The surgical management of breast cancer has evolved significantly, facilitated by advancements in technology and imaging and improvements in adjuvant therapy. The changes in surgical management have been characterized by equal or improved outcomes with significantly less morbidity. The next step in this evolution is the minimally invasive or noninvasive ablation of breast cancers as an alternative to lumpectomy. In this article, the various modalities for nonsurgical breast cancer ablation and the clinical experience are reviewed, and some of the next steps necessary for their clinical implementation are outlined.
Key points
- •
Nonsurgical ablation has several potential advantages over lumpectomy for the treatment of early stage breast cancer.
- •
A variety of technologies are available for nonsurgical ablation, each with its own advantages and disadvantages.
- •
Ablate and resect trials have shown the ability of nonsurgical techniques such as cryoablation, radiofrequency ablation, and high-intensity focused ultrasonography to completely ablate breast tumors.
- •
There are limited data from ablation alone trials, and many questions remain to be answered before nonsurgical ablation can be considered a viable alternative to lumpectomy.
Introduction
The surgical management of breast cancer has seen a radical evolution over the past several decades, characterized by equal or improved outcomes, with significantly less morbidity. Eradication of the primary tumor has progressed from radical mastectomy (and extended radical mastectomy), through modified radical mastectomy, to lumpectomy. Management of the regional nodes has transformed from routine axillary lymph node dissection (ALND) to sentinel lymph node (SLN) biopsy and ALND for all SLN-positive patients, and ALND for only a few SLN-positive patients. These changes have been facilitated by a multitude of factors, including improvements in technology and screening, better quality and more widely used adjuvant therapies, and countless patients participating in multi-institutional prospective, randomized trials.
The next, seemingly inevitable, step in the evolution of breast cancer therapy would be the replacement of lumpectomy, at least for a select group of patients, with nonsurgical methods for destroying the tumor. Although most of these techniques use thermal energy to destroy the tumor, newer technologies use nonthermal technologies. The potential advantages to nonsurgical breast cancer ablation are multiple, including lower cost of care and simplifying treatment, increased patient comfort, and greatly improved cosmetic outcomes. Various techniques have been used for the in situ ablation of other tumor types, including cancers of the liver, bone, kidney, prostate, and skin. Given recent advances in breast imaging, and our ability to target nonpalpable lesions, it seems logical that breast cancer would be an ideal clinical target. However, many of the technologies for nonsurgical breast cancer ablation have been around for decades, and lumpectomy still remains the absolute standard of care for the treatment of early stage breast cancer. In this article, the clinical experience with a variety of technologies being studied in breast cancer treatment and some of the obstacles to their clinical implementation are reviewed.
Introduction
The surgical management of breast cancer has seen a radical evolution over the past several decades, characterized by equal or improved outcomes, with significantly less morbidity. Eradication of the primary tumor has progressed from radical mastectomy (and extended radical mastectomy), through modified radical mastectomy, to lumpectomy. Management of the regional nodes has transformed from routine axillary lymph node dissection (ALND) to sentinel lymph node (SLN) biopsy and ALND for all SLN-positive patients, and ALND for only a few SLN-positive patients. These changes have been facilitated by a multitude of factors, including improvements in technology and screening, better quality and more widely used adjuvant therapies, and countless patients participating in multi-institutional prospective, randomized trials.
The next, seemingly inevitable, step in the evolution of breast cancer therapy would be the replacement of lumpectomy, at least for a select group of patients, with nonsurgical methods for destroying the tumor. Although most of these techniques use thermal energy to destroy the tumor, newer technologies use nonthermal technologies. The potential advantages to nonsurgical breast cancer ablation are multiple, including lower cost of care and simplifying treatment, increased patient comfort, and greatly improved cosmetic outcomes. Various techniques have been used for the in situ ablation of other tumor types, including cancers of the liver, bone, kidney, prostate, and skin. Given recent advances in breast imaging, and our ability to target nonpalpable lesions, it seems logical that breast cancer would be an ideal clinical target. However, many of the technologies for nonsurgical breast cancer ablation have been around for decades, and lumpectomy still remains the absolute standard of care for the treatment of early stage breast cancer. In this article, the clinical experience with a variety of technologies being studied in breast cancer treatment and some of the obstacles to their clinical implementation are reviewed.
Clinical outcomes
Interstitial Laser Therapy
Mechanism
Interstitial laser therapy (ILT) involves the placement of a laser fiber with a diffusing tip through a trocar into a breast cancer. Laser light is then delivered directly to the target lesion, and the resultant thermal effect results from the interaction between the laser photons and the molecules of the tissue. Absorption of the laser light results in transformation of laser energy to heat, which increases the tissue temperature and creates a zone of thermal ablation. One advantage to ILT is that the optical fibers are magnetic resonance (MR)-compatible, allowing for MR imaging (MRI)-guided ILT.
Clinical experience
There are a few clinical trials examining ILT in the treatment of breast cancer. Akimov and colleagues treated 35 patients, 7 of whom had no further treatment. Among the 28 patients who had surgery after ILT, the investigators described the common histologic findings but did not quantify the number of patients with complete ablation. Among the 7 patients treated by ILT only, 5 achieved local tumor control. There were also some complications, including skin burns and 1 case in which there was gaseous rupture of the tumor, resulting in pain and subcutaneous emphysema. Dowlatshahi and colleagues treated 56 patients with ILT without MRI guidance before surgery and then examined the excised tissue. All patients had tumors with the greatest diameter no larger than 23 mm. Thirty percent of the patients had residual disease, although 2 women who underwent ILT but did not go through with the subsequent surgery had no evidence of recurrence for 2 years. Haraldsdottir and colleagues performed ILT before surgery in 24 patients, but showed complete ablation in only 3 patients with smaller tumors. The inefficacy was mainly caused by the ability to visualize the tumor and judge the extent of laser damage with ultrasonography. Harms used MRI-guided ILT in a population of women with larger tumors. Although the MRI allowed for better contrast and improved resolution, only 3 women achieved complete destruction, all with tumors smaller than 3 cm.
Challenges moving forward
Although ILT has several advantages, including the ability to use MR-guidance and minimal pain, allowing it to be performed under local anesthesia in an outpatient setting, early experience has not shown a reliable ablation of tumors. However, a multicenter ablate and resect trial of ILT for patients with tumors smaller than 2 cm is currently recruiting participants ( ClinicalTrials.gov : NCT01478438 ).
Radiofrequency ablation
Mechanism
Radiofrequency ablation (RFA) involves the placement of an electrode into a tumor. A high-frequency alternating current flowing through the electrode causes ionic agitation, which in turn leads to friction heat and thermal damage, depending on the resultant temperature. Heating to 50°C to 55°C causes irreversible cellular damage in a few minutes, whereas heating between 60°C and 100°C causes instantaneous tissue coagulation. Different types of electrodes are used, including expandable multifilaments and internally cooled and perfusion electrodes. These electrodes determine the size of the area that can be ablated. RFA is typically performed in the operating room (OR) with sedation or general anesthesia.
Clinical Experience
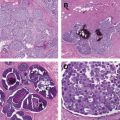
Early on, RFA was the most widely investigated ablation technique for breast cancer. This technique started in 1999, when Jeffrey and colleagues reported the use of RFA in 5 women with locally advanced breast cancer, showing the potential of RFA for lesions smaller than 3 cm. Subsequently, several investigators reported the results of studies in which patients underwent tumor ablation followed by surgical resection 1 to 4 weeks later. One difficulty with RFA is that histologically, it can sometimes be difficult to assess the success of RFA on hematoxylin-eosin staining, because there are often normal-appearing cells within the area of coagulation. Many investigators therefore perform reduced nicotinamide adenine dinucleotide staining for viability after RFA.
In these early ablate and resect studies, the success rates (rate of complete ablation of the tumor) ranged from 76% to 100% ( Table 1 ). The technique was relatively well tolerated, although complications included burns of the skin, local swelling and pain, and thermal damage to the chest muscle and pneumothorax. Based on these results, a handful of investigators have explored the possibility of RFA alone, either with or without radiation therapy. This technique initially started with some small trials in elderly patients who were not believed to be good surgical candidates. Susini and colleagues performed RFA on 3 elderly, unresectable patients and after 18 months of follow-up reported no evidence of local recurrence by either MRI or core needle biopsy. In a similar approach, Marcy and colleagues had no local recurrences in 3 elderly women treated with hormonal therapy, RFA, and radiation.
| Reference | Location | N | Tumor Size (cm) | Complete Ablation (%) |
|---|---|---|---|---|
| Jeffrey et al, 1999 | Stanford, CA | 5 | 4–7 | 80 |
| Izzo et al, 2001 | Naples, Italy | 26 | 0.7–3.0 | 96 |
| Burak et al, 2003 | Columbus, OH | 10 | 0.8–1.6 | 90 |
| Hayashi et al, 2003 | Victoria, BC, Canada | 10 | 0.5–2.6 | 86 |
| Fornage et al, 2004 | Houston, TX | 21 | 0.6–2.0 | 95 |
| Noguchi et al, 2006 | Ishikawa, Japan | 17 | 0.5–2.0 | 100 |
| Earashi et al, 2007 | Yatsuo, Japan | 24 | 0.5–2.4 | 100 |
| Medina-Franco et al, 2008 | Mexico City, Mexico | 25 | 0.9–3.8 | 76 |
| Manenti et al, 2009 | Rome, Italy | 34 | 1.65–1.96 | 97 |
| Imoto et al, 2009 | Tokyo, Japan | 30 | 0.9–2.4 | 92 |
| Wiksell et al, 2010 | Stockholm, Sweden | 31 | 0.7–1.8 | 84 |
| Ohtani et al, 2011 | Hiroshima, Japan | 41 | 0.5–1.8 | 87.8 |
| Kreb et al, 2013 | Hertogenbosch, Netherlands | 20 | 0.4–1.5 | 85 |
Several larger series examined RFA as an alternative to lumpectomy. Oura and colleagues treated 52 patients with tumors 2 cm or smaller as confirmed by mammogram, ultrasonography, and MRI. Under general anesthesia, patients had RFA of the primary tumor and SLN biopsy. To rule out residual disease, fine-needle aspiration was performed 1 month after the operation and MRI was performed 1 to 3 months later. No patients had residual disease, and after 15 months of follow-up there were no recurrences. In a similar trial, Yamamoto and colleagues treated 30 tumors less than 2 cm in 29 patients. Again, this treatment was performed in the OR with SLN biopsy, and after treatment, MRI and Mammotome vacuum-assisted breast biopsy (Mammotome, Cincinnati, OH, USA) were used to ensure no residual disease. Twenty-seven of 29 patients who had posttreatment biopsies showed no viable cells. The 2 patients with viable cells refused additional surgery and went on to whole breast radiotherapy with a boost. With a median follow-up of 17 months, there were no recurrences.
Challenges Moving Forward
As with other hyperthermic ablative techniques, there have been reports of skin burn or burns to the underlying chest wall, and so a subset of tumors, even if they are within the appropriate size limits, would not be good candidates for RFA secondary to proximity to the skin or pectoralis muscle. The 2 most significant challenges facing the use of RFA for the percutaneous ablation of breast cancer are the skills required to perform breast RFA and the difficulty monitoring the ablation with current imaging modalities. To perform RFA, the needle electrode is inserted percutaneously through the tissues until the tip abuts the lesion. The prongs are then deployed. Real-time sonographic monitoring is needed to verify that the prongs are deployed in a symmetric fashion around the lesion, which is more challenging in the breast than other areas in which RFA is used. To ensure successful RFA, the device needs to be at the geometric center, which requires accurate three-dimensional mental images of the location of the tips of the deployed prongs and the anticipated shape and size of the ablation volume. Thus, the level of skill required to perform breast RFA makes it less desirable than other modalities.
Compared with some other techniques, there are no specific sonographic changes during the procedure that can assure the physician that the lesion is reliably ablated. Instead, as the procedure progresses, the visibility of the lesion decreases and by the end can be completely obscured. It is therefore more difficult to be assured that the entire lesion has been adequately treated. Given these challenges, several investigators have shifted away from using RFA as an alternative to lumpectomy and instead are examining its use in combination with excision, either lumpectomy or percutaneous excision.
Cryoablation
Mechanism
Cryoablation is performed by placing a cryoprobe at the center of a tumor. A cryoprobe is a high-pressure, closed-loop gas expansion system, in which the metal probe is insulated, except for the tip. The cryoprobe is rapidly cooled by means of the Joule-Thomson effect (rapid expansion of a gas results in a change in the temperature of the gas), removing heat from the tissue contacting the probe. For ablation of smaller tumors, a single probe is typically placed under ultrasound guidance through the center of a tumor. For larger tumors, multiple probes can be placed to generate cytotoxic isotherms.
Although cryoablation refers to the freezing of tissues, cell damage is induced by a variety of mechanisms during both the freezing and thawing process, as well as indirect damage to the microcirculation. The method by which the cells die is related to the lowest temperature reached, the amount of time at subzero temperatures, and the number of freeze-thaw cycles (allowing the frozen tissue to thaw before freezing again). Close to the cryoprobe, the freezing rates are high enough to induce freezing of the intracellular fluid, or intracellular ice formation. This is a lethal event associated with irreversible membrane damage. Further from the probe, freezing rates are slower. Here, the extracellular fluid freezes, but the intracellular fluid has better protection by the lipid membrane. This situation leads to osmotic forces that shift pure water out of the cell, or cellular dehydration. When the tissue is thawed, the intracellular compartment is hypertonic, and as the ice melts, fluid rushes into the damaged membranes, and the cells burst. In addition, large ice crystals may form during recrystallization in the warming period, and these create direct shearing forces, which further disrupt the tissues. When the freezing is repeated, the damaged tissue conducts the cold more efficiently, increasing the area of necrosis beyond the first cycle. Cells not killed by direct cryoinjury may also suffer apoptotic dell death secondary to cryoinduced destruction of the microvasculature and postthaw platelet aggregation and vascular stasis.
Clinical Experience
Initial experience with cryoablation for breast cancer centered on palliation of locally advanced disease. An initial preclinical and clinical study of in situ cryoablation led to several small series of cryoablation followed by surgical resection ( Table 2 ). Pfleiderer and colleagues treated 16 tumors of any size in 15 patients under ultrasound guidance. The investigators reported that for the 5 tumors smaller than 16 mm, there was no residual invasive cancer after cryoablation, whereas for the 11 tumors greater than 23 mm, ablation was incomplete. Following on this work, these investigators reported a series of 29 patients, limited to tumors 15 mm or smaller, and reported 100% ablation of the visualized tumor. Similar findings were reported in 3 additional series of ultrasound-guided cryoablation. Niu and colleagues reported on 27 patients who underwent successful ultrasound-guided cryoablation, followed by surgery 8 to 35 days later. No invasive cancer was seen in 85.2% of the patients, and as with the study by Pfleiderer and colleagues, this was 100% when restricted to the patients with tumors less than 15 mm. Sabel and colleagues reported on 27 patients treated as part of a multicenter trial, followed by surgery 7 to 30 days later. Complete ablation was seen in 21 (78%), with a success rate of 100% for all tumors smaller than 1.0 cm, and for tumors smaller than 1.5 cm if lobular carcinomas and those patients with an extensive intraductal component on their initial core biopsy were excluded. Manenti and colleagues, limiting cryoablation to lesions 4 to 12 mm in size, had complete ablation in 14 of 15 (93%) patients, with the 1 patient having residual disease secondary to a technical failure. Morin and colleagues treated 25 women, 4 weeks before their scheduled mastectomy. Using MRI guidance rather than ultrasound, these investigators attempted to treat larger tumors (only 2 were <2.0 cm). Complete ablation was achieved in only 13 of 25 women, but this study did show the ability of MRI (combined with scintomammography) to predict the histopathologic results, with an accuracy of 96%.
| Reference | Location | N | Tumor Size (cm) | Complete Ablation (%) |
|---|---|---|---|---|
| Pfleiderer et al, 2002 | Jena, Germany | 16 | 0.9–4.0 | 31 |
| Sabel et al, 2004 | Multicenter, United States | 27 | 0.6–2.0 | 78 |
| Pfleiderer et al, 2005 | Jena, Germany | 29 | 0.5–1.5 | 100 |
| Niu et al, 2007 | Guangzhou, China | 27 | 0.8–2.5 | 85.2 |
| Morin et al, 2007 | Quebec City, Canada | 25 | 1.2–6.0 | 52 |
| Pusztaszeri et al, 2007 | Geneva, Switzerland | 11 | 0.5–2.6 | 20 |
| Manenti et al, 2011 | Rome, Italy | 15 | 0.4–1.2 | 93 |
Two studies have looked at cryoablation alone, without surgical excision. Littrup and colleagues treated 22 lesions in 11 patients who refused surgery. Using ultrasound and computed tomography guidance to place multiple cryoprobes (average of 3), 100% procedural success (defined as 1 cm visible ice around all tumor margins) was obtained, and with a mean follow-up of 18 months, there were no local recurrences. Fukuma and colleagues have presented (but not published) results of 2 clinical trials of cryoablation alone for small breast cancer. In the first study, 38 patients with luminal A invasive ductal carcinoma or ductal carcinoma in situ (DCIS), less than 10 mm in size, were treated. With a median follow-up of 43 months, there were no local recurrences. In the second study, 20 similar patients were treated. MRI and core biopsy failed to detect residual disease after treatment.
Challenges Moving Forward
Early on, breast cancer cryoablation was slow in building momentum, because the equipment needed (often requiring large tanks of gas) made it less desirable than, for example RFA, which requires only a table top device. However, with the increasing use of cryoablation in the treatment of several other malignancies, its US Food and Drug Administration (FDA)-approved use in the treatment of fibroadenomas of the breast, and design improvements that made the equipment more portable and user friendly, momentum has grown. Cryoablation seems to be the most popular ablative technique being investigated, as shown by the recently completed multicenter national trial of cryoablation by the American College of Surgeons Oncology Group (ACOSOG Z1072).
Before cryoablation becomes a viable alternative to lumpectomy, there are still several questions that need to be addressed. Outside the work by Littrup and colleagues, most of the experience with cryoablation has been with a single cryoprobe, limiting treatment to small, well-visualized tumors. Further investigation is needed to determine if this is truly the optimal method for cryoablation. Although ultrasonography and MRI can be used to monitor the procedure, whether MRI can be used to select appropriate patients and accurately predict whether patients have had a complete ablation, or have residual disease after cryoablation (thus requiring excision), is unknown. This question is being examined in the Z1072 trial, and the results of this trial are anxiously awaited. However, the Z1072 trial examined the use of MRI within a few weeks of cryoablation. Inflammatory changes, which can be confused for residual enhancing tumor, can be seen up to 3 months after cryoablation. Further study of MRI, and other breast imaging modalities, may be necessary to determine the appropriate before and after cryoimaging.
Although there is some experience with cryoablation without excision, there are still several unknowns about what happens to the cryolesion after treatment. After cryoablation of fibroadenoma, the lesion initially gets larger, and can take several months before it completely resorbs. This situation may not only be of psychological concern to patients who have breast cancer, but it is not clear how this might affect the delivery of radiation, and how radiation might affect the resorption of the lesion. In a case report by Littrup, 1 patient did have radiation therapy 3 months after cryoablation (delayed to allow healing) and did report resorption of the mass to have stalled during radiation, although it resolved. Although cryoablation and radiation have been used in combination in the treatment of prostate cancer, there are unanswered questions about the timing and complications of radiation therapy to the breast after cryoablation, the impact on surveillance imaging, and the ability to detect recurrence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree