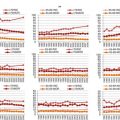
Signs and symptoms
Nursing management
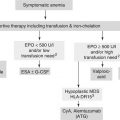
Anaemia
Palpitations
Red blood cell transfusions
Chest pain
Administration of erythropoietin agents
Fatigue
Dyspnea
Dizziness
Headaches
Neutropenia
Fever
Timely recognition of infection
Cough
Administration of recombinant granulocytic growth factors
Dysuria
Antimicrobial therapy (prophylactic or for active infections)
Recurrent/refractory infections
Withhold therapy or dose adjustment
Thrombocytopenia
Petechiae
Timely recognition of risk of bleeding
Ecchymosis
Platelet transfusion
Epistaxis
Aminocaproic acid (prophylactic or for active bleeding)
Hemoptysis
Monitoring medication with anti-platelet effect
Hematuria
Withhold therapy or dose adjustment
Stomatitis and mucositis
Painful mouth sores
Prevent secondary infection
Difficulty chewing/swallowing
Provide pain relief
Reduction of food intake
Maintain dietary intake
Malnutrition
Motivate routine systematic oral care
Negative impact on QoL
In case of fungal infection topical or systemic antifungal agents
Nausea and vomiting
Lack of food/fluid intake
Anti-emetics
Malnutrition
Encourage adequate hydration
Negative impact on QoL
Check intake, weight,
Ensure baseline and ongoing renal function
Diarrhoea
Mucositis
Evaluate for infectious aetiology
Infection
Minimise the complication of dehydration by
Faecal impaction
Encourage adequate hydration
Anti-diarrheals
Dietary consultation
Constipation
Altered bowel elimination
Laxatives
Nausea
Include foods that have a high fibre content
Vomiting
Adequate fluid intake
Abdominal pain
Light exercises
Malaise
Prevent
Decreased mobility
Decreased oral intake
Use of antiemetics/narcotics
Fatigue
Exhaustion
Rehabilitation should begin with the cancer diagnosis but depends on extent of disease
Decreased capacity for mental or physical work
Establish a baseline
Rarely an isolated symptom
Seek information about related factors and offer interventions if possible
Recent illnesses
Pain
Emotional stress
Medication regimen
Anaemia
Sleep disorders
Altered nutritional status
Malnutrition
Anorexia
Encourage adequate hydration
Weight loss
Dietary measures/consultation
Altered and/or loss of taste
Antiemetics
Reluctance
Stomatitis
Gastrointestinal toxicity
To be able to adequately address QoL issues numerous validated QoL questionnaires for cancer patients exist. Older patients can have also other Health Related Quality of Life (HRQOL) concerns than their younger counterparts. Weelwrigt et al. [6] identified 14 specific issues that affect perceived HRQOL in patients older than 70 years with a solid tumor [6]. These 14 items have been grouped into the following conceptually related five scales (mobility, worries about others, futureworries, maintaining purpose and illness burden) and two single items (joint stiffness and family support), and resulted in the EORTC-QLQ-ELD 14 [6].
Nursing Role
To increase patient’s compliance and decrease his/her anxiety, the oncology nurse should discuss all relevant information with the patient and relatives before therapy starts. This information should be delivered in an easily understand way
Nursing care should also be centred during and after treatment to assist their patients to maintain their QoL.
To give information on how the chemotherapy affects the disease as well as QoL, and for how long this can be expected before recovery
Written information on the treatment and the possible adverse events should always be given
The importance of when to alert the treating physician must be emphasised so that the ongoing treatment can be reassessed as soon as possible
To adequately address all HRQOL issues which are important to older patients
To limit the severity of adverse events, their early identification and prompt intervention are needed for the most common ones
To carefully evaluate psychological problems
Case Presentation (Continued)
Mr. A calls the hotline from the hospital. He cannot eat very well. He is feeling nauseous and it feels as if he has a full stomach. When the nurse asks about his bowel elimination, it appears that Mr. A has been constipated since three days. During the nurse’s assessment she also asks Mr. A how his fluid intake, diet and physical activity have been. Mr. A admits he has not been out of his chair since the last visit to the hospital. Mr. A is given a prescription for a laxative and the nurse encourages him to walk around more.
She makes a note in the electronic patient’s file and also lists him for a recall phone call in a couple of days for reassessment’s.
Patient Preferences and Information Needs
Older persons grew up in a culture where decision making was more paternalistic. This may either lead to a lower information need or to a risk for poor communication. Research indicates that patient preferences and information needs differ widely. Patient information should target older patients’ needs, in order to prepare them to the prescribed treatment and to help them deal with adverse effects [7].
The majority of older adults must also cope with growing limitations in the physical and cognitive functioning along with age progresses. However cognitive decline due to aging, may limit the understanding and memorization of complex information; this might imply that the need for further information may be inhibited [8]. As a result of this, patients may feel distressed due to the difficulties in understanding what is happening along their clinical course. In the communication with family and friends, stress can also worsen when patients become incapable of understanding the consequences of their decisions [9].
Older patients have unmet communication needs as serious gaps in recalling and understanding may occur during psychological and physical health crisis [9]. A possible explanation for this is that older adults have unique language, cognitive, psychological, and social issues that affect their own health ability to read and write [10]. Unfulfilled information needs may cause non-compliance, and this is an important risk factor for the outcome of the medical treatment.
Patient’s coping strategies have been described as influencing their information needs [11]. Each single individual will differ in his/her coping styles (and information needs): this can influence the patient’s requests and behaviour. According to Miller et al. [12], individuals can use two main cognitive coping styles in dealing with cancer and other health threats: monitoring (attending to) or blunting (avoiding) potentially threatening information. Individuals may use either coping style at different moments [12]. Patients fare better (psychologically, behaviourally, and physiologically) when the information they receive about their medical condition is tailored to their own coping style: generally those with a monitoring style tend to do better when given more information, and those with a blunting style do better with less information. To explicitly judge patients in advance on their preferences, the following questions may be helpful: ‘Do you generally think ‘I want to know every detail’ or do you tend to say ‘I’ll will just see what is going to happen’? [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree