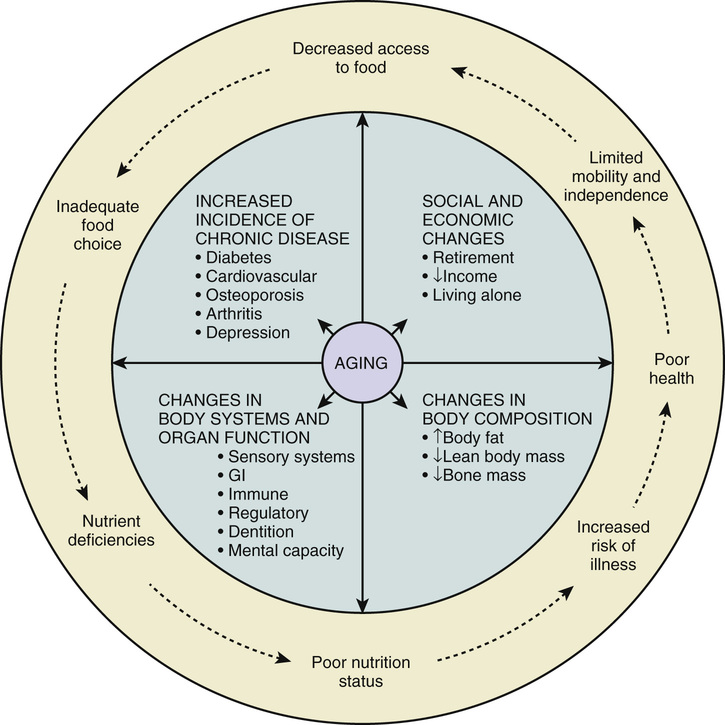
C. Shanthi Johnson, Gordon Sacks In caring for the older adult population, the nutrition goals are to maintain or even improve their overall health and quality of life as well as to prevent and/or treat age- and nutrition-related problems by improving the nutritional status of individuals and population groups. Whether defined as “the condition of a population’s or individual’s health as affected by the intake and utilization of nutrients and non-nutrients”1 or as the degree of balance between nutrient intake and nutrient requirements, nutritional status is extremely important to overall health and to maintaining optimal nutritional status. Not only is optimal nutritional status fundamental to overall health and well-being as people grow older, but it has been shown to influence the aging process, various physiologic systems and functions, body composition, and the onset and management of various chronic conditions. The process of aging also affects nutritional status. Specifically, the aging process has been shown to directly contribute to the changes in nutritional needs with requirements of various nutrients decreasing, increasing, or remaining the same.2 With aging, changes in economic and social status arise that contribute to decreased access to food, poor food choices, nutrient deficiencies, and poor nutritional status, which in turn lead to increased risk of illness, poor health, and limited mobility and independence, as illustrated in Figure 79-1.3 In addition, the nutrition and health status of individuals and populations are influenced by social determinants such as income, educational level, social support, gender, culture, and other factors outlined in the population health framework.4 These factors partly account for the wide and stubbornly resistant disparities in nutritional and health status that exist in populations. For example, research in the area of food costing shows that seniors living alone are not able to afford nutritious diets.5 A study investigating supplement use among older adults showed that the consumption of vitamin and mineral supplements was higher among those with higher levels of education.6 Furthermore, seniors who live alone and lack social support tend to be at greater nutritional risk compared to older individuals with social support.7 There are many physiologic factors that impact the nutritional status and well-being of older adults. An inadequate or excess intake of nutrients is the result of ingestion and utilization of nutrients from a variety of dietary sources, as well as other various elements (e.g., age-related changes, medication intake, socioeconomic factors, and functional and cognitive capacity). These factors facilitate the depletion or storage of tissue stores and changes in plasma nutrient levels, enzymatic activity, and other physiologic functions, which affect anthropometric indicators (e.g., weight, body composition). As a result, anthropometric measures, as well as biochemical, clinical, and dietary factors are critical and must be considered in the assessment of an individual’s nutritional status. Anthropometric measures are used to assess nutritional status through the examination of body proportions and composition, as well as the fluctuations in these indicators over time, and include body weight, weight history, height or other estimates of stature, body mass index (BMI), skinfold thickness, and circumference.8,9 Self-reported measures are often inaccurate, and standardized measurement protocols should be adopted by trained technicians to reduce measurement error.10,11 Body weight is a key indicator in nutritional status, and one’s weight history serves as an indicator of nutritional risk. Periods of excessive or significant weight loss include 2% body weight in a week, 5% in a month, 7.5% in 3 months, or 10% in 6 months. In addition to weight changes, height changes, which are largely due to compression of the spine, are reliable indicators of an at-risk individual. If unable to stand or stand straight, estimates of stature can be estimated via arm span, demi-span, or knee height. Arm span measurements can determine the maximal height in adulthood rather than one’s actual height, while age-, gender-, and race-specific equations are used to estimate stature from knee height measures12 with supine knee height valued as more reliable than seated knee height. Once height and weight measures are obtained, BMI can be calculated. Body weight (kg) is divided by height squared (m), which evaluates weight independent of height but does not directly measure body fat. For older adults, a BMI of less than 24 is associated with poor nutritional health, a BMI between 24 and 29 is believed to be a healthy weight, and a BMI of over 29 is seen as overweight and may lead to health problems.13 Skinfold thickness measurements are used to determine body fatness. However, in older adults, skin changes in thickness, elasticity, and compressibility and skinfold thickness measurements are not reliable measurements. Body fat stores can be assessed through circumference measurements (e.g., waist, waist-to-hip ratio, and upper arm circumference), much like measures that are used to estimate skeletal muscle mass (somatic protein stores). Body fat measurement can be used as a quick screening tool to pinpoint high-risk individuals who may be susceptible to under- or over-nutrition and are useful alone or combined with height and weight measurements. Another useful measure for individuals at risk for nutritional problems is biochemical markers, which can be used to find subclinical deficiencies (e.g., through blood or urine specimens). Through such tests, biochemical markers of visceral protein status can be substantiated; these markers include serum albumin, thyroxine-binding prealbumin, serum transferrin, and retinol-binding protein as well as total lymphocyte counts. Although serum albumin is a commonly used marker because it can predict mortality in older adults, it is not always reliable. Values can be elevated as a result of dehydration, or values can decline because of inflammation, infection, and age-related degeneration of muscle mass. Other biochemical measures such as total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglycerides are used to assess lipid status and are also used to measure micronutrient status (e.g., iron status). Low total cholesterol is associated with poor nutritional status and may be a predictor of mortality in older adults. Hematologic assessments can also be used to screen for malnutrition in older adults and include hemoglobin, hematocrit, mean cell volume, mean cell hemoglobin concentration, mean cell hemoglobin, and total iron binding capacity. A combination of these measures is used for a proper clinical diagnosis and can be compared to normative age and gender group values. Clinical indicators are also used to assess nutritional status. The components of clinical assessment can include medical history and physical signs and symptoms associated with nutritional deficiencies, functional status, and cognitive status. Some clinical signs and symptoms are nonspecific and attributed to the aging process rather than to a particular nutritional deficiency. Functional status can be assessed in several different ways. Most commonly various tools are used to assess the person’s abilities to perform basic activities of daily living (ADLs), which include basic self-care such as bathing, grooming, dressing, feeding, and toileting, and instrumental activities of daily living (IADLs), which include cooking, shopping, housekeeping, and managing one’s own affairs. These can serve as clinical indicators useful in the assessment of nutritional status. The inability to execute such tasks may indicate a higher risk of poor nutrition, although some clinical signs may be nonspecific and attributed to aging rather than to a specific deficiency. Clinical assessment can include physical signs and symptoms affiliated not only with nutritional deficits but also with functional and cognitive status. Both functional and cognitive status can be assessed in multiple ways. Dietary assessment is an integral component in the measurement of nutritional status allowing the evaluation of foods consumed and eating patterns. Dietary assessment methods can be categorized as retrospective or prospective. A retrospective assessment involves the recall of all foods and fluids consumed in a particular time frame (often 24 hours). Retrospective assessment can be unreliable if the individual has problems with his or her cognitive status. In this case, a prospective assessment may be favored, as this involves keeping a written record of all foods and fluids consumed in a given period of time (e.g., 3 days [including 2 weekdays and a weekend day] or 7 days). Although this type of assessment aids those with cognitive challenges, it poses a problem for individuals who suffer from a particular functional disability, such as arthritis of the hand or poor vision. A 3-day food record with intakes of 2 weekdays and 1 weekend day recorded is considered to be one of the better dietary assessment methods because it does not depend on memory and can provide detailed intake data, although no single best method exists. Given that a comprehensive assessment of nutritional status is complex and time consuming, rapid screening is beneficial to identify those who might at risk for poor nutrition and individuals who might need in-depth assessment. Several screening tools exist. The DETERMINE checklist developed as part of the Nutrition Screening Initiative provides public awareness about basic nutrition information and can help identify individuals at risk for poor nutrition in community settings. The checklist is widely used in the United States14 and is executed in two stages or levels. Level I can include assessments of body weight, eating habits, living environment, and functional status (particularly ADLs and IADLs) and is usually filled out by the individual’s primary caregiver.15 The level II screen can include anthropometric measurements, laboratory data, polypharmacy, and cognitive status assessments. Based on the assessment, a specific nutritional care plan or support is provided. In Canada, a screening tool titled Seniors in the Community: A Risk Evaluation Tool for Eating and Nutrition Version II (SCREEN II) has been developed for assessing nutritional risk among community-dwelling seniors.16 The Mini Nutritional Assessment (MNA) is also widely used for initial screening and assessment for individuals in the community as well as in long-term care settings.17,18 In a variety of settings, using different instruments, malnutrition has been linked to frailty.19,20 Indeed, not only are nutritional parameters commonly used in frailty assessment tools,21,22 but it has been suggested that a short version of the MNA can be used to screen for frailty.23 Still, comprehensive assessment can reveal an important interplay of other factors, including medications.24 In addition to these commonly used screening tools, several others exist. These include Payette Nutrition Screening Scale, Nutritional Risk Index (NRI), Nutritional Risk Score (NRS), Nutritional Risk Assessment Scale (NuRAS), Prognostic Nutritional Index (PNI), Sadness-Cholesterol-Albumin-Loss of weight-Eating-Shopping (SCALES), and Subjective Global Assessment (SGA). Screening tools are beneficial for helping identify individuals at risk or as educational tools, and they can provide simple, rapid, and reliable assessment.25 However, some clinicians suggest that screening tools are of limited value in apparently healthy older adults.26 It is therefore important to select and use appropriate screening tools based on the target group (e.g., home care, long-term care), ease of use, and psychometric properties (validity/reliability). While researchers and clinicians have traditionally relied on the nutritional assessment and screening based on anthropometric, biochemical, clinical and dietary considerations as well as the presence of various risk factors that could predispose one to have less than optimal nutritional intake, we need to consider what the appropriate indicators of nutritional health are in the context of the aging population. Is it the nutrient intake of macro- and micronutrients or BMI (an indicator of weight status based on the proportion of weight for height) as we have traditionally measured, or should we pay attention to the variety, moderation, and balance in food group consumption, or should we include indicators of food security such as availability, access, and affordability of nutritious diet? How do we measure availability and access to traditional diet and the quality and safety of traditional foods or cultural foods for minority populations? There is a considerable need for identifying appropriate indicators of nutritional health among the aging population. The physiologic, functional, and overall health changes that accompany aging affect the requirements for some nutrients and how nutrient needs should be met. Therefore, determination of a person’s nutritional requirements is critical in order to ensure optimal nutrient intake is provided. Reduction in energy requirements is one notable difference between individuals older than 65 years of age and their younger counterparts.27 For example, it is estimated that total daily energy expenditure decreases approximately by 10 kcal/yr for men and 7 kcal/yr for women aged 30 years and older.28 Therefore, a man who needs 2200 kcal at age 20 requires only 1700 kcal/day at age 70. In older adults, the decrease in energy needs is largely attributed to the age-related reduction in resting metabolic rate, reduced lean body mass, and decreased physical activity level.29–31 Yet, other problems, including chewing and swallowing difficulties, living alone, and low income contribute to a decline of energy intake in older adults. Whereas total energy intake significantly increased in the U.S. older adult population from 1977 to 2010, average energy intake decreased with increasing age, with adults older than 75 years having the lowest energy intake for all years.32 The third National Health and Nutrition Examination Survey (NHANES III, 1988-1991) reported that women and men aged 60 to 69 years and 70 to 79 years consumed an average of 534 kcal/day and 658 kcal/day less than women and men aged 30 to 39 years, respectively.33 Different methods exist for estimating the energy requirements of older individuals, and knowledge of patient-specific information (such as height, weight, and age) is required. One simple method, only requiring a patient’s weight, estimates energy expenditure in the range of 20 to 25 total kcal/kg/day. Thus, the energy requirements of an older 70-kg individual could be met with the provision of 1400 to 1750 total kcal/day. These estimates appear to be appropriate because indirect measurements of energy expenditure in critically ill older adults were found to be 22 to 25 kcal/kg/day.34 If weight gain is the desired objective, an increase in calories up to 30 kcal/kg/day may be warranted. One of the most widely used methods for predicting energy expenditures in older adults are the Harris-Benedict equations (Table 79-1).35 These equations are based on the measurement of oxygen consumption and carbon dioxide production using direct calorimetry. Subjects used in the development of these equations in the year 1919 ranged in age from 15 to 74 years. However, these equations are often considered inaccurate for older adults because only 9 of the 239 healthy male and female subjects of the population measured were older than 60 years. Some consider equations established by the World Health Organization for people older than 60 years to be more precise than Harris-Benedict equations (see Table 79-1). Recommendations from the National Research Council include multiplying the calculated energy expenditure by coefficients accounting for various levels of physical activity.36 An activity coefficient 1 to 1.12 times the energy expenditure is used for older adults who are sedentary or fairly inactive. Activity coefficients of 1.27 to 1.45 should be used to account for energy expended by older adults with highly active lifestyles. Despite the decline of energy requirements with increasing age, it is important that older adults meet intake of protein, fat, and carbohydrate that falls within the acceptable macronutrient distribution range. For protein, this corresponds to between 10% and 35% of total energy intake. Traditionally, guidelines for dietary protein intake have recommended 0.8 g/kg of body weight in order to maintain protein equilibrium and avoid loss of lean body mass for all adults, regardless of age. However, evidence suggests as much as 1.0 to 1.2 g of protein/kg of body weight is required to meet the needs of healthy older adults.36,37 The increased intake is necessary, in part because of decreased lean body mass, changes in metabolism, changes in body composition, and protein utilization efficiency associated with aging. In addition, protein needs for older adults may reach 1.2 to 1.5 g/kg body weight for those with acute or chronic diseases and as much as 2.0 g/kg body weight for those with severe infections, surgery, or trauma.36 Geriatric patients generally tolerate moderately high protein intakes without deterioration in renal function. However, those patients with existing renal disease should avoid high-protein diets as they may hasten a greater decline in renal function.38 Sarcopenia is used to describe the age-associated loss in skeletal muscle and its functional consequences.39 While the role of dietary protein in the causes and prevention of sarcopenia is unclear, the loss of muscle mass has been linked to sedentary lifestyles, neurogenic processes, and dietary protein deficiencies. There is no consensus on the recommended daily protein intake to enhance muscle protein anabolism and minimize the loss of muscle mass with age. Overall, dietary data from the United States and Canada show protein intakes decline with increasing age. Therefore, intake of high-quality protein sources, such as fish, lean meat, dairy products, eggs, and legumes are recommended at each meal throughout the day.40,41 Another key factor in maintaining healthy nutritional status is an appropriate intake of dietary fat. Fats contain twice as many calories per gram as carbohydrates or proteins, and given the fact that higher intakes of dietary fat are associated with an increased risk of developing diabetes, heart disease, and other chronic ailments, it is recommended that lower fat choices such as skim milk, rather than whole milk, are made by older adults. Ideally, total fat intake should fall within 20% to 35% of total daily energy intake; however, if an older adult is unable to consume enough of his or her daily energy requirement, the risks associated with a higher fat intake may be overlooked in favor of meeting the necessary daily energy requirement. According to the dietary reference intakes (DRI) recommendations developed by the Institute of Medicine, older adults should acquire 45% to 65% of their daily energy intake from complex carbohydrates, such as whole grains, vegetables, and fruits. Dietary fiber requirements decrease for older adults because of overall decreased energy intake. After age 50, 30 g/day for men and 21 g/day for women is needed to improve gastric motility, maintain healthy blood glucose levels, and reduce cholesterol.28 Along with these fiber requirements, fluid intake must be optimal to ensure regular gastrointestinal motility. To maintain a healthy nutritional diet and nutritional status, one must maintain an opportune intake of micronutrients, specifically vitamins and minerals, as one ages. Since energy needs decrease, while some vitamin and mineral needs increase, the challenge of maintaining optimal intake for older adults is vital. According to the DRI recommendations, older adults need more calcium, vitamin D, and vitamin B6 as they age. For example, 1200 mg/day of calcium for women older than 50 years and men older than 70 is essential to protect against decreased absorption of calcium and bone loss. Similarly, the DRI indicates that vitamin D needs increase from 600 IU for individuals aged 19 to 70 to 800 IU for those older than age 70. Hypovitaminosis D is currently a significant problem among older adults. An age-related decline in vitamin D intake is correlated with lower dietary intakes, usually due to limited consumption of milk, which is fortified with vitamin D. Decreased vitamin D intake in older adults is also related to less sun exposure, less efficient skin synthesis of vitamin D, and impaired kidney function, which in turn impairs the conversion of vitamin D from its inactive to active form, thus causing deficiency. Insufficient levels of vitamin B6, in addition to folate and vitamin B12, are known to contribute higher than normal levels of serum homocysteine, a known risk factor in the development of coronary artery disease, stroke, and depression, as well as a decrease in cognitive function. Individuals older than 50 years need to consume more vitamin B6 to reduce homocysteine levels and optimize cognitive functioning.42 Also, older adults may need to rely on supplements to avoid the malabsorption of food-bound B12, since as many as 30% of older adults are deficient in vitamin B12 daily. Water is often overlooked as an essential nutrient, and inadequate hydration poses an additional risk for increased morbidity and mortality in older adults. Age-related decline in intracellular water and fluid reserves, paired with changes in renal function (causing an inability to concentrate urine), can result in difficulty maintaining appropriate fluid levels in older adults. Not only do these physiologic factors impair fluid levels, but altered thirst perception, cognitive impairment, and changes in functional status (such as restricted mobility) can result in reduced fluid intake.43 External factors, such as adverse effects of medication use, may also contribute to more impediments to balanced fluid intakes. Residents of long-term care facilities are especially at risk for dehydration because of their limited access to oral fluids or underlying conditions (vomiting, diarrhea, colostomy/ileostomy) that increase fluid losses. Institutional issues, including inadequate staffing and a subsequent need for better supervision, places frail older adults at greater risk.44 Untreated dehydration in hospitalized older adults can result in a mortality rate exceeding 50%.45 As a result, specific triggers are used by staff at long-term care facilities to detect inadequate hydration (Table 79-2). As such, older adults should make a conscious effort to increase fluid intake and not just rely on thirst perceptions. The adequate intake of fluid is the same for older and younger adults.46 A water intake of 1 mL/calorie ingested or 30 mL/kg/day with a minimum of 1500 mL/day is generally recommended to meet dietary water requirements and achieve adequate fluid intake in older adults.47,48
Nutrition and Aging
Introduction
Nutrition Screening and Assessment
Nutritional Requirements
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nutrition and Aging
79