Gastroesophageal cancer (GEC) remains a major cause of cancer-related mortality worldwide. Although the incidence of distal gastric adenocarcinoma (GC) is declining in the United States, proximal esophagogastric junction adenocarcinoma (EGJ) is increasing in incidence. GEC, including GC and EGJ, is treated uniformly in the metastatic setting. Overall survival in the metastatic setting remains poor. Molecular characterization of GEC has identified mutations and copy number variations, along with other oncogenes, biomarkers, and immuno-oncologic checkpoints that may serve as actionable therapeutic targets. This article reviews these key aberrations, their impact on protein expression, therapeutic implications, and clinical directions within each pathway.
Key points
- •
Anti-human epidermal growth factor receptor 2 (HER2) trastuzumab therapy is standard for HER2 amplified/overexpressed gastroesophageal adenocarcinoma, whereas second/later lines of anti-HER2–directed therapy have not shown definitive benefit to date.
- •
Anti–vascular endothelial growth factor receptor 2 (VEGFR2) ramucirumab modestly improves survival as monotherapy and in combination with paclitaxel in second-line treatment of patients with gastroesophageal adenocarcinoma.
- •
Anti–epidermal growth factor receptor (EFGR) therapy has not shown benefit in unselected gastroesophageal patients in any line of therapy, although gene amplification/overexpression warrants further investigation.
- •
Anti-MET therapy has not shown benefit in overexpressing gastroesophageal patients in any line of therapy, although gene amplification/overexpression may merit further investigation.
- •
Other promising predictive biomarkers and targeted therapies, including fibroblast growth factor type 2 and claudin 18.2, require further investigation in larger trials to confirm therapeutic benefits for patients with gastroesophageal adenocarcinoma.
Background
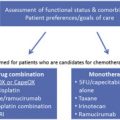
Distal gastric adenocarcinoma (GC) incidence ranks fifth globally and third for cancer-related mortality of all malignancies. Approximately 25,000 new GC cases and 11,000 deaths occurred in the United States in 2015. In contrast, esophagogastric junction adenocarcinoma (EGJ), is increasing in incidence. For both (gastroesophageal cancer [GEC]), most patients present with metastatic disease, or locally advanced disease with a high risk of recurrence despite aggressive perioperative therapy. In the metastatic setting, median overall survival (OS) remains approximately 11 months with optimal palliative chemotherapy in ERRB2 -nonamplified patients. Over the past decade, molecular subtyping of GEC has highlighted the interpatient heterogeneity of GEC and uncovered potentially actionable molecular pathways. Routine next-generation sequencing identified that at least 37% of patients with GC harbor genetic alterations in receptor tyrosine kinases (RTKs), including ERBB2 , MET , EGFR , KRAS , and FGFR2 . These genomic events, as well as recently derived key subsets of the disease, namely microsatellite instability-high (MSI-high), Epstein-Barr virus (EBV) associated, chromosomal instability (CIN), and genomically stable (GS), provide more molecularly targeted therapeutic possibilities.
Erb-B2 Receptor Tyrosine Kinase 2
Erb-B2 receptor tyrosine kinase 2 (Erb-B2), or HER2, is a transmembrane RTK within the epidermal growth factor receptor (EGFR) family, encoded at chromosome 17q21. HER2 regulates proliferation, adhesion, differentiation, and migration via activation of the Ras and Mitogen-activated protein kinases (RAS-MAPK) and phosphatidylinositol-3-kinase and AKT (PI3K-AKT) pathways. HER2 lacks an exogenous ligand and is transactivated via heterodimerization with other HER family members, leading to downstream kinase activation. Significant and therapeutically relevant overexpression results predominantly from gene amplification. HER2 IHC expression localizes to the cell membrane in well-differentiated adenocarcinoma and to the cytoplasm in poorly differentiated adenocarcinomas, which may affect treatment response. HER2-expressing tumors are more common with EGJ (15%–20%) compared with distal GC (10%–15%), and the prognostic impact of HER2 expression remains controversial.
Effective targeting of HER2 in GEC was initially shown using trastuzumab, a humanized monoclonal anti-HER2 antibody against the HER2 ectodomain ( Table 1 ). The phase III ToGA trial evaluated first-line fluoropyrimidine/cisplatin chemotherapy doublet with or without trastuzumab in patients with HER-2 over-expressing (any IHC 3+ or fluorescence in-situ hybridization [FISH] HER2/CEP17 ratio ≥2) unresectable or metastatic GEC. Patients receiving trastuzumab survived a median of 13.8 months versus 11.1 months with chemotherapy alone, and response rates were 47% and 35% respectively in the intention-to-treat (ITT) population. In a subset analysis, median survival was 16 versus 11.8 months in the combined IHC2+/FISH+ and IHC3+ groups, accounting for 77% of the patients. This trial therefore led to the approval of trastuzumab in HER2 overexpressing GEC for the IHC2+/FISH+ and IHC3+ subsets of the trial.
| Line | Trial | N | Treatment | Primary End Point (Met?) | mOS (mo) | HR | mPFS (mo) | HR | RR (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1L | Bang et al, 2010 ToGA | 584 | Cis/FP + placebo Cis/FP + trastuzumab | OS (Yes) | 11.1 | 0.74 | 5.5 | 0.71 | 35 |
| 13.8 | P <.0046 | 6.7 | P <.001 | 47 | |||||
| 1L | Hecht et al, 2016 LOGiC | 545 (487) | Cis/FP + placebo Cis/FP + lapatinib | OS (No) | 10.5 | 0.91 | 5.4 | 0.82 | 39 |
| 12.2 | P = NS | 6 | P = .03 | 53 | |||||
| 2L | Satoh et al, 2014 TyTAN | 261 | Paclitaxel + placebo Paclitaxel + lapatinib | OS (No) | 8.9 | 0.84 | 4.4 | 0.84 | 9 |
| 11 | P = NS | 5.5 | P <.001 | 27 | |||||
| 2L | Kang et al, 2016 GATSBY | 345 (1:2) | Paclitaxel (38%)/Doc (62%) T-DM1 | OS (No) | 8.6 | 1.15 | 2.9 | 1.13 | 20 |
| 7.9 | P = NS | 2.7 | P = NS | 21 |
Although HER-2 overexpression/ ERBB2 amplification predicts benefit from the anti-HER2 antibody trastuzumab in the first-line setting, the definition of positivity and trial inclusion criteria within trials has evolved over time. Current clinical diagnostic testing requires evaluation by a combination of IHC (membranous reactivity in ≥10% of cancer cells in a surgical specimen or a cluster of at least 5 cells in a biopsy specimen), and FISH (with HER2/CEP17 ratio ≥2). IHC 0/1 is considered negative, and IHC3+ is considered positive, whereas IHC2+ requires reflex FISH assessment. Higher throughput assays, including mass spectrometry and next-generation sequencing, have emerged with potential to refine diagnostic accuracy as well as possessing multiplexing capability to assess for other relevant aberrations. Assessment of ERBB2 amplification by cell-free DNA is also emerging as a potential noninvasive strategy for serial assessment of HER2 status that can monitor intrapatient tumoral evolution.
Lapatinib, a selective intracellular tyrosine kinase inhibitor (TKI) of ErbB1 and ErbB2, was also studied in first-line and second-line GEC (see Table 1 ). The phase III TRIO-013/LOGiC trial randomized 545 untreated patients with HER2-positive (HER2/CEP17 ratio ≥2 by FISH or IHC 3+ if FISH not available) GEC to receive capecitabine and oxaliplatin in addition to either lapatinib or placebo. Lapatinib increased objective response from 39% to 53%, and modestly increased median progression-free survival (PFS) from 5.4 to 6 months, but failed to confer an OS benefit in the ITT population. Younger and Asian patients seemed to derive the most benefit in subset analyses. The absolute level of amplification positively correlated with outcome, as previously described, signifying heterogeneity of benefit within the current HER2-positive classification. Recently, the degree of amplification has been shown to correlate closely with absolute protein expression level, which is associated with clinical benefit. Inter-trial variation in absolute amplification/expression as well as lack of antibody-dependent cell-mediated cytotoxicity (ADCC) with lapatinib compared with trastuzumab, serve as two of the many potential explanations when contrasting outcomes of ToGA and LOGiC. In the second line, the phase III Asian TyTAN trial enrolled patients with GEC regardless of HER2 expression (FISH ratios ≥2 were eligible), and 31% of patients enrolled were FISH+ and IHC 0/1+. Patients received paclitaxel alone or in combination with lapatinib. Despite response rates of 27% versus 9%, no significant PFS or OS benefit was shown in the ITT population. Of note, when evaluating only those patients with 3+ HER2 expression by IHC, median survival improved from 7.6 to 14 months in this subgroup ( P = .0176), and PFS 4.2 to 5.6 months ( P = .0101). This finding highlights the need to improve patient selection for targeted therapies.
Trastuzumab emtansine (T-DM1), an antibody-drug conjugate that is approved in HER2-positive metastatic breast cancer, was studied in the second-line GATSBY trial (see Table 1 ), but failed to demonstrate a response or survival benefit versus paclitaxel monotherapy. Possible explanations for this negative trial include intrapatient tumor heterogeneity, recognized to be more frequent in GEC than observed in breast cancer, with HER2-negative clones not controlled by targeted cytotoxic therapy. Another possible explanation is the recent appreciation of conversion of HER2 status after first-line therapy, making archived samples, as used in GATSBY (and TyTAN), inadequate for selecting appropriate HER2+ patients in the second line.
In addition, although trastuzumab binds domain IV of HER2, pertuzumab binds domain II and thereby prevents dimerization. The CLEOPATRA trial revealed PFS and OS benefits with the addition of pertuzumab to trastuzumab and chemotherapy in breast cancer, and initial results from the JACOB trial evaluating pertuzumab in combination with trastuzumab and chemotherapy are eagerly awaited.
Thus, to date, no standard anti-HER2–directed approaches are recognized in trastuzumab-refractory HER2+ GEC. However, standard chemotherapy with irinotecan-based or taxane-based regimens are recommended. Notably, although second-line ramucirumab trials, discussed later, included HER2-positive and trastuzumab-treated patients, this accounted for only ∼6% of patients enrolled in RAINBOW and less than 1% of REGARD. Other strategies under evaluation in the second and later lines include novel TKIs like apatinib, trastuzumab beyond progression, novel HER2 antibodies, and combination therapy with immune checkpoint inhibitors (see Table 5 ).
Vascular Endothelial Growth Factor
Vascular endothelial growth factor (VEGF) induces angiogenesis and neovascularization. Overexpression is found in up to 58% of patients with resected gastric cancer , and 7% of The Cancer Genome Atlas (TCGA) patients with gastric cancer have VEGF-A gene amplification. Ramucirumab, a human immunoglobulin G1 (IgG1) monoclonal antibody that directly binds to VEGFR2 and inhibits VEGF ligand binding, was evaluated in the second-line setting in the phase III REGARD trial ( Table 2 ). Compared with supportive care, ramucirumab demonstrated an OS of 5.2 versus 3.8 months ( P = .047), despite a response rate of only 3% (the same as the placebo control). The phase III RAINBOW trial subsequently compared paclitaxel with or without ramucirumab in the second-line setting (see Table 2 ). Patients had a significant OS benefit of 9.6 versus 7.4 months ( P = .017) as well as statistically significant PFS and objective response rate (ORR) benefits. In the third-line setting, apatinib, a multi-TKI, including VEGF receptor (VEGFR) kinases, showed an absolute 0.8-month PFS advantage (2.6 vs 1.8 months) as well as a nearly 2-month OS benefit compared with placebo in a Chinese population.
| Line | Trial | N | Treatment | Primary End Point (Met?) | mOS (mo) | HR | mPFS (mo) | HR | RR (%) |
|---|---|---|---|---|---|---|---|---|---|
| 2L | Fuchs et al, 2014 REGARD | 335 | Placebo Ram | OS | 3.5 | 0.78 | 1.3 | 0.48 | 3 |
| 5.2 | P = .047 | 2.1 | 3 | ||||||
| 2L | Wilke et al, 2014 RAINBOW | 665 | Paclitaxel + placebo Paclitaxel + Ram | OS | 7.4 | 0.8 | 2.9 | 0.64 | 16 |
| 9.6 | P = .017 | 4.4 | 27 | ||||||
| 3L | Li et al, 2016 | 267 | Placebo Apatinib | OS/PFS | 4.7 | 0.71 | 1.8 | 0.44 | 0 |
| 6.5 | P = .015 | 2.6 | 3 | ||||||
| 1L | Ohtsu et al, 2011 AVAGAST | 774 | Cis/5FU + placebo Cis/5FU + Bev | OS (No) | 10.1 | 0.87 | 5.3 | 0.8 | 37.4 |
| 12.1 | NS | 6.7 | P = .004 | 46 | |||||
| 1L | Shen et al, 2015 AVATAR | 202 | Cis/Cape + placebo Cis/Cape + Bev | OS (No) | 11.4 | 1.11 | 6 | 0.89 | 34 |
| 10.5 | NS | 6.3 | NS | 41 | |||||
| 1L | Yoon et al, 2014 | 168 | FOLFOX + placebo FOLFOX + Ram | PFS (No) | 11.7 | 1.08 | 6.7 | 0.98 | 46 |
| 11.5 | NS | 6.4 | NS | 45 | |||||
| 1L | Enzinger et al, 2016 | 64 | FOLFOX + placebo FOLFOX + aflibercept | 6m PFS (No) | 18.7 | 0.7 | 7.3 | 0.88 | 75 |
| 1:02 | 13.7 | NS | 9.9 | NS | 61 |
However, evaluation of antiangiogenesis in the first-line setting of GEC has been disappointing to date. The AVAGAST trial evaluated chemotherapy (cisplatin and capecitabine) with or without bevacizumab, a humanized IgG1 VEGF-A monoclonal antibody. Despite PFS (6.7 vs 5.3 months; P = .0037) and ORR (46% vs 37.4%; P = .0315) benefits, the improved median OS of 12.1 over 10.1 months observed in the control was not statistically significant. An Asian trial, AVATAR, confirmed these negative findings. A phase II trial of first-line ziv-aflibercept with FOLFOX recently did not meet its primary end point of 6-month PFS compared with FOLFOX alone. In addition, a phase II trial in first-line GEC comparing FOLFOX with or without ramucirumab was negative. Despite this, the phase III RAINFALL trial is currently evaluating first-line ramucirumab/placebo in combination with capecitabine and cisplatin in metastatic GEC, with results eagerly awaited ( NCT02314117 ).
Predictive biomarkers of response to antiangiogenesis, to be incorporated into routine practice, have remained elusive. The AVAGAST trial suggested that patients with high plasma VEGF-A levels had increased OS compared with those expressing low VEGF-A levels, and hypertension as a biomarker has been noted. Further biomarker development may help identify a subset of patients who derive the most benefit from targeting this axis. However, biomarkers of response may remain undefined, potentially because of a marginal benefit realized by most patients.
Epidermal Growth Factor Receptor
EGFR, or Erb-B1 is a transmembrane receptor and a well-recognized mediator of oncogenic phenotype that is overexpressed in approximately 30% of GEC. EGFR-overexpressing tumors are associated with higher stage, more poorly differentiated histology, increased vascular invasion, and potentially shorter survival. EGFR amplification is found in only ∼5% of patients.
EGFR-directed therapies evaluated in GEC include cetuximab and panitumumab, which are monoclonal antibodies that antagonize the extracellular binding domain. Preclinical data also suggested that cetuximab, a recombinant human-murine chimeric monoclonal antibody of a murine Fv region and a human IgG1 heavy and k light chain Fc region, induces ADCC. Small-molecule TKIs, such as gefitinib, erlotinib, lapatinib, and afatinib, competitively bind intracellularly to the tyrosine kinase domain. Early phase II trials combining cetuximab, panitumumab, or erlotinib with cytotoxic chemotherapy in GEC reported first-line therapy response rates ranging from 41% to 65%. Second-line phase II evaluation of gefitinib or erlotinib monotherapy led to more modest responses of ∼9% to 11%, and responses seemed limited to proximal EGJ cancers rather than distal GC.
Subsequent phase III GEC trials targeting EGFR included EXPAND (cetuximab with capecitabine/cisplatin, first line), REAL-3 (panitumumab with epirubicin/oxaliplatin/capecitabine, first line), and COG (gefitinib, second line or higher) ( Table 3 ). Disappointingly, each trial was negative, and panitumumab resulted in worse survival compared with the control. Notably, each of these trials enrolled all-comers without biomarker selection of any kind.
| Line | Trial | N | Treatment | Primary End Point (Met?) | mOS (mo) | HR | mPFS (mo) | HR | RR (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1L | Lordick et al, 2013 EXPAND | 904 | Cis/5FU + placebo Cis/5FU + Cetuximab | PFS (No) | 10.7 | 1.00 | 5.6 | 1.09 | 29 |
| 9.4 | 4.4 | P = .32 | 30 | ||||||
| 1L | Waddell et al, 2013 REAL-3 | 553 | Epi/Oxali/Cape + placebo Epi/Oxali/Cape + P | OS (No) | 11.3 | 1.37 | 7.4 | 1.22 | 42 |
| 8.8 | P = .013 | 6.0 | 46 | ||||||
| 2L | Dutton et al, 2014 COG | 450 | Placebo Gefitinib | OS (No) | 3.67 | 0.9 | 1.17 | 0.8 | ∼1 |
| 3.73 | 1.57 | ∼4 |
Xenograft models evaluating anti-EGFR therapy for EGFR -amplified tumors have reported potential benefit. In the phase II study combining FOLFOX with cetuximab, 22% of patients had greater than 4 EGFR copies, which correlated with increased OS. Similarly, in TRANS-COG, the translational correlative study of COG, 15.6% of patients had increased gene copy number, including true EGFR amplification (∼5%); this latter small subset of EGFR -amplified patients derived a statistically significant survival benefit with the addition of gefitinib (hazard ratio [HR], 0.19; P = .007). The EXPAND trial also showed survival benefit in the small subset with extremely high EGFR expression by IHC H-score (likely representing EGFR-amplified tumors, but yet to be confirmed). With these recent promising subset analyses of EGFR amplification and consequent overexpression, future studies assessing the benefits of anti-EGFR therapy in these patients are being pursued. Also, a phase III trial of second-line nimotuzumab with irinotecan ( NCT01813253 ) is currently recruiting patients deemed to harbor EGFR-overexpressing (IHC 2/3+) tumors (see Table 5 ).
MET
The MET proto-oncogene encodes the c-MET receptor tyrosine kinase, which is involved in cell proliferation, angiogenesis, and migration. MET overexpression, as well as the subset with MET amplification, are each associated with worse survival in most reports. Canonical MET activation occurs via binding of its ligand, hepatocyte growth factor (HGF), but MET activation can also occur in an HGF-independent manner through RTK crosstalk. MET amplification leads to constitutive receptor activation independent of HGF ligand, and is reported in ∼4% to 10% of GEC cases, but overexpression ranges from 23.7% to 70% in GEC, depending on the cohort evaluated and method of analysis used.
As a predictive biomarker, early-phase reports and trials initially suggested that patients with GEC with MET-expressing tumors may benefit from MET-directed therapy. However, a subsequent phase II and two phase III MET-directed trials in GEC have been reported with overall negative results ( Table 4 ). The METGastric study evaluated onartuzumab, a humanized IgG1 antibody against the extracellular domain of c-MET, in combination with mFOLFOX6, in patients with c-MET–expressing tumors (≥1+, ≥50% cells). However, METGastric was terminated prematurely (70% of planned accrual) because of negative results (regardless of intensity of MET expression) in the prior/parallel YO28252 phase II biomarker evaluation trial of onartuzumab in unselected patients with GEC. With this in mind, no benefit was seen in the ITT or in the MET IHC 2/3+ preplanned subgroup analysis of the phase III trial (∼38% of enrolled patients; HR, 0.64; P = .06), which had less power to identify a true benefit because of early termination of the trial. Similarly, RILOMET-1, which evaluated epirubicin, cisplatin, and capecitabine with or without the addition of rilotumumab, a fully human IgG2 antibody against HGF ligand, was terminated because of an increased risk of death from the study drug.
| Line | Trial | N | Treatment | Primary End Point (Met?) | mOS (mo) | HR | mPFS (mo) | HR | RR (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1L | Cunningham, 2015 RILOMET-1 | 609 | Epi/Cis/5FU + placebo Epi/Cis/5FU + Rilo | OS (No) | 11.5 | 1.37 | 5.7 | 1.3 | 39 |
| 9.6 | P = .016 | 5.7 | 30 | ||||||
| 1L | Shah et al, 2016 METGastric | 562 | FOLFOX + placebo FOLFOX + onartuzumab | OS (No) | 11.3 | 0.82 | 6.8 | 0.9 | 41 |
| 11 | P = .24 | 6.7 | 46 |
One pitfall of these phase III trials was their loose definition of MET expression. In RILOMET-1, patient selection was defined as greater than or equal to 1+ MET expression by IHC in greater than or equal to 25% of tumor cells to be eligible, which amounted to 81% of all patients screened, and of all patients enrolled and treated only 21% were in the very high MET expression group of IHC 2/3+ in greater than or equal to 50% of cells. Similarly, only 38% of METGastric patient samples were IHC 2/3+ in greater than or equal to 50% of cells, but, as discussed earlier, these patients showed a near-significant benefit in an underaccrued trial. Even with the large phase III MET inhibitor trials, it could be argued that the selection for MET-dependent cancers was too lenient and inadequate, and the highest expressing tumors under-represented. Another negative trial in second line with the multi-TKI foretinib was observed, again without selecting patients by any biomarker.
More promising results have been reported in smaller trials of MET inhibitors for MET -amplified patients (4%–5% of GEC), with consequent overexpression. AMG-337, a highly selective MET TKI, showed clinical responses in patients with MET -amplified advanced GEC (ORR, 50%), but the phase II study has been on hold after the expansion phase of the trial (results not publicly available). Similarly, half of MET -amplified patients treated with crizotinib in a phase I expansion cohort experienced response, and 75% of MET -amplified patients receiving ABT-700 monoclonal antibody monotherapy showed an objective response. The challenge of molecular heterogeneity, particularly in the CIN subset of GEC, may account for general lack of durable response and rapidly acquired resistance to MET-directed monotherapy for MET -amplified GEC. Any future therapeutic attempts with MET inhibitors are likely to be directed toward the small subset of MET -amplified patients, likely with combination approaches with either chemotherapy, other targeted therapies, or immune checkpoint inhibition to address this complex biology ( Table 5 ).
| Target | Line | Trial | Phase | Treatment | Primary End Point | Outcome |
|---|---|---|---|---|---|---|
| HER2 | 2L HER2+ | NCT02689284 | I/II | Margetuximab + pembrolizumab | MTD/ORR | Ongoing |
| HER2 | 1L | NCT01774786 JACOB | III | TP ± pertuzumab | OS | Ongoing |
| EGFR | 1+, amplified | NCT02213289 PANGEA-IMBBP | I/II | Chemotherapy + ABT-806 | OS | Ongoing |
| MET | 2+L, MET-amplified | NCT02016534 | II | AMG-337 | ORR | Ongoing (HOLD) |
| EGFR | 2, EGFR Exp 2/3+ | NCT01813253 | III | Irinotecan ± nimotuzumab | OS/PFS | Ongoing |
| FGFR2 | 3+L, amplified | NCT01719549 | II | Dovitinib | RR/PFS | Ongoing |
| FGFR2 | 2+L, amplified | NCT01921673 | I/II | Dovitinib + Doc | MTD/PFS | Ongoing |
| FGFR2 | 2L, polysomy/amplified | NCT01457846 SHINE | II | AZD4547 vs paclitaxel | PFS | Negative (amplified mPFS 1.5 vs 2.3 mo) |
| FGFR2 | Any | NCT02318329 | I | FPA144 | MTD/DLT | Ongoing |
| PI3K | 2+L | NCT01576666 | IB | LDE225 + BKM120 | MTD/DLT | Ongoing |
| PI3K | 2-4L, PIK3CA mutated/amplified or HER2+ | NCT01613950 | IB | BYL719 + AUY922 | MTD/DLT | Ongoing |
| Akt | 2L, PIK3CA mutated/amplified | NCT02451956 | II | AZD5363 + paclitaxel | ORR | Ongoing |
| Akt/mTOR | 2L | NCT02449655 | II | Paclitaxel + AZD5363 or AZD2014 | ORR | Ongoing |
| mTOR | 2-3L | NCT00879333 GRANITE-1 | III | Everolimus vs placebo | OS | Negative (5.4 vs 4.3 mo, P = .124) |
| CLDN18.2 | 1L, CLDN18.2 expressing | NCT01630083 FAST | II | EOX ± IMAB362 | PFS | Positive – improved PFS, OS |
Fibroblast Growth Factor Type 2
Fibroblast growth factor type 2 ( FGFR2 ) encodes an RTK that regulates cell angiogenesis and proliferation, and, when highly expressed, portends a poor prognosis in both Western and Asian populations. FGFR2 expression in GEC is primarily driven by gene copy number, with 4% to 10% of GEC patients harboring FGFR2 amplification. FGFR2 amplification has been associated with diffuse-type GC but also CIN EGJ adenocarcinoma. Dovitinib, a TKI targeting FGFR1/2/3, VEGF1/2/3, PDGFR and c-KIT, exhibited activity in vitro. The SHINE trial compared paclitaxel with AZD4547, another FGFR2 TKI, in advanced GC in Asia in previously treated patients, but the paclitaxel arm had superior survival, even in the FGFR2 -amplified patient subset. In contrast, another small phase IIa trial showed response in 3 out of 9 patients (33%) with promising durability in FGFR2 -amplified patients, and also observed that higher and homogeneous gene amplification may better predict therapeutic benefit. These early-phase trials suggest safety from this class of TKIs, with mainly hyperphosphatemia and ocular toxicities reported. Phase II trials are ongoing in combination with cytotoxic therapies, which, similarly to HER2, may be a more promising approach than monotherapy. Recently, 2 out of 6 (33%) patients with FGFR2 overexpressing gastric cancer responded to FPA144, a novel humanized monoclonal IgG1 antibody against the FGFR2b isoform, in a chemotherapy-refractory phase I evaluation. Another 3 out of 6 (50%) had stable disease, resulting in a 5 out of 6 (83%) disease control rate in this early assessment. Phase I expansion accrual remains ongoing in this patient population, with specific interest in patients with FGFR2 -amplified GEC (see Table 5 ). FPA144 does not inhibit FGF23 signaling, which mitigates adverse hyperphosphatemia that has hindered FGF TKI development.
PI3K-AKT-mTOR
The PI3K-AKT-mammalian target of rapamycin (mTOR) pathway is commonly altered in GEC, leading to increased proliferation and apoptotic resistance. PIK3CA activating mutations, loss of PTEN , RICTOR amplification, and AKT amplification have all been described. PIK3CA activating mutation alone is observed in ∼15% of GEC.
Attempted inhibition of mTOR with everolimus showed a median PFS of 2.7 months and OS of 10.1 months in an early study, but the subsequent phase III GRANITE-1 trial comparing everolimus with placebo in an unselected patient population of second-line or third-line therapy failed to show an OS benefit. Results from a phase III trial of paclitaxel with or without everolimus are still awaited ( NCT01248403 ). Numerous PI3K inhibitors have shown benefit in preclinical studies, including BEZ235 and BKM120 as monotherapy, or in combination with HSP90 or hedgehog inhibitors, suggesting a disconnect between preclinical models and GEC patients treated with these agents. Second-line AKT inhibition trials are ongoing with AZD5363 in combination with paclitaxel ( NCT02451956 / NCT02449655 ), as well as the first-line JAGUAR trial combining FOLFOX with or without AKT inhibition using ipatasertib ( NCT01896531 ). Strategies selecting for only those with tumors having a genomically activated PI3K-AKT-mTOR pathway may enrich for clinical benefit to these targeted therapies, but further investigation is required to support this notion (see Table 5 ).
CLDN18.2
Claudins are structural components of tight junctions that seal intercellular space, and are overexpressed in numerous cancers. CLDN18 amplification is found in 3% of TCGA patients with gastric cancer and 3% of patients also harbor oncogenic gene fusions between CLDN18 and ARHGAP26 , a RHOA inhibitor. These fusions impair cell-extracellular membrane adhesion, and in doing so promote migration. Claudiximab (IMAB362) is a chimeric IgG1 monoclonal antibody against CLDN18.2 that is intended to enhance T-cell infiltration and antibody-dependent cell-mediated toxicity (ADCC). Claudiximab was developed from high-throughput screening of malignancy-specific cell surface molecules that identified gastric specificity of claudin 18 splice variant 2. Phase II evaluation of claudiximab in combination with epirubicin/oxaliplatin/capecitabine (FAST trial) demonstrated a 39% ORR along with PFS and OS in patients expressing CLDN18.2 (defined as ≥2+ intensity) in at least 40% of cells. Benefit was more pronounced in patients with overexpression in over 70% of tumor cells (see Table 5 ). Further evaluation is planned in a phase III study.
Programmed-death Ligand 1
Immune checkpoint inhibition using programmed-death 1 (PD-1) and programmed-death ligand 1 (PD-L1) inhibitors are under evaluation in many cancers, including GEC. PD-L1 normally binds to receptors on T lymphocytes, thereby inhibiting T-cell proliferation and inducing apoptosis, which impairs the cytotoxic immune response. EBV-associated GEC overexpresses PD-L1 and PD-L2 because of amplification of 9p24, and MSI-high tumors are also associated with intense immune infiltration and overexpression of checkpoint inhibitor targets. KEYNOTE-012 evaluated pembrolizumab, a PD-1 inhibitor, in PD-L1+ (∼30%–40% of patients screened) advanced GC, and showed a 22% ORR. Of note, although PD-L1 overexpression correlated with a higher response rate, PD-L1 expression remains a poor predictive biomarker; patients without PD-L1 expression can still respond, and most often those with expression do not derive benefit. Similarly, in the CheckMate-032 trial, objective response to nivolumab, another PD-1 inhibitor, was 18% and 12% in PD-L1-positive and PD-L1-negative patients, respectively, in patients with chemorefractory GEC. Second-line response rates, stratified by PD-L1 status, were similar in the Javelin GEC trial with avelumab, a PD-L1 antagonist (18.2% vs 9.1%), and less in subsequent lines (10% vs 3.1%). RNA expression signatures reflecting interferon gamma activity and T-cell activity are are currently under development in order to improve patient selection. Phase III evaluation of pembrolizumab (KEYNOTE-062, KEYNOTE-061) in the first-line and second-line metastatic settings respectively, and nivolumab (CheckMate-577) in the adjuvant setting are ongoing, with various other approaches in all lines of therapy being assessed with multiple PD-1/PD-L1 inhibitors.
Cytotoxic T Lymphocyte Antigen 4
Cytotoxic T lymphocyte antigen 4 (CTLA4) is constitutively expressed on the surface of T-regulatory cells and expression can be inducible on activated T lymphocytes and monocytes. Downregulation leads to interleukin (IL)-2 production and IL-2R expression, with subsequent priming of the T-cell response. Mutations and copy number variation of CTLA4 occur rarely, in only 2.5% of TCGA patients with gastric cancer. Tremelimumab is a fully humanized IgG2 anti-CTLA4 monoclonal antibody that has undergone evaluation in numerous other malignancies. Of the 18 patients with metastatic GC enrolled in a second-line phase II trial, no objective responses were seen after cycle 1. However, 12-month survival was 33%, and 1 patient later derived a partial response after 25.4 months of therapy and was alive at 32.7 months at the time of publication. Ipilimumab, another CTLA-4 antagonist, was evaluated as maintenance therapy after receiving a platinum fluoropyrimidine doublet, but failed to prolong PFS or OS. Evaluation remains underway in combination with PD-1/PD-L1 antagonists as discussed earlier.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree