Malnutrition or evidence of cachexia present at diagnosis
Highly emetogenic chemotherapeutic regimens
Treatment regimens associated with severe GI complications such as constipation, diarrhea, loss of appetite, mucositis, enterocolitis (i.e., treatment of sarcomas, non-Hodgkin lymphoma, brain tumors)
Relapsed disease
Age <2 months
Radiation to the head and neck or abdomen
Postsurgical complications such as prolonged ileus or short gut syndrome
HSCT
Low socioeconomic status
The importance of adequate nutritional status is best exemplified by recent studies documenting the effect of poor nutrition on therapy-related toxicities, survival and adherence to medical care. Recent studies performed in homogenous patient populations with fairly large sample sizes have addressed some of the weaknesses of earlier studies. Although most of the studies were retrospective reviews, significant relationships between nutritional status, toxicity and outcome have been reported. In one of the first studies conducted in 768 children with acute myeloid leukemia (AML), body mass index (BMI) percentile at diagnosis was associated with reduced survival (Lange et al. 2005). After controlling for age, race, leukocyte count, cytogenetics and stem cell transplantation, underweight patients had a trend toward decreased survival (HR 1.85, 95 % CI 1.19–2.87, p = 0.06) and were more likely to experience treatment-related mortality (HR 2.66, 95 % CI 1.38–5.11, p = 0.03) while overweight patients were less likely to survive (HR 1.88, 95 % CI 1.25–2.83, p = 0.02) and also had increased treatment-related mortality (HR 3.49, 95 % CI 1.99–6.10, p < 0.001) (Lange et al. 2005). In another large study of 498 pediatric osteosarcoma patients, Hingorani et al. (2011) reported an association between low BMI at the start of treatment with increased postoperative wound infection as well as significant increased risk of arterial thrombosis in children with overnutrition. A retrospective review conducted among 4,260 children with acute lymphoblastic leukemia (ALL) found a hazard ratio of 1.29 (95 % CI 1.02–1.56, p = .04) for relapse in those with obesity, most prominent in the preteenage and adolescent years (Butturini et al. 2007). More recently, a retrospective study exploring the effect of nutritional status at diagnosis and throughout therapy in children with high-risk ALL found that those who remained malnourished for the majority of treatment experienced increased toxicity and reduced survival (Orgel et al. 2014). Remediation of malnutrition reduced the risk of toxicity and improved survival; similar observations have been reported in children residing in Central America (Antillon et al. 2013; Orgel et al. 2014).
Taken together, these studies consistently emphasize the importance of timely and effective nutritional interventions both for those underweight and overweight. Effective nutrition intervention appears to minimize the effects of malnutrition on therapy-related toxicity and survival. Increased attention is needed in regards to the nutritional evaluation and in management of pediatric oncology patients to scientifically evaluate nutritional interventions and monitor for improved outcomes. Here we review the evidence basis for effective measurement and management of nutritional complications and provide graded recommendations (Table 12.2).
Table 12.2
Graded evidence-based recommendations for nutritional intervention in pediatric oncology patientsa
Clinical scenario | Recommendations | Level of evidenceb |
|---|---|---|
Undernutrition | Dietary counseling | 1C |
Nutritionally fortified drinks (see Table 12.4) | 1C | |
Medium-chain triglyceride oil | 1C | |
Appetite stimulants | 2C | |
Enteral tube feeding | 1A | |
Parenteral nutrition avoided when possible | 1A | |
Severe immunosuppression | Data are lacking to recommend neutropenic or low microbial diets | 2C |
Overnutrition | Dietary and lifestyle counseling | 1C |
12.2 Nutrition Assessment
Guidelines for the assessment and categorization of nutritional status, and criteria for intervention, are available to instruct the provision of nutrition therapy. Nutrition assessment should commence at diagnosis and be carried out during treatment as well as into survivorship. As in most aspects of clinical medicine, the importance of history and physical assessment cannot be underestimated. Baseline evaluation should include dietary history to ascertain the extent of caloric protein intake as well as known food aversions, allergies and intolerance. Clinical evaluation includes appropriate anthropometric and biochemical measurements (Table 12.3).
Table 12.3
Components of the nutritional assessment
Basic anthropometrics | Advanced anthropometrics | Biochemical indices |
|---|---|---|
Weight | Body composition assessment | Albumin |
Height/length | Isotope dilution methods | Prealbumin |
Head circumference (<3 years of age) | Bioelectric methods | Glucose |
Weight for height/length | Absorptiometry methods (DPA and DEXA) | Lipid panel |
BMI | Renal panel | |
Height and weight Z score | C-reactive protein | |
Triceps skinfold | Vitamin and trace elements | |
Arm circumference | ||
Waist circumference |
Practically, weight is the measurement most frequently ascertained and followed. Assessments based on weight alone can be misleading, especially in the acutely ill patient when fluid balance may be disturbed, particularly by the presence of edema or mass disease. Additionally, weight may be maintained but lean body mass can be diminished. This situation may arise in the patient who is obese at the onset of treatment. BMI (calculated as weight [kg]/height squared [m2]) is recommended for monitoring growth in children and adolescents and has to be interpreted relative to population reference data due to changes with age and differences between genders. BMI is considered a better proxy for body fat and lean body mass compared to weight alone; however, it is not without limitations, such as in those with increased muscle mass (Mosby et al. 2009). For children <2 years of age, ideal body weight (IBW) should be monitored. Mid-upper-arm circumference and triceps skinfolds provide the best estimate of lean body mass and adipose tissue and should preferably be undertaken by the same trained observer due to interobserver variability (Barr et al. 2011).
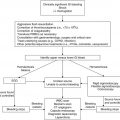
Repeat nutrition assessment during therapy is required to detect changes in nutritional status due to treatment or complications of treatment which may necessitate nutritional interventions. Assessment of hospitalized patients is usually undertaken by the dietician or nutritionist and occurs as per institutional guidelines and ideally during each admission, especially in those at high risk for nutritional depletion (Table 12.1). The use of nutrition software to calculate protein and calories may be beneficial to the clinician. For outpatients, the maintenance of a nutritional diary of variety and quantity of foods and supplements taken is a valuable aid for the dietician to ascertain if the patient is nutritionally replete. Several methods of gathering data can be utilized; 24-h dietary recall conducted on nonsequential days or a 3–5-day food record is most optimal for dietary consultation.
Biochemical assessments need to be interpreted carefully as some proteins can also be acute-phase reactants and give spurious values. Any condition that can alter rate of protein synthesis, degradation, or excretion may alter serum protein concentration. Albumin and prealbumin are most frequently used as nutrition assessment tools, the latter of which is a better indicator of the acute state due to its shorter half-life. Biochemical laboratory assessment should include liver function, renal function, lipid panel and glucose to determine if dietary modification is required; the clinician must be cognizant that values may be altered due to cancer therapy or concurrent infection. For example, L-asparaginase inhibits liver protein synthesis and a very low-fat diet (i.e., <10 g fat/day) is often required due to asparaginase side effects. Similarly, glucose levels must be followed in patients receiving high-dose steroids such as ALL induction. Dietary intervention helps in maintaining adequate nutrition so that chemotherapy can continue at the appropriate dose and schedule and to mitigate potential side effects.
During cytotoxic therapy and with episodes of sepsis, the pediatric cancer patient undergoes a catabolic state with nutrient depletion. Decreased intake of micronutrients has been reported following chemotherapy and may be associated with therapy-related toxicity (Ladas et al. 2004). For example, reduced intake of B vitamins may be associated with the development of neuropathy; zinc, important in both immune function and mucosal integrity, has been associated with increased infection and dysgeusia (altered taste); reduced antioxidant nutrients may be associated with infection and increased hospital stay; and reduced intake of vitamin D and calcium may increase bone morbidity in children with ALL (Henkin et al. 1976; Mahajan et al. 1980; Bolze et al. 1982; Watson et al. 1983; Kennedy et al. 2004; Ozyurek et al. 2007; Youssef et al. 2008; Tylavsky et al. 2010). Thus, a thorough analysis of dietary intake should accompany anthropometric and biochemical assessments.
12.3 Nutrition Intervention
The primary goal of nutritional therapy in the pediatric oncology population is to sustain and promote normal growth and development while the patient is receiving the necessary anticancer treatments. Nutrition interventions should be proactive to prevent the development of malnutrition. If malnutrition develops, nutrition interventions should be implemented to reverse malnutrition and, secondarily, to prevent future protein-energy malnutrition. The most appropriate interventions must meet the nutritional needs of the child but be associated with the least risk. Nutrition counseling and education should be provided to the family with awareness of cultural differences in nutritional practice. The utilization of a dietitian or nutritionist to provide and support the education of healthcare staff, patient families, and patients is a crucial component of optimal nutrition care in pediatric oncology (Sacks et al. 2004). Nutritional intervention should be implemented in the following situations: (1) patients who present underweight (i.e., BMI <5th %ile or <70 % IBW); (2) patients who present overweight (i.e., BMI >95th %ile or IBW >120 %); (3) patients not meeting >80 % of their caloric requirements through oral intake during treatment; and (4) >5 % weight loss from baseline body weight.
12.3.1 Dietary Counseling
Nutrition counseling should begin with strategies to enhance dietary consumption, such as through the utilization of nutrient dense foods. Oral intake may be difficult for many children and adolescents undergoing treatment due to treatment-related toxicities such as severe nausea, vomiting, stomatitis, constipation, and diarrhea but should be offered as an initial strategy before advancing to enteral or parenteral nutrition. Nutritionally fortified drinks should be recommended for patients unable to consume food. Pediatric formulations such as Boost®, PediaSure®, and Ensure® can augment oral intake, and other formulations may be provided to ensure adequate electrolyte balance (Table 12.4). Medium-chain triglyceride (MCT) oil may complement feeding strategies by increasing total calories in a readily absorbable formulation.
Table 12.4
Commonly used nutritional supplements
Oral | High-calorie oral | Enteral |
|---|---|---|
Boost® | Boost® Plus | PediaSure® with/without fiber |
Carnation® Instant Breakfast | Ensure® Plus | Jevity® |
Compleat® Pediatric | PediaSure® 1.5 | Nutren® 1.5/2.0 |
Ensure® | Resource® 2.0 | Osmolite® |
PediaSure® with/without fiber | Peptamen® | |
Nutren Junior® with/without fiber |
Special diets, such as the neutropenic diet or low microbial diet, have been suggested for severely immunosuppressed patients such as those treated with hematopoietic stem cell transplant (HSCT) to minimize the introduction of pathogenic organisms into the gastrointestinal (GI) tract (Moody et al. 2002). Adherence to these diets is difficult and provides further restraints on dietary intake. Clinical trials performed in adults and children with cancer have found that the neutropenic diet is not associated with reduced risk of infection and does not offer an added benefit over food safety guidelines alone (Moody et al. 2006; Gardner et al. 2008). Current standards of practice should consider the lack of evidence supporting a neutropenic diet as an augmentation to food safety guidelines (Table 12.5) prior to recommending it to patients at risk for severe immunosuppression.
Table 12.5
Food safety practicesa
Food shopping |
1. Check expiration dates on food and do not buy or use if the food is out of date. |
2. Do not purchase ready-to-eat food from bulk food bins (i.e., breads, nuts, dried fruit, candies). |
3. Avoid all food in cans that are swollen, dented or damaged. |
4. Avoid produce that is bruised or damaged. |
5. Bag fresh fruits and vegetables separately from meat, poultry and seafood products. |
Food storage |
1. Store perishable fresh fruits and vegetables (i.e. cucumbers, tomatoes) in a clean refrigerator at a temperature of 40 °F or below. |
2. Refrigerate all produce that is purchased pre-cut or peeled. |
3. Beef should be refrigerated at 40 °F and used within two days. Beef can be frozen at 0 °F and used within 6 months of the purchase date. |
Food preparation |
1. Wash hands with water and soap for 20 s before and after any food preparation. |
2. Wash fruits or vegetables under running water even if you are going to peel them. Do not use soap, bleach or commercial produce washes to clean fruit. |
3. Dry produce with a clean cloth towel or paper towel. This will reduce the spread of bacteria. Do not wash meat, poultry or eggs. |
4. Defrost all meats in the refrigerator. Do not defrost at room temperature. |
5. Food-preparation surfaces must be cleaned first. Wash surfaces thoroughly with soap and water and thoroughly dry. As an extra precaution, you can use a solution of one tablespoon unscented, liquid chlorine bleach in one gallon of water to sanitize washed surfaces and utensils. |
6. Wash cutting boards, dishes, utensils and counter tops with hot, soapy water after preparing each food item and before you go on to the next item. |
Cooking |
1. Cook foods immediately after thawing. |
2. All raw foods such as meats, poultry and entrees should be cooked until they are well-done. Beef should be cooked to 160 °F, depending on the cut. Chicken should be cooked to an internal temperature of 165 °F. Cold foods should be stored <40 °F, hot foods kept >140 °F. A home thermometer may help. |
Storage of cooked foods |
1. Store leftovers within 2 h. By dividing leftovers into several clean, shallow containers, you’ll allow them to chill faster. Discard leftovers that were kept at room temperature for greater than 2 h. |
2. Perishable foods (fruits, vegetables, meat, dairy) should be put into the fridge or freezer within 2 h. In the summer months, cut this time down to 1 h. |
3. Do not use leftovers prior to reheating to >165 °F before serving. |
Baby food/infant formula |
1. Never put baby food in the refrigerator if the baby doesn’t finish it. Do not feed your baby directly from the jar of baby food. Instead, put a small serving of food on a clean dish and refrigerate the remaining food in the jar. If the baby needs more food, use a clean spoon to serve another portion. Throw away any food in the dish that’s not eaten. If you do feed a baby from a jar, always discard any remaining food. |
2. Prepare safe water for preparing formula. Bring tap water to a roiling boil and boil it for 1 min. If you use bottled water, follow this same process. Cool the water to body temperature before mixing formula. |
3. Sterilize bottles and nipples before first use. After that, wash them by hand or in a dishwasher. |
4. Formula can become contaminated during preparation, and bacteria can multiply quickly if formula is improperly stored. Prepare formula in smaller quantities on an as-needed basis to greatly reduce the possibility of contamination. Always follow the label instructions for mixing formula. |