Introduction
This chapter reviews the nonpharmaceutical interventions for the treatment of osteosarcopenia in older adults. Modifiable risk factors such as exercise, nutrition, nutritional supplements, supplements plus nutrition, and complex interventions will be covered. Other factors such as intentional weight loss/regain, and circadian rhythms will also be discussed. Both skeletal muscle and bone have a mesodermal origin making these tissues respond to stimulus such as resistance and aerobic exercise and nutritional interventions, in some similar, but also unique manners. Although genetic factors significantly contribute to the attainment of peak bone mineral density and muscle mass, the impact of modifiable factors such as exercise and nutrition, also play a role in the loss of these tissues with aging . Other lesser studied factors such as rest periods in resistance training, weight loss and regain, and circadian rhythms may also play a role.
The relationship between muscle and bone has been described as a mechanostat model where deformations of the bone in response to muscle contractions are monitored by osteocytes, which in turn signal osteoblasts and osteoclasts to begin modifying bone architecture and mass to maintain bone homeostasis . Thus, it is biologically plausible that the loss of muscle could result in the reduction of bone mass leading to osteosarcopenia . In order to understand the context of designing effective and appropriate nonpharmaceutical interventions, a brief review of the physiological changes in skeletal muscle and bone and their response to external forces (e.g., resistance exercise) and nutrition are addressed followed by more specific recommendations for exercise prescription and nutritional recommendations.
Age-related changes in skeletal muscle and bone
Changes in skeletal muscle
The loss of skeletal muscle involves both the atrophy of fast-twitch muscle fibers (type IIa and IIx) and the total number of myofibers . Resistance training (also called weight or strength training) can be an effective stimulus for hypertrophy of myofibers. The physiological response to resistance training in older adults’ results in a myofiber type redistribution (IIx to IIa) and myofiber hypertrophy across fiber types, which is preferential to type II fiber types . However, the loss of myofiber number does not appear to be reversed by resistance training . Thus, the main adaptation to resistance training in older adults is type II myofiber hypertrophy . Concurrent with the loss of muscle mass, there is a change in neuromuscular function, which occurs faster than changes in muscle mass . There may be ~ 30%–40% fewer motor units in older adults compared with young adults , and the surviving motor units are both larger and undergo remodeling in type I myofibers . It has been suggested that neural activation of the larger type I motor units may also play a role in reduced muscular power in older adults . It is beyond the scope of this chapter to discuss the accumulation of adipocytes in skeletal muscle and bone marrow, which is now recognized as a common feature of aging in these tissues and could impact on response to interventions discussed in this chapter .
Changes in bone mass
Cortical and trabecular bone microarchitecture is essential to the strength of bone. In normal/nonosteoporotic bone the trabeculae are plate-like structures, but these become thinner and more rod shaped with osteoporotic changes . Osteoporotic changes include microarchitecture defects of the trabeculae, defective intrinsic material properties of bone tissue, and defective repair of microdamage to bone . In adults, bone remodeling is the primary mechanism for bone renewal. The remodeling is triggered by signaling from osteoblasts or their matured form osteocytes, which in turn activate osteoclasts. The osteocyte is replaced by bone remodeling and can result in increased hypermineralized calcium phosphate blockages that decrease canalicular fluid flow and negatively impact the osteocyte’s sensing of mechanical loading, which can subsequently lead to microdamage .
Skeletal muscle and bone: Cross talk
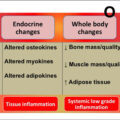
Although the “mechanostat” hypothesis in the interaction between skeletal muscle and bone is important, there are also paracrine and/or endocrine factors involved . Muscle secretes myokines and bone secretes osteokines that play a role in the cross-communication between muscle and bone . For example, Myostatin inhibits skeletal muscle growth but also affects tendons and bone . In skeletal muscle, the age-related bone changes of the lacuno-canalicular system, that was described above, result in fewer factors produced to support muscle myogenesis and function . Skeletal muscle contractions also result in the production of factors that maintain osteocytes, but this is decreased or lost with aging . Other signaling pathways include the Wnt-β-catenin pathway that controls osteoblast activity and is also involved with muscle regeneration . The receptor activator of nuclear factor kappa-B ligand (RANKL), is produced by osteocytes to activate osteoclasts, and the receptor for RANKL, (RANK) is expressed by both osteoclasts and skeletal muscle . In skeletal muscle, RANKL appears to regulate Ca 2 + storage and sarcoendoplasmic reticulum Ca 2 + -ATPase, activity, which has implications for exercise . The Growth Hormone/Insulin-like Growth Factor axis is also involved with the regulation of both muscle and bone . So it is clear that skeletal muscle and bone do not respond and adapt in isolation, but rather cross-talk between these tissues underlies their ability to respond to stimulus.
Research has clearly shown that loading of both skeletal muscle and bone is critical for not only achieving peak muscle and bone mass but also for maintaining these tissues during aging and that there are complex biochemical and signaling pathways involved in the cross-talk between muscle and bone. Unfortunately, in more developed countries low physical activity/exercise is pervasive not only in older adults, but across the life course, leading to an increased risk of not achieving peak skeletal muscle and bone mass and then not maintaining it during aging. There is evidence in community-dwelling older adults that BMI and physical activity are inversely associated with osteosarcopenia and that higher fat mass increases the risk in both men and women with a greater than twofold increased risk in women . Thus, both age and sex may be risk factors for developing osteosarcopenia, but the modifiable risk factors are physical activity/exercise and nutrition. The next section will focus on physiological responses to exercise and nutrition in skeletal muscle and bone.
Exercise
Physiological responses to exercise in skeletal muscle and bone
Acute exercise stimulates the secretion of exosomes with cargo molecules that can mediate the endocrine effects between muscle and bone. Conversely, long-term exercise induces adaptations of the tissue secretome in order to maintain a homeostatic environment . Thus, acute, and long-term adaptations to exercise may not be the same . Both muscle and bone need exercise that is dynamic (rather than static), and that exceeds a threshold of intensity, with adequate nutrition to support adaptation .
As discussed earlier in this chapter, the strain placed on the musculoskeletal system is sensed through cells and translated into biochemical and/or physiochemical responses, which result in bone formation, myofiber hypertrophy, and increased production of the components of the extracellular matrix, adhesion molecules, and elements of the cytoskeletal. Both bone and skeletal muscle secret growth and differentiation factors in response to this stimulus . A stimulus such as resistance exercise changes the tension and compression of skeletal muscle, which stimulates the rapamycin complex 1 (mTORC1) that in turn integrates mechanical strains, nutrients, and growth factors, leading to the activation of signaling pathway that initiates muscle protein translation . Insulin-like growth factor 1 also increases in response to resistance training and activates a PI3K-Akt-mTORC1 signaling pathway to stimulate muscle protein synthesis . The Wnt-catenin signaling pathway is also stimulated by exercise which initiates osteogenesis, either by direct stimulation of bone transcription factor RUNX2 or by cross-talk with Parathyroid hormone or protein signaling pathways . The release of Parathyroid hormone stimulated by exercise also downregulates sclerostin in osteocytes at the same time it upregulates fibroblast growth factor-23 expression, which in turn influences phosphatase homeostasis and vitamin D metabolism . Exercise also increases the OPG/RANKL ratio and downstream inhibition of osteoclast differentiation, promotion of osteoblast differentiation, and bone formation .
As noted in the previous section, acute and chronic exercise training responses are not the same and one does not predict the other. Moreover, the magnitude of the response in skeletal muscle to resistance training is different in younger and older adults . Acute bouts of resistance training may increase muscle protein synthesis lasting up to 48 h whereas repeated bouts of resistance training stimulate the rapamycin complex 1 (mTORC1), which directly promotes protein synthesis via phosphorylation of specific downstream effectors (S6K1, rpS6, eEF2, and 4EBP1). A single bout of resistance training can increase the muscle protein anabolic response to nutritional stimuli and specific myofiber hypertrophy is reported to be partially mediated by differential induction of ribosome biogenesis . Long-term resistance training may increase basal muscle protein synthesis, but in older adults does not further improve the muscle protein anabolic response to amino acids .
As described earlier, bone has an extensive network of cell processes located in the canaliculi, and loading of the skeletal system causes shifts in fluid flow in the lacunae and canaliculi . However, microcracks can transect canaliculi disrupting communication and triggering osteocyte apoptosis. This has a flow-on effect on RANKL and other cytokines to be transmitted to bone surfaces which in turn signals osteoclast precursors to differentiate into osteoclasts for removal and repair by osteoblasts . Liu and colleagues nicely summarized a large number of genes and polymorphisms that are possible candidates for regulating bone mass. This included transforming growth factor B1 (TGF-B1), bone morphogenic proteins (BMPs), sclerostin (SOST), transcription factors such as Runx2, cathepsin K, type 1 collagen (TCIRG1), chloride channel 7 (CLCN7), vitamin D receptor (VDR), and estrogen receptor (ER-a) .
This section has described some of the known cellular responses and adaptations for exercise. Now we will turn to more practical implications of exercise prescription for skeletal muscle and bone.
Exercise modalities
At present, there is no scientific consensus regarding the optimal mode and dose (type, frequency, duration, and intensity) of exercise that can simultaneously enhance bone and muscle health and improve functional ability in older adults with osteosarcopenia. As such this section will address training programs for muscle and bone separately and identify potential overlaps in the training that could be applied to osteosarcopenia.
Skeletal muscle training programs
Resistance training has been shown to be safe and effective for older adults, with rates of injuries extremely low and similar across all ages and intensities as long as exercise sessions progressively increase intensity and the movements are performed with the correct form . Training dose is made up of the frequency (number of days per week), intensity (% of a 1 repetition maximum (RM)), and volume (number of sets and repetitions within a set). The American College of Sports Medicine (ACSM) recommends a minimum of two resistance training sessions per week , although a minimal effective dose of once-weekly has also been shown to elicit adaptations . Other investigations have reported no difference in training response across different training frequencies although the lack of consensus could be the often-overlooked aspect of exercise training which is rest periods both within and between exercise sessions. Stec and colleagues conducted a four-arm, randomized dose-response trial and reported substantially greater gains in total lean body mass, thigh muscle mass, and strength using 3 day/week training, with the second training day at a lower intensity, compared to 3 days that were all high-intensity training .
Most resistance exercise programs use isotonic contractions, which is a concentric contraction where the contracting muscle shortens to overcome an external force . Power training is characterized by rapid concentric movement followed by a slower eccentric (lowering) phase. A review and metaanalyses on power training in older adults reported that it is feasible and safe and has similar gains in muscle strength but better functional outcomes (e.g., chair rising time, stair climbing, walking speed) . Despite this, the majority of resistance training programs utilize slow velocity concentric contractions (2–4 s concentric phase) at a moderate to high intensity . There are even fewer studies that have used isometric (static contractions) or isokinetic (controlled contractions at constant angular velocity using dynamometers).
Looking at the influence of duration of the resistance training program on skeletal muscle mass and strength, a metaanalysis of 49 studies averaging 20 weeks in duration reported the number of sets and repetitions was positively associated with increases in lean body mass . Others reported that using constant intensity for 6–10 weeks showed gains in muscle mass and strength that were similar between higher (3 sets) and lower (1 set) , but by the 20th week there was more benefit from sessions that used a higher number of sets and repetitions . Villareal and colleagues have used high-intensity resistance exercise training (85% 1RM 3 × week) in older obese frail adults and have demonstrated this feasible and effective for mitigating the loss of lean body mass while dieting .
Bone exercise training programs
The current national and international consensus guidelines for osteoporosis recommend a combination of weight-bearing and resistance training with challenging balance exercises to improve falls risk . As discussed in the physiological adaptations to exercise, the stimulation of bone remodeling requires some unique training aspects. A metaanalysis of randomized controlled trials in older adults reported a combination of impact producing weight-bearing impact exercise such as jogging, stair-climbing, and jumping, along with resistance training were most effective for maintaining bone mineral density or preventing bone loss at clinically relevant sites such as the hip and spine . Sufficient loading is needed to stimulate osteogenic bone remodeling and it must be dynamic (i.e., not isometric), with fast high-frequency strains that are progressed over time . As well as the speed of the movement, higher loading intensity requires fewer repetitions to stimulate an osteogenic response . The recommendation is high mechanical load with high velocity (around 80%–85% of 1 RM with fast movements) , performed at least twice a week, and using large muscles targeting the hip and spine . A recently published RCT using Osteo-cise: Strong Bones for Life multicomponent exercise program that consisted of progressive resistance, weight-bearing impact, and balance training (3 days/week) demonstrated significant improvement in the lumbar spine and femoral neck BMD, muscle strength, and physical measures. However, there was no difference in falls incidence or trabecular bone microarchitecture of the distal femur or proximal tibia .
Aerobic training such as swimming, cycling, and walking provide inadequate stimulus to increase bone mass . The message that weight-bearing exercise, such as walking, can preserve bone mass is confusing given walking alone in not an adequate stimulus for bone remodeling. Only if the aerobic exercise includes high-impact or multidirectional weight-bearing is there evidence for maintaining or increasing hip and spine bone mineral density- in older adults .
Current exercise guidelines for people with or at high risk for osteoporosis is moderate-intensity exercises (70%–80% 1 RM, 8–15 repetitions) for individual muscle groups, which are likely insufficient to generate mechanical strain to stimulate an osteogenic response in the hip . Initiating the types of exercise that will increase BMD or slow the loss in people with diagnosed osteoporosis, particularly severe osteoporosis needs to be undertaken with extreme caution due to the risk of low trauma fracture. Similar to the physiological response to resistance exercise in skeletal muscle, recovery or rest periods are also needed for the bone to physiologically respond. Repetitive skeletal loading can desensitize the osteocytes and it has been reported that shorter bouts with rest intervals are more beneficial than the same number of loads performed all at once .
Although skeletal muscle and bone require different interventions to stimulate muscle hypertrophy and osteogenesis, respectively, it has been recommended that a combination of resistance exercise with weight-bearing aerobic exercise (e.g., running, skipping, jumping, or high-impact aerobics) can provide muscular loading while weight-bearing aerobic exercise provides additional mechanical loading to the bone above gravity alone. This approach has been demonstrated in individual studies, systematic reviews, and metaanalyses to increase lumbar spine and femoral neck BMD, and to increase muscle mass, and strength, in older women as well as men . Thus this may be the type of exercise that would be appropriate for people with osteosarcopenia.
In summary resistance exercise either alone or in combination with other exercise interventions increases muscle mass and strength and appropriate high magnitude and intensity stimulus to the skeletal systems slows bone loss and/or increases BMD in both lumbar spine and femoral neck in older adults. Table 1 show summarizes the exercise recommendations for skeletal muscle and bone.
| Exercise modality | Intensity | Speed of movement | Set and repetitions | Frequency | Rest periods | |
|---|---|---|---|---|---|---|
| Skeletal muscle | Isotonic resistance training | High intensity 80%–85% 1RM | 2–4 s contraction phase | 3 sets 6–8 reps | 2–3 times/weekly 1 × weekly minimum effective dose | Alternate high-intensity training days with low intensity |
| Bone | Resistance training or multidirectional high impact movements | High strain | Fast | 3 sets 6–8 reps | 2–3 times/week | Shorter intense bouts with rest intervals |
Now we will briefly discuss nutritional interventions for skeletal muscle and bone with a focus on calcium, vitamin D, and protein.
Calcium
Calcium plays a key role in muscle contraction through calcium-induced calcium release from the sarcoplasmic reticulum and contributes to the strength of bone, nerve impulses and transmission, regulation of heartbeat, and cellular fluid balance . For most people, adequate calcium can be obtained through a balanced diet that includes dairy products (e.g., milk, yogurt, and cheese), nuts, dark-green leafy vegetables, dried peas, and beans . Low dietary calcium intake, high sodium intake, and excessive alcohol and cola consumption are risk factors for low bone mass in older adults . The absorption of calcium through the intestine is increased in people with obesity, but the physiological mechanisms are poorly understood Conversely, caloric restriction resulting in weight loss is associated with decreased intestinal absorption of calcium independent from the effects of vitamin D and may be one mechanism underlying the loss of bone mass with weight loss . In people with osteoporosis who have adequate vitamin D status and a normal calcium intake, routine calcium and vitamin D supplements are not required and supplementation does not appear to affect treatment efficacy for osteoporosis . Calcium supplementation also can have side effects that include constipation, bloating and kidney stones, and a small increased risk of myocardial infarction . Insufficient calcium intake during peak bone growth and mineralization periods may lead to suboptimal bone mass peak and low bone mineralization, possibly contributing to the risk of osteoporosis . Current guidelines recommend an adequate intake of calcium (1000–1300 mg/day) from the diet for optimal bone health .
As noted above, calcium intake and supplementation are controversial. A review of randomized controlled trials and cohort studies concluded that increasing calcium intake from dietary sources cannot prevent fractures . Reid and Bollard also concluded that “calcium supplements in healthy individuals are not needed, nor are they required in most people receiving treatment for osteoporosis” . The European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases and the International Osteoporosis Foundation also concluded that current evidence on calcium supplementation alone does not reduce the risk of fracture .
Thus, for older adults, it appears that the main message is against taking calcium supplementation, but to try to achieve adequate calcium intake through the diet.
Vitamin D
Most of the circulating vitamin D is made in the skin when exposed to sunlight. Dietary sources include oily fish, liver, egg yolks, margarine, some yogurts, cheeses, cereals, and vitamin D-fortified milk and orange juice, but the major source of vitamin D3 comes from sunlight exposure . Many studies have described the association of low vitamin D status with osteoporosis and increased risk of fracture whereas for sarcopenia, Bruyère and colleagues reported that there was an association of low vitamin D levels with negative muscle-related outcomes . Conversely, Reid and Bollard reviewed clinical trials and concluded that vitamin D supplementation had no benefits for nonskeletal endpoints. They also reviewed trials that showed vitamin D increases bone density only when winter 25‐hydroxyvitamin D levels are below 25–30 nmol/L and that supplementation with 400–800 units per day was effective in restoring normal serum vitamin D levels . These low daily doses appear to be safe; however, there is no evidence that loading, or bolus doses have a positive effect on falls or fracture outcomes , in fact, high doses have been shown to increase falls incidence and fractures . Vitamin D toxicity can occur if > 10,000 IU of vitamin D are taken per day for more than 5 months .
One can conclude from these studies and reviews that vitamin D supplementation may only be warranted if 25‐hydroxyvitamin D levels are below 25–30 nmol/L and that lower doses of vitamin D supplementation 400–800 IU/day is sufficient to restore levels to normal ranges.
Protein
There are reports that moderate or high consumption of protein (≥ 1.1 g/kg/day) in older adults (aged 70–79 years) attenuates age-related loss of skeletal muscle and also preserves lower limb performance when compared with protein intake is lower than 0.8 g/kg/day . Data from the Framingham Osteoporosis Study reported that low protein intake was also associated with bone loss at proximal femur and spine over 4 years whereas protein supplements have been reported to increase BMD and decrease fracture risk . An expert consensus for healthy adults have recommended a dietary intake of protein of 0.8 g per kg of body weight per day (g/kg/day), and somewhat surprisingly, this was irrespective of age or sex . However, older postmenopausal women may need up to 1.2 g/kg/day which is similar to the recommendation in older people with frailty living in residential aged care facilities with the additional recommendation to have the protein intake equally split across the meals .
It has been suggested that higher supplemental protein intake is more effective when vitamin D levels are in an optimal range . The level of vitamin D supplementation that was recommended was at least 1000 IU/day, which is much higher than the recommendation by Reid and Bollard . There are other sources of protein such as leucine, β-hydroxy-β-methylbutyrate, creatine, and whey, that are under investigation .
Weight loss and weight regain
Both intentional and unintentional weight loss, either with or without exercise, has been shown to decrease BMD at the hip . Surprisingly, all weight loss/weight loss plus exercise RCTs with older obese people have reported no changes in lumbar spine BMD . These results support an earlier metaanalysis of weight-loss trials that also concluded BMD at the lumbar spine is unaffected by weight loss . The biological mechanisms behind the differential loss of bone at the hip versus the spine have yet to be elucidated. More concerning is that BMD lost with voluntary weight loss in older adults with obesity and in postmenopausal women is not regained with weight regain . The biological mechanisms behind these changes are unknown, but it does suggest negative alterations in calcium balance during weight loss , which may be associated with increased calcium absorption in people with obesity.
Circadian rhythm
The circadian cycle is a molecular clock of approximately 24 h based on light/dark and works as a series of interconnected transcriptional-translational feedback loops . Every cell in the body has a circadian rhythm including muscle and bone and these rhythms are important for the maintenance of bone , regulation of skeletal muscle metabolic homeostasis and possibly bone to muscle crosstalk . Bone formation and resorption have circadian rhythmicity with C-terminal cross-linked telopeptide of type 1 collagen with a low point in the afternoon and a high point at night . In mice, scheduled resistance exercise appears to entrain the circadian clocks , which is intriguing, but not considered in exercise or nutritional interventions in humans. The circadian clock becomes less synchronous with age, which may be associated with visual changes and reduced sensitivity to light, daytime sleeping, and low physical activity , which given the evidence in mice on exercise entraining circadian rhythms could be a new avenue to explore. It is intriguing to think that understanding these pathways might lead to specifically timed exercise and nutrition interventions aimed to alter clock genes in muscle to slow the loss or promote the growth of skeletal muscle mass and subsequently bone mass.
Conclusions
Age-related changes and loss of skeletal muscle and bone appear most responsive to exercise interventions and adequate nutrition is essential for a physiological response to exercise interventions. However, the role of calcium, vitamin D, and protein supplements either with or without exercise is still unclear. It is clear that physiological responses to acute and long-term exercise are not the same and that these mediate the endocrine effects between muscle and bone and adaptations of the tissue secretome. Both muscle and bone require relatively high-intensity resistance exercise (~ 85% 1 RM) for a physiological response. The differentiating factor is bone needing high intensity and speed movements to stimulate osteogenesis and bone remodeling, whereas for skeletal muscle high intensity seems more critical than the speed of the movement. For both bone and muscle walking alone, is not an adequate stimulus, but is an important component of an exercise training regime for older adults. Resistance exercise sessions require adequate recovery both within sessions and between sessions, which is an often-overlooked element of exercise training and requires more research. Another potentially overlooked area of resistance exercise training is the role of circadian rhythms and the impact of weight loss and weight gain, particularly on bone mass.
Based on the separate evidence for sarcopenia and osteopenia one could suggest that a nonpharmaceutical approach for people with, or at risk of, osteosarcopenia would be the approach used for maintaining or increasing bone mass. This should provide adequate stimulus for both muscle and bone and the limited available evidence reports that skeletal muscle/lean body mass does respond to exercise modalities targeting bone. More research is needed on including the other elements discussed in this chapter particularly the role of other proteins supplements and timing of the supplements, recovery during and after exercise sessions, and the timing of training sessions to optimize circadian rhythms.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree