In patients with cancer, malnutrition may appear simultaneously with the disease. Patients with cancer often exhibit anorexia because of decreased nutritional intake with resultant weight loss. There may be an increased nutritional requirement because of the increased demands of the patient and the tumor. Resting metabolic rates can vary greatly, but in as many as 60% of patients, the rate may be elevated. The stage of malnutrition in patients with cancer can lead to cachexia with weakness and tissue wasting. The extent of malnutrition in the patient may be greater than can be explained by decreased nutritional intake. Metabolic abnormalities include an abnormal response to glucose tolerance testing, increased gluconeogenesis (which can result in decreased muscle protein synthesis), and abnormalities in protein and fat metabolism. A patient with a malignancy may need additional nutritional support while undergoing intensive treatment, which can include surgery and chemotherapy. Parenteral nutrition seems to improve a patient’s tolerance of the treatment and improves her nutritional state; however, parenteral nutrition has not been shown to improve survival.
The malnutrition seen in cancer patients is commonly referred to as cancer cachexia. Nutritional depletion is seen as a protein-calorie malnutrition with a loss of body cell mass. The importance of protein-calorie nutrition is its association with increases in postoperative complications, deficiencies in immune function, and poorer tolerance of therapy.
Dietary nutrients required for good health include water, protein, fat, carbohydrates, vitamins, and minerals. Energy is required for normal body function, growth, and repair. Protein is necessary for growth and development to maintain body structures and function. It is the source of the essential amino acids and nitrogen needed for the synthesis of nonessential amino acids. Dietary protein replaces the essential amino acids and nitrogen that are lost through protein turnover and normal body functions. During illness, protein requirements increase. Nitrogen balance is essential for good health and requires intake of protein and energy. At higher energy intakes, less protein is needed to achieve nitrogen balance. Nitrogen is lost continuously in the body through normal body functions. Fat is the food substance with the highest concentration of calories.
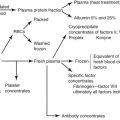
The visual protein compartment is best measured by assessment of the plasma albumin, transferrin, and total lymphocyte count. Albumin is the major determinant of plasma colloidal osmotic pressure because its large size does not permit it to pass the capillary membrane. The appearance of edema is often a sign of low serum albumin. Serum levels lower than 3.0 g/dL are reflective of nutritional deficiency. Transferrin is a protein of hepatic origin and transports iron. The level is reflective of the patient’s ability to make serum protein. Transferrin levels are more sensitive than albumin levels because of its shorter half-life (8 days compared with 20 days), and it is preferable to evaluate the efficacy of nutritional therapy. The response of a patient’s total lymphocyte count to nutritional therapy may also be a favorable prognostic sign during the first 7 to 14 days of therapy ( Table E.1 ).
|
* Routine use of total parenteral nutrition (TPN) in patients with cancer is not indicated.
Linoleic acid is the only essential fatty acid required in the diet; it is necessary for the synthesis of arachidonic acid, which is a major precursor of prostaglandin. Linoleic acid comes mainly from polyunsaturated vegetable oils. A deficiency of essential fatty acids results in poor wound healing, hair loss, and dermatitis. Fatty acids and cholesterol make up most of the fat in our diets. Carbohydrates include sugar, starch, and fibers. When carbohydrates are not included in the diet, ketosis begins to occur, and there is excessive breakdown of protein as amino acids are used for gluconeogenesis. Water-soluble and fat-soluble vitamins cannot be synthesized in adequate amounts by the body. Fat-soluble vitamins are required for absorption, transport, metabolism, and storage. They are not excreted in the urine like the water-soluble vitamins, and an excess accumulation can lead to well-known toxic conditions. Major minerals, as well as trace elements, are important in human nutrition.
Lack of appetite with reduction in food intake is a key factor in cancer cachexia. The role of the neurotransmitter serotonin appears to be central to appetite. Inhibition of serotonin increases appetite and food intake in animals. Cancer patients also report a loss of taste and smell with a resulting loss of appeal of most foods. Weight loss may also be greatly influenced when the location of the tumor affects the ability to take nutrition (eg, a mass causing a partial bowel obstruction). Cytokines produced by the patient in response to a growing neoplasm may result in nutritional derangements. Cytokines can regulate appetite and metabolic rate, so they can be very important factors. Dudrick and coworkers suggest that patients who have a 10-lb weight loss or a 10% decrease in body weight 2 months before assessment, serum albumin of less than 3.4 g/dL, alergy to four of five standard skin test antigens, and a low total lymphocyte count and who cannot or will not eat enough are candidates for nutritional assessment. Nutritional history, with a 24-hour dietary recall, can be used to assess nutritional intake. Anthropometric measurements are useful when assessing the patient’s nutritional status. Relative body weight is probably the most useful of these measurements because rapid weight loss is usually an indication of protein-calorie undernutrition. The triceps skinfold test assesses fat stores, and midarm circumference tends to assess protein status. Edema, which is often seen with protein-calorie deficiency, can mask true weight loss and muscle wasting. Serum albumin is probably the single most important test for determining protein calorie undernutrition. Albumin is the main plasma protein needed to maintain plasma osmotic pressure as well as other functions. In a patient with low albumin, morbidity and mortality are increased. Albumin can be influenced by conditions other than malnutrition and may be affected by hydration status. Transferrin binds and transports iron in the plasma and is a good indicator of protein nutritional status. The extent of malnutrition depends on the type and site of the cancer. Cancers such as ovarian cancer, with its potential effect on the gastrointestinal (GI) tract, appear to contribute to malnutrition to a greater degree than does cervical cancer. As expected, malnutrition becomes worse as the cancer progresses. The mechanism of cancer-related malnutrition is unknown. There are probably multiple contributing factors. Decreased food intake because of anorexia, early satiety, nausea, and vomiting can all play a role. Poor absorption of nutrients can also be a contributing factor. Food aversion, particularly in patients undergoing chemotherapy or irradiation, is well known. Change of taste and smell can contribute to decreased intake. Generalized weakness may also contribute to decreased food intake. Decrease in total lymphocyte count (<1200 cells/mL) is also suggestive of malnutrition. Creatinine height index (CHI) may be helpful because urinary creatinine excretion is proportional to total body muscle mass. As muscles become depleted, creatinine excretion falls. A CHI of 80% or more usually indicates a normal lean body mass. A CHI between 60% and 80% indicates moderate depletion; a CHI of less than 60% indicates severe depletion.
Enternal Nutrition
Numerous clinical trials have been published using aggressive enteral nutritional support as a supplement during cancer therapy in patients who would not eat well. The trials are not consistent in demonstrating benefit of enteral nutrition. However, it is a well-accepted concept that enteral therapy is the preferred route for feeding cancer patients when the GI tract is not obstructed. Methods of enteral nutrition vary from frequent snack between meals to the insertion of a comfortable nasogastric feeding tube on a continuous drip of nutritional supplements. Others have used gastrostomy or jejunostomy feeding tubes.
The role of total parenteral nutrition (TPN) in patients with cancer has yet to be determined. TPN can correct nutritional deficits that commonly occur in patients with cancer. TPN can also improve nitrogen balance and decrease catabolism. Glucose turnover and clearance rates are increased, gluconeogenesis is suppressed, and free fatty acid oxidation is increased. TPN can increase body weight and reverse serum markers of malnutrition; however, as an adjuvant to cancer therapy, the results have not been encouraging. TPN has not added to lean body mass or eliminated the GI or hematologic toxicity associated with chemotherapy. In patients treated with chemotherapy, response rates and survival have not been increased with TPN. Although irradiation can contribute to poor nutrition (eg, diarrhea, enteritis, and malabsorption), particularly to the GI tract when gynecologic cancers are treated, TPN has not produced a significant improvement regarding treatment response, tolerance to treatment, local control, survival, or decreased complications of therapy. Nutritional support for patients with cancer requiring surgery is also ill defined. Malnourished patients undergoing surgery have a higher postoperative morbidity and mortality compared with well-nourished patients. Whether TPN can affect morbidity and mortality in patients with cancer is undetermined, and the concern that TPN may stimulate tumor growth is unfounded. Although routine use of TPN in patients with cancer is not warranted, it may be indicated in severely malnourished patients undergoing surgery or for those with postoperative complications.
Nutritional supports are of two main types: enteric and parenteral. For a patient with a functional GI tract, enteric nutrition may be considered through the use of a nasoenteric tube. A gastrostomy or jejunostomy tube may also be used. Obviously, GI dysfunction is a contraindication to this method. Nevertheless, this method appears to be cost effective; it probably maintains the GI mucosa integrity, provides a normal sequence of intestinal and hepatic metabolism before systemic distribution, appears to preserve normal hormonal patterns, and avoids the risk of sepsis. Enteric solutions differ in composition, calorie content, and multiple other factors. These solutions are usually complete because they contain a full supplement of nutrient requirements or incomplete when they are designated to contain a specific macronutrient such as fat, protein, or carbohydrate. Most solutions contain 1000 calories and 37 to 45 g/L of protein. Elemental diets consist mainly of amino acids and simple sugars. They are extremely hypertonic and may induce diarrhea, which may be corrected with a formula of lower osmolarity. Electrolyte imbalance and glucose intolerance can also occur.
Many patients with cancer who require nutritional supplementation will need TPN. In some cases, TPN can be administered through a peripheral vein, particularly if TPN is to be given for only a short amount of time. Although adequate protein can usually be infused peripherally, high-caloric supplementation is usually given centrally. Fat solutions, which can account for a high caloric intake, can be given peripherally. Major complications of peripheral TPN are thrombophlebitis and infiltration. In most cases, TPN is given through a central vein—either the subclavian vein or a major neck vessel. The catheter can be inserted in the superior vena cava, which allows rapid infusion of hypertonic solutions without difficulty. Infusion of parenteral solution should be started slowly to prevent hyperglycemia. If glucose intolerance develops, a small amount of insulin is used to control blood sugars. Meticulous care must be taken of the central catheter because this site can be a major source of infection. Frequent changing of intravenous tubing and filters and the catheter is required routinely. TPN is usually managed as a team endeavor with the attending physician, nutritionist, nurse, pharmacist, and dietitian. Daily requirements must be standardized regarding calories, proteins, fat, minerals, vitamins, and trace elements. These should be varied as the situation demands. Metabolic complications may include hyperglycemia or hypoglycemia, hyperosmolarity, azotemia, hyperchloremic metabolic acidosis, mineral electrolyte disorder, liver enzyme elevations, and anemia. In many hospitals, standard hyperalimentation solutions with appropriate nutrients have been formulated, and adjustments are made for specific needs. Intense metabolic monitoring is required in these patients, and established hospital protocols are now available in many institutions.
Today, both enteric and parenteral nutritional support can be implemented successfully on an outpatient basis. Indications are not uniformly agreed on for this method of nutrition. In patients with cancer, nutritional support may be indicated to help satisfy nutritional needs while toxicity of treatment is abating. Most authorities do not believe that home nutritional support is needed for terminally ill cancer patients.
A typical nutritional guideline for adult patients is shown in Table E.2 (see the Expert Consult website). Many institutions have nutritional protocols in place. Although there may be variations on the theme, these guidelines have become relatively standardized.