the ambient environment; and (c) ionizing and nonionizing electromagnetic radiation.
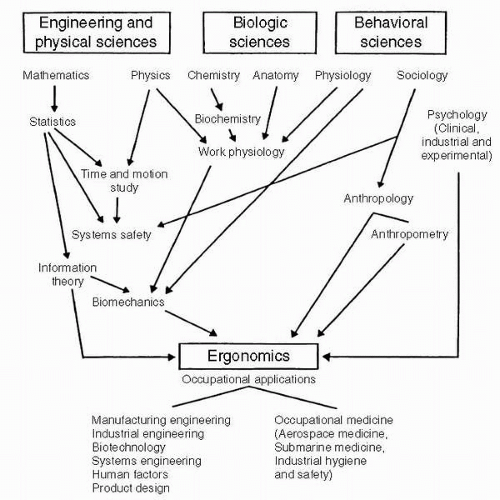
Figure 21-1 introduces other forms of physical hazards on the job that are typically defined as ergonomic or biomechanical but also have important consequences to worker health, safety, and productivity (
19). Many of these hazards are discussed in detail in other chapters within this text (see
Chapters 4,
5, and
7).
Electromagnetic Radiation Hazards
The electromagnetic radiation hazards (EMRs) spectrum encompasses an unbroken series of ethereal waves, moving with the velocity of light that vary widely in wavelength from cosmic rays as short as 4 × 10
−12 cm to hertzian waves (used in radio and power transmission), which extend several miles in length. For purposes of hazard evaluation and control, EMR falls into two distinct categories based on the ability to dissociate a substance in solution into its constituents or ions. These categories are universally identified as ionizing radiation (IR) and nonionizing radiation (
NIR). For further details on these hazards in the aerospace environment, the reader is referred to
Chapter 8.
Biological Hazards
Biological hazards may cause illness as a consequence of their infectious or toxic properties or because they may act as antigens and produce an adverse immune response. Such hazards are uncommon in airframe manufacturing, but of major concern in flight line operations. A noted exception in manufacturing is biological agent contamination of machine cutting fluids that are used to disperse heat and assist in removing metal cuttings.
In 1960, the first Report and Guide to Hygiene and Sanitation in Aviation was published. This addressed many of the flight line operational issues related to biological hazards. Disposal of passenger-generated waste presents a potential infection hazard to ground personnel. Animal transport by air introduces the possibility of spread of zoonoses to airline and ground personnel. The aircraft as a vector for disease transmission is addressed in Section Two of this chapter.
Ergonomic Hazards
Ergonomics has been defined by Chaffin as the science of fitting the job to the worker (
20). In both flight line operations and aircraft manufacturing, this interaction of workers with machines focuses on the one hand with compatibility of the worker’s capabilities and limitations, and the job requirements and machine interface on the other. Ergonomic design is well appreciated in the cockpit, but may receive little consideration in engineering the job of a millwright in a cutting machine operation or the biomechanics of baggage handling for ground personnel. Ergonomic hazards are defined as physical stressors and environmental conditions that pose a potential risk of injury or illness to a worker. These physical stressors are described as repetition, force, posture, and vibration. To these stressors must be added the issues of poor job design; inadequate workstation layout; and negative work organizational factors such as work rates, shift work, work-rest cycles, and managerial insensitivity.
Human-related error counts for approximately 70% of all transportation accidents including aviation. Fatigue is a significant factor that contributes to human error in the industry. The Air Transport Association (
ATA) has developed an alertness management guide to assist those in industry in managing, preventing, and providing countermeasures to operational fatigue. In December 2000, the
ATA established an Alertness Management Initiative Scientific Advisory Board to address alertness in flight operations (
21).
Disregarding ergonomic factors can lead to work related injury and disability. Assembly-line work that requires a repetitive cycle of less than 30 seconds is associated with upper extremity musculoskeletal injury. The application of poor body mechanics to lifting, pulling, or pushing is a major contributor to low back pain and disability. The significant increase in carpal tunnel syndrome over the last 20 years has been attributed in part to repetitive injury and biomechanical strain. In 1985, NIOSH released its Proposed National Strategy for the prevention of work-related musculoskeletal injury (
22). This documented the need to control work-related low back injuries as a national goal. One of the resulting strategies was the development of new lifting guidelines. This effort led to the development of
the revised 1961 Lifting Equation for Material Handling (
23). In 2000,
OSHA promulgated a new standard for ergonomics that had been in preparation for nearly a decade. Within months of its publication and before its implementation, it was rescinded by Congress. To date (2007), a new ergonomics standard has not been forthcoming.
Currently
OSHA has a four-prong approach approved to address ergonomic issues as follows:
Guidelines that are developed for specific industries.
Inspections for ergonomic hazards with citations issued under the general duty clause.
Outreach and assistance to employers for program development.
Formation of a national advisory board
To determine ergonomic risk, it is helpful to perform a job analysis that evaluates job requirements and psychophysiologic variables, as well as environmental factors. This is the hallmark of prevention: anticipating risks, validating the degree of risk, and then modifying or reducing the risk to avoid biomechanical injury.