Normal Physical Growth and Development
Jeremi M. Carswell
Diane E. J. Stafford
KEY WORDS
Adrenarche
Gonadotropins
Growth
Growth hormone
Puberty
Sexual development
Sexual maturity rating
Accelerated growth, maturation of sexual characteristics, and the attainment of adult height and body proportions are the physical hallmarks of adolescence. Underlying these changes are the complicated activation and interplay of several hormonal axes that have been previously quiescent. This chapter provides an overview of the normal pubertal process and highlights the wide variation in the onset and duration of puberty in healthy adolescents and between male and female adolescents. Understanding these variations will provide the health care provider a framework for differentiating normal variations from abnormal pubertal development. The focus of Chapter 11 is abnormalities in growth and pubertal development.
Although there is activity and change in most hormonal systems during adolescence, the three that are primarily responsible for many of the physical changes are the hypothalamic-pituitary-gonadal (HPG) axis, the hypothalamic-pituitary-adrenal (HPA) axis, and the growth hormone (GH) axis.
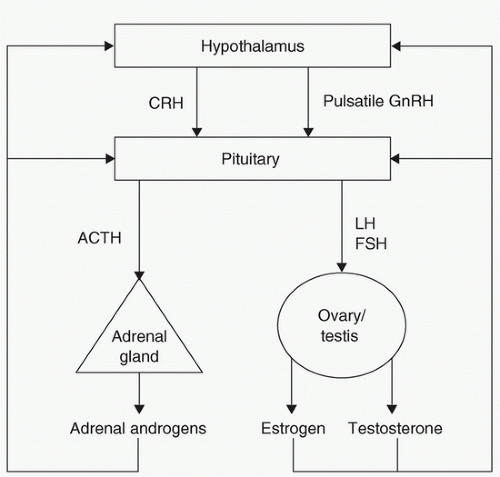
HPG Axis
This axis is ultimately responsible for the release of estradiol and testosterone from the ovaries and testes, respectively, via the pituitary hormones, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). This process originates with the release of gonadotropin-releasing hormone (GnRH) from the hypothalamic pulse generator that then signals release of LH and FSH from the anterior pituitary. The mechanisms by which this system is activated are not completely understood, although it appears that it is released/inhibited by the central nervous system, which in turn enables a positive feedback loop that results in pubertal maturation (Fig. 2.1).
HPA Axis
The products of HPA maturation in the context of puberty are the adrenal androgens, primarily dehydroepiandrosterone (DHEA) and its sulfate ester, dehydroepiandrosterone-sulfate (DHEA-S). These hormones exert their effects primarily by acting as precursors for the more potent androgens testosterone and dihydrotestosterone. It is important to recognize that production of these androgens is independent of the changes occurring in the HPG axis and that maturation may occur at different times.
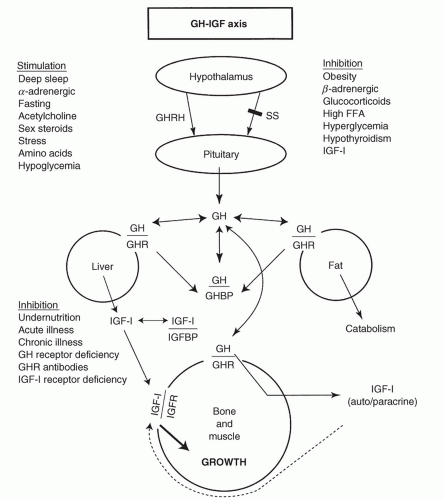
GH Axis
Pituitary secretion of GH is positively regulated by GH-releasing hormone (GHRH) and negatively by somatostatin. GH is released in a pulsatile manner, with maximum secretion at the onset of slow-wave sleep.
The effects of GH are primarily modulated through proteins called insulin-like growth factors (IGFs) and their binding proteins (BPs). The major mechanism for growth appears to be through stimulation of IGF-1 by GH, which affects bone growth. Measurement of IGF-1 and IGFBP-3 levels serves as a surrogate measure of GH production because of significant diurnal variation in GH levels. Serum IGF-1 levels increase with age and pubertal development (Fig. 2.2).
Gonadal Steroids
Estrogen
Estradiol (E2) from the ovary accounts for most of the circulating estrogens, although there is a small amount of extraovarian conversion from androstenedione (to estrone) and testosterone (to estradiol). In addition to stimulating breast growth and maturation of the vaginal mucosa, estrogen has profound effects on the skeleton, being the primary hormone responsible for epiphysial closure. At higher doses, estrogen causes epiphyseal fusion and, therefore, termination of linear growth. The mechanism by which this occurs is thought to involve estrogen’s stimulation of chondrogenesis on the epiphyseal growth plate.1
Testosterone
Although the testes represent the primary source of this hormone, a small amount is generated from the extratesticular conversion of the adrenal hormone androstenedione in both males and females. Testosterone is the primary hormone responsible for the voice change in males and attainment of male body habitus, but it is dihydrotestosterone, the product of conversion of testosterone by 5α-reductase, that causes phallic and prostate growth.
GnRH Pulse Generator and Its Regulators
GnRH Pulse Generator
The exact triggers for the pulsatile hypothalamic release of GnRH that occurs around the time of puberty are incompletely understood, although three distinct changes are observed.
Nocturnal sleep-related augmentation of pulsatile LH secretion begins as a result of the increase in the pulsatile release of GnRH.2 When measuring LH levels to assess for the onset of hormonal activation, levels will initially only be detectable in the early morning, with inherent implications for testing the activity of the HPG axis in early puberty.
The sensitivity of the hypothalamus and the pituitary to estradiol (E2) and testosterone (T) decreases such that the gonadotropins LH and FSH begin to increase.
A positive feedback system develops in females so that rising levels of estrogen trigger GnRH release, stimulating LH to initiate ovulation.
Kisspeptins and the KISS1/GPR54 System
Kisspeptins refer to a class of peptides encoded by the KISS1/Kiss1 gene that act through the receptor, GPR54. These compounds appear to stimulate LH through GnRH at the hypothalamic level and are implicated as necessary for pubertal onset, as well as normal reproductive function.3
Leptin
This product of the ob gene produced by fat cells was initially thought to have a gateway role in pubertal development. It was discovered to play a key role in the regulation of appetite, food intake, and energy expenditure, providing a signal to the central nervous system regarding satiety and the amount of energy stored in adipose tissue.4 With further investigation, its role has been identified as more modest; it appears that leptin is permissive for pubertal advancement at the hypothalamic level by modulation of the GnRH system, although it has also been shown to have effects at other levels of the HPG axis.5
What are commonly thought of as pubertal secondary sexual characteristics should be separated into gonadarche and adrenarche, arising from activation of the HPG axis and HPA axis, respectively. In girls, gonadarche is represented by thelarche, or the onset of breast budding, and in boys by testicular enlargement to 4 mL and above, or 2.5 cm in the longest axis. Pubarche, or the growth of terminal sexual hair in girls, is mainly the result of adrenarche. In boys, both testicular and adrenal androgens contribute.
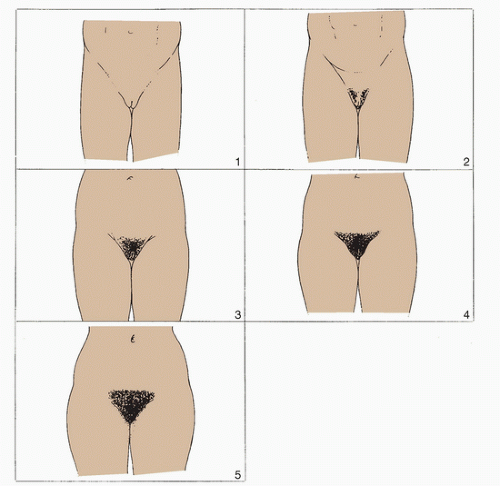
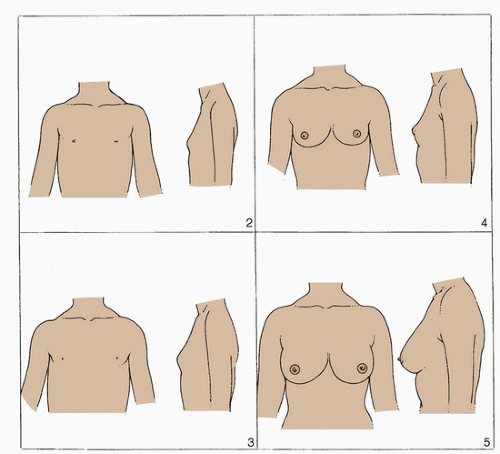
Sexual Maturity Rating Scales
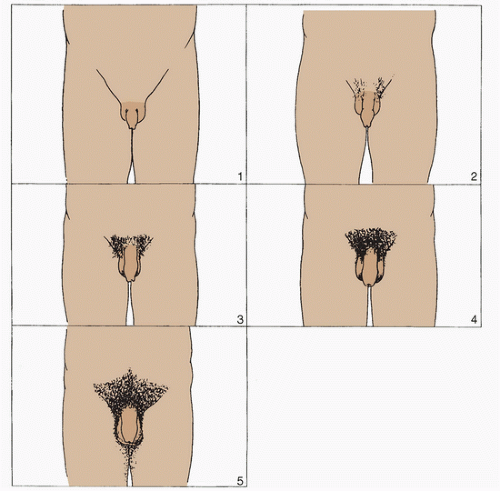
Sexual maturity rating (SMR) scales (also called Tanner staging) as developed by Marshall and Tanner6,7 allow for accurate classification of physical pubertal maturation. For both boys and girls, there are five stages categorizing secondary sexual characteristics (pubic hair and breast development in females, pubic hair and genitalia in males). These stages are described as follows and are shown in drawings in Figures 2.3 to 2.5.
Males (testicular volumes as measured by a Prader Orchidometer)
Genital stage 1 (G1): Prepubertal
Testes: Volume, <4 mL, or long axis, <2.5 cm
Phallus: Childlike
Genital stage 2 (G2)
Testes: Volume, 4 to 8 mL, or long axis, 2.6 to 3.3 cm
Scrotum: Reddened, thinner, and larger
Phallus: No change
Genital stage 3 (G3)
Testes: Volume, 10 to 15 mL, or long axis, 3.4 to 4.0 cm
Scrotum: Greater enlargement
Phallus: Increased length
Genital stage 4 (G4)
Testes: Volume, 15 to 20 mL, or long axis, 4.1 to 4.5 cm
Scrotum: Further enlargement and darkening
Phallus: Increased length and circumference
Genital stage 5 (G5)
Testes: Volume, >25 mL, or long axis, >4.5 cm
Scrotum and phallus: Adult
Females
Breast stage 1 (B1)
Breast: Prepubertal; no glandular tissue
Areola and papilla: Areola conforms to general chest line
Breast stage 2 (B2)
Breast: Breast bud; small amount of glandular tissue
Areola: Areola widens
Breast stage 3 (B3)
Breast: Larger and more elevation; extends beyond areolar parameter
Areola and papilla: Areola continues to enlarge but remains in contour with the breast
Breast stage 4 (B4)
Breast: Larger and more elevation
Areola and papilla: Areola and papilla form a mound projecting from the breast contour
Breast stage 5 (B5)
Breast: Adult (size variable)
Areola and papilla: Areola and breast in same plane, with papilla projecting above areola
Male and Female: Pubic hair
Pubic hair stage 1 (PH1)
None
Public hair stage 2 (PH2)
Small amount of long, slightly pigmented, downy hair along the base of the scrotum and phallus in the male or the labia majora in female; vellus hair versus sexual type hair (PH3)
Pubic hair stage 3 (PH3)
Moderate amount of more curly, pigmented, and coarser hair, extending more laterally
Pubic hair stage 4 (PH4)
Hair that resembles adult hair in coarseness and curliness but does not extend to medial surface of thighs
Pubic hair stage 5 (PH5)
Adult type and quantity, extending to medial surface of thighs
Female Pubertal Changes
Events of Puberty
During puberty, the breasts develop and the ovaries, uterus, vagina, labia, and clitoris increase in size, with the uterus and ovaries increasing in size by approximately five-fold to seven-fold. Body composition changes, as girls accumulate fat mass at an average annual rate of 1.14 kg/year.8
Sequence
Often, the earliest physical sign of puberty in girls is thelarche, although few girls have pubic hair development as the first sign. On average, breast development starts at the age of 10 years for White girls and at 8.9 years for Black girls, according to a frequently cited large cross-sectional study.9 The Breast Cancer and the Environment Research Program (BCERP) examined >1,200 girls longitudinally over 7 years in three urban areas and reported age at thelarche by both visual inspection as well as palpation (in contrast to the Pediatric Research in Office Settings (PROS) study which employed only inspection); median age of thelarche (SMR B2) was 8.8 for Black girls, 9.3 years for Hispanic, and 9.7 years for Caucasian and Asian participants. Notably, higher body mass index (BMI) was associated with earlier attainment of SMR 2.10 These physical findings, however, may be preceded by the growth spurt by approximately 1 year. As a result, the growth curve is an essential tool in the evaluation of precocious or delayed puberty. The average length of time for completion of puberty is 4 years, but can range from 1.5 to 8 years.
Menarche
Menarche usually occurs during SMR B3 or B4, and approximately 3.3 years after the growth spurt, or roughly 2 years after breast budding. The normal range for menarche varies from 9 to 15 years and is dependent on such factors as race, socioeconomic status, heredity, nutrition, and culture. It occurs later at higher altitudes, in rural areas, and in larger families. Body composition also influences age at menarche, although controversy exists whether there is a necessary amount of adipose mass needed at the time of menarche.
Earlier menarche is usually correlated with shorter adult height, although this depends on the degree of estrogen stimulation before menses. Girls with higher or prolonged estrogen levels tend to grow less after menarche. On an average, girls grow 4 to 6 cm after menarche. The sequence of pubertal events in females is found in Figure 2.6. The age at menarche has gradually decreased during the last century. However, this trend has slowed significantly in the past few decades.
Several investigators have examined data from the Third National Health and Nutrition Examination Survey (NHANES III) conducted from 1988 to 1994.11,12,13 One study12 compared data from an earlier US survey 25 years previous to the NHANES III data and found that the average age at menarche had declined only minimally (i.e., by approximately 2.5 months, from 12.8 to 12.5 years). Another study cited up to a 4-month decrease in age at menarche.12 Review of all available data in 2008 suggested a trend toward earlier menarche in the United States between 1940 and 1994, but with a magnitude of change of 2.5 to 4 months, revealing questionable clinical significance.14 All studies that have examined race have demonstrated that Black girls reach menarche the earliest, followed by Mexican American and White girls.
Age at Puberty
Although there are slight differences in the ages of onset, the trend is for earlier pubertal onset, but almost no change in the age at menarche. On an average, girls of Black descent appear to enter puberty earlier than their Hispanic and White counterparts. The large study from the PROS group sampled >17,000 White and Black girls from around the United States with the SMR method and found that the earliest signs of puberty are occurring earlier than previously described.8 In that study, the mean ages at onset of breast development were 8.9 years for Black girls and 10 years for White girls. Pubic hair development started at 8.8 years for Black girls and at 10.5 years for White girls. Similarly, Black girls experienced menarche at 12.2 years, and White girls at 12.9 years.
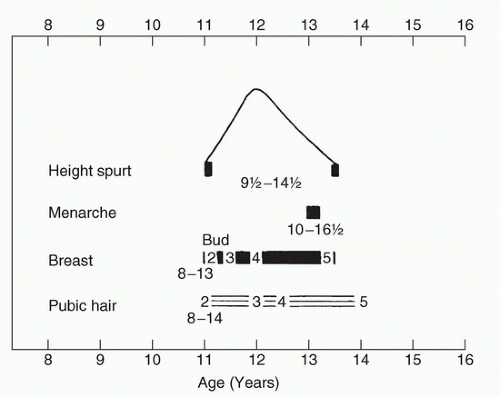 FIGURE 2.6 Biologic maturity in girls. (From Tanner JM. Growth at Adolescence. 2nd ed. Springfield, IL: Blackwell Scientific Publications, 1962, with permission. Copyright © 1962 by Blackwell Scientific Publications.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|