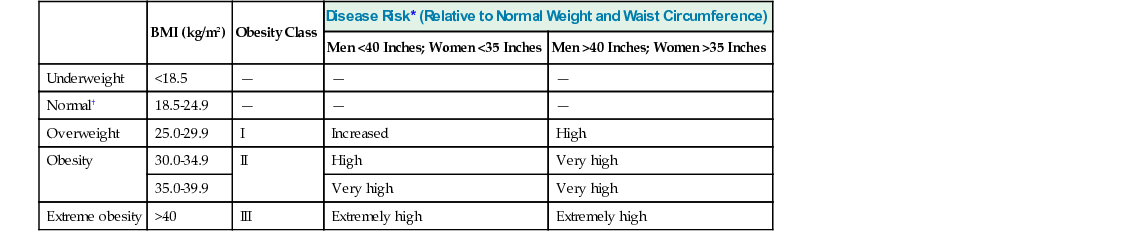
Krupa Shah, Dennis T. Villareal Obesity is defined as an unhealthy excess of body fat, which enhances the risk of morbidity and untimely mortality. Obesity is a growing epidemic in developed countries and is also becoming increasingly problematic in our aging population. Obesity in older adults is accompanied by an untoward burden of chronic disease, metabolic complications, and a worsening in quality of life. More important, obesity in older adults exacerbates the age-related decline in physical function, which leads to frailty and disability. The current treatment designed for weight loss in older persons includes lifestyle intervention (diet, exercise, and behavior modifications), pharmacotherapy, and surgery. Existing evidence indicates that weight loss therapy in obese older adults prevents or delays functional decline and medical complications and improves quality of life. However, clinicians prescribing weight loss therapy for older adults must consider adverse effects on patients’ muscle and bone mass. This chapter describes the clinical importance of obesity in older adults and provides medical professionals with evidence-based guidelines for treating obesity in older adults. Body mass index (BMI) and waist circumference are widely used and accepted as simple methods to classify overweight and obesity. BMI is calculated as weight (kg)/height squared (m2). However, the measurement of height is often unreliable and impractical in older adults in nursing homes. In this situation, using alternative measurements such as arm span may be more reliable.1 Central obesity, as measured by waist circumference, is the excessive accumulation of fat in the abdomen. It is an independent predictor of comorbidities such as diabetes, hypertension, and cardiovascular disease.2 Table 80-1 incorporates both BMI and waist circumference in the classification of overweight and obesity and estimates relative disease risk.3 TABLE 80-1 Classification of Overweight and Obesity by Body Mass Index (BMI), Waist Circumference, and Associated Disease Risk18 The prevalence of obese older adults is rising sharply. According to National Health and Nutrition Examination Survey (NHANES) data from the period 1991 to 2000, the prevalence of obesity increased dramatically for those in the age ranges of 60 to 69 and 70 to 79 years,2,3 by 56% and 36%, respectively.4 More recent estimates suggest that 37% of adults 65 years of age or older are obese (BMI ≥ 30 kg/m2), and such prevalence is expected to become even more evident with the aging of baby boomers.5 The prevalence of obesity in older adults is likely to continue to increase and challenge our health care systems. Moreover, obesity poses an increasing dilemma for long-term care facilities and raises concerns about nursing home preparedness and access.6 The global growth rate for age-related obesity in developed counties is predicted to be 15% to 20%, and the same trends are being observed in developing countries as they gain more economic affluence.7 Aging is associated with significant changes in body composition. After the age of 30 years, individuals tend to show a progressive decrease in fat-free mass (FFM), such as muscle and bone, and an increase in fat mass. Moreover, data from some studies suggest an accelerated loss of FFM in women after they reach age 60 years.8,9 FFM attains its peak during the third decade of life, whereas fat mass reaches its peak during the seventh decade and is followed by a subsequent decline.9 In addition, aging is associated with the redistribution of body fat. The intraabdominal fat (central adiposity) increases with aging, whereas the subcutaneous fat and total body fat decrease with aging.10 The hormonal changes with aging may explain some of the age-related shifts in proportion of fat and FFM. These age-related changes include a reduced production of the anabolic hormones, growth hormone, insulin-like growth factor 1, testosterone, and dehydroepiandrosterone (DHEA), without a concomitant decline in the catabolic hormone cortisol.11,12 Obesity results when total energy intake exceeds the energy output. Energy intake neither changes nor declines with advancing age. Hence, the decrease in total energy output is an important contributor in the gradual accumulation of body fat with aging. Aging is associated with a decrease in all major components of energy output. These components are basal metabolic rate (which explains 70% of energy output), thermal effect of food (10%), and physical activity (20%). The resting metabolic rate decreases with age, largely because of an age-related decline in FFM.13 The thermic effect of food also declines with aging. The decline in physical activity with aging contributes approximately 50% of the reduction in energy output that occurs with aging.14 Obesity is associated with several complications that are commonly known to increase mortality and morbidity15 (Table 80-2). In addition, obesity has a detrimental effect on physical function and quality of life in older adults. These adverse effects of obesity are discussed in this section. TABLE 80-2 Adverse Effects of Obesity in Older Adults Obesity is associated with increased cardiovascular and overall mortality in both younger and older adults.16 Even though obesity is associated with a higher relative risk of death for younger adults than for older ones, an elevated BMI increases absolute mortality and health risks linearly up to 75 years of age.17 The relationship of obesity in individuals 75 years or older with total mortality is equivocal. In very old persons, the prevalence of obesity could actually be lower. One explanation for this demographic shift is selective mortality. The underlying diseases can themselves increase the risk of early mortality in obese adults, thus causing an underestimation of the relation between obesity and mortality in older adults. Those who are vulnerable to the adverse effects of obesity die at a younger age. The remaining surviving groups of obese older adults are called the “resistant” survivors. Obesity and increased abdominal fat are associated with increased morbidity (see Table 80-1), mortality, and poor quality of life.15 The prevalence of medical conditions commonly associated with obesity (such as hypertension, diabetes, dyslipidemia, and cardiovascular disease) increases with age.18 Therefore, obesity and weight gain during middle age may contribute to medical complications and the increasing health care expenditures that occur during old age.19 The age-related glucose intolerance increases with abdominal obesity and lack of physical activity. Older people who are physically active and do not have increased abdominal girth are much less likely to develop insulin resistance and type 2 diabetes mellitus.20 In addition, obese older adults have a higher prevalence of dyslipidemia (high triglyceride and low high-density lipoprotein [HDL]) and hypertension.21,22 In a 15-year longitudinal study, increased BMI in older men was associated with an increase in new cases of coronary heart disease and cardiovascular disease mortality.23 Advancing age causes physical dysfunction because of both a progressive decline in muscle mass and strength and an increase in joint immobility and arthritis.24 These functional limitations adversely affect the activities of daily living (ADLs) and quality of life. Obesity exacerbates this age-related decline in physical function. In addition, medical comorbidities such as diabetes, heart disease, and pulmonary disorders frequently coexist with obesity and contribute to functional decline. Moreover, older adults who are obese (BMI ≥ 30) have a greater rate of nursing home admissions than those who are nonobese (BMI, 18.5-24.9).25 Both cross-sectional studies and longitudinal studies have consistently demonstrated a strong link between a decline in physical function of older persons and an increase in BMI.26,27 Obesity is also associated with frailty syndrome in older adults. In one study, 96% of community-living obese (BMI > 30) older subjects (65 to 80 years old) were frail, as determined by physical performance test scores, peak oxygen consumption, and self-reported ability to perform ADLs.26 In another study, which was conducted in older women (70 to 79 years old), obesity was linked with a marked increased risk of frailty, determined by weakness, slowness, weight loss, low physical activity, and exhaustion.28 In a study of community-dwelling older adults, frailty was related to BMI in a U-shaped manner (i.e., increased frailty in people with extremes of low or high BMI). However, in people with large waist circumference (≥35 inches in women and ≥40 inches in men), frailty was shown to exist in all BMI categories.29 Despite having higher absolute muscle mass, obese older adults are particularly susceptible to the adverse effects of obesity because not only do they have smaller muscle mass relative to their body weight (relative sarcopenia), but they also have age-related decline in muscle mass leading to sarcopenic obesity.30,31 With higher fat mass and lower muscle mass, physical activity becomes progressively more difficult. Hence, sarcopenic obesity acts synergistically with aging to augment disability by leading to functional dependence, inactivity, and poor quality of life. It should be noted that a potential benefit of obesity with aging is the protection from osteoporosis-related fractures. Higher body weight is associated with greater bone mineral density.32 This is explained by the bone-stimulating effects of carrying extra body weight as well as hormonal changes (e.g., increased adipose tissue conversion of androstenedione to estrone). Heavier individuals have been found to have higher bone densities even in their non–weight-bearing bones. Furthermore, in the event of a fall, the extra cushioning provided by body fat can serve as protection against fractures, particularly of the hip. Adipose tissue is recognized as a source of inflammatory mediators by producing cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-6.33 It appears that the relationship between obesity, insulin resistance, and atherosclerosis may depend partially on the increased production and the release of these inflammatory mediators from adipose tissue. It is postulated that the visceral fat (intraabdominal fat) is most responsible for producing these deleterious cytokines, which in turn leads to diabetes, coronary artery disease, and malignant disease more commonly seen in older adults. Similarly, cytokines and inflammatory mediators produced by adipose tissue may play an important role in the pathophysiology of sarcopenic obesity.34 A better understanding of the mechanisms that lead from gain in fat mass to muscle loss, or vice versa, seems to be crucial. More research is needed to better characterize this new area of study. Because weight loss results in a decrease in both fat mass (75%) and FFM (25%),35 it is possible that weight loss in obese older persons could worsen the age-related loss of muscle mass. Nevertheless, adding regular exercise to a weight loss program can attenuate the loss of FFM. This effect was observed in randomized controlled trials (RCTs) conducted on obese older subjects. There was no significant difference in the loss of FFM after regular exercise was added to a diet-induced weight loss program compared to a control group that did not lose weight.30,36 It is well known that weight loss improves or normalizes metabolic abnormalities associated with obesity in young and middle-aged persons.37 Clinical trials conducted in obese older adults have shown similar results. It was observed that a decrease in multiple coronary artery disease risk factors (including the prevalence of the metabolic syndrome) and insulin resistance, as well as an increase in insulin secretion, resulted from weight loss therapy in obese older adults.38,39 The results of a recent RCT in obese older subjects showed weight loss improves insulin sensitivity and other cardiometabolic risk factors, but continued improvement in insulin sensitivity is only attained when exercise training is added to weight loss.40
Obesity
Introduction
Measurement
BMI (kg/m2)
Obesity Class
Disease Risk* (Relative to Normal Weight and Waist Circumference)
Men <40 Inches; Women <35 Inches
Men >40 Inches; Women >35 Inches
Underweight
<18.5
—
—
—
Normal†
18.5-24.9
—
—
—
Overweight
25.0-29.9
I
Increased
High
Obesity
30.0-34.9
II
High
Very high
35.0-39.9
Very high
Very high
Extreme obesity
>40
III
Extremely high
Extremely high
Obesity Prevalence
The Relationship between Body Composition and Aging
Causes of Obesity in Older Adults
Adverse Effects of Obesity
Disorders Directly Caused by Obesity
Disorders Aggravated by Obesity
Metabolic syndrome
Osteoarthritis
Hypertension
Urinary incontinence
Dyslipidemia
All cardiopulmonary abnormalities
Coronary artery disease
Postoperative complications
Diabetes mellitus
Cataracts
Neoplasia
Obstructive sleep apnea
Mortality
Comorbid Disease
Functional Impairment and Quality of Life
Beneficial Effects of Obesity
Mechanisms by Which Obesity Increases Mortality and Morbidity
Effects of Intentional Weight Loss in Older Adults
Body Composition
Medical Complications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Obesity
80





