Neoadjuvant systemic therapy in breast cancer treatment was initially utilized for inoperable disease. However, several randomized prospective studies have demonstrated comparable survival with adjuvant chemotherapy in early-stage, operable breast cancer while also decreasing tumor size facilitating breast conservation without significant increases in local recurrence. Response to therapy can predict outcome, with improved survival associated with pathologic complete response (pCR). Triple negative and HER2-positive subtypes show increased pCR rates. A multidisciplinary approach is necessary with neoadjuvant treatment. This can improve rates of breast conservation, provide insights into tumor biology and predict patient outcomes.
Key points
- •
Neoadjuvant chemotherapy in the treatment of breast cancer offers comparable survival benefit to adjuvant chemotherapy.
- •
Response to neoadjuvant systemic therapy and molecular subtype holds important implications for prognosis and individualized patient outcomes.
- •
The addition of trastuzumab to neoadjuvant chemotherapy improves pathologic complete response in patients with HER2-positive breast cancer.
- •
Neoadjuvant endocrine therapy with aromatase inhibitors in postmenopausal women with hormone receptor-positive tumors can significantly decrease tumor burden, thereby facilitating breast-conserving surgery.
- •
Neoadjuvant chemotherapy safely allows for a more limited operative approach with breast-conserving surgery and sentinel lymph node dissection without an increase in local-regional recurrence rates in selected patients.
Introduction
The treatment of breast cancer has evolved from a primary surgical approach with a focus on local-regional control to multidisciplinary management with an emphasis on systemic therapy resulting in significantly improved survival. The optimal timing of systemic therapy relative to operative management has been studied for several decades with strong evidence supporting a neoadjuvant approach to systemic therapy in certain populations. Neoadjuvant therapy implies the initiation of systemic therapy before definitive local-regional management. It is also referred to as primary systemic therapy or preoperative chemotherapy. Although historically reserved for patients with inoperable disease, contemporary management of breast cancer involves a neoadjuvant approach for patients with inflammatory breast cancer, locally advanced disease, and selected patients with early-stage, operable breast cancer. Neoadjuvant chemotherapy has emerged as a powerful treatment modality with individualized prognostic significance based on response to therapy.
Introduction
The treatment of breast cancer has evolved from a primary surgical approach with a focus on local-regional control to multidisciplinary management with an emphasis on systemic therapy resulting in significantly improved survival. The optimal timing of systemic therapy relative to operative management has been studied for several decades with strong evidence supporting a neoadjuvant approach to systemic therapy in certain populations. Neoadjuvant therapy implies the initiation of systemic therapy before definitive local-regional management. It is also referred to as primary systemic therapy or preoperative chemotherapy. Although historically reserved for patients with inoperable disease, contemporary management of breast cancer involves a neoadjuvant approach for patients with inflammatory breast cancer, locally advanced disease, and selected patients with early-stage, operable breast cancer. Neoadjuvant chemotherapy has emerged as a powerful treatment modality with individualized prognostic significance based on response to therapy.
Rationale for neoadjuvant chemotherapy
The paradigm shift from adjuvant to neoadjuvant chemotherapy is rooted in observations of tumor kinetics and the hypothesis of micrometastatic disease present in the early stages of breast malignancy. Fisher and colleagues performed animal studies and observed a change in tumor kinetics with increased cellular proliferation at metastatic sites after resection of the primary tumor. Another concern was resistance to chemotherapy with increased tumor growth resulting in increased drug-resistant variants, suggesting the optimal time for chemotherapy administration was early after diagnosis. These observations along with multiple clinical studies showing benefit in decreasing the primary tumor burden prompted randomized trials examining the potential survival benefit of neoadjuvant chemotherapy over adjuvant systemic therapy in treating disseminated micrometastatic disease. Although this survival advantage was not ultimately demonstrated, a decrease in the primary tumor burden converted some patients to operative candidates and facilitated breast conservation in at least 25%. In addition, insights into prognosis based on tumor response arose as significant clinical implications of neoadjuvant chemotherapy.
Comparison of neoadjuvant to adjuvant systemic therapy
Initiated in 1988, the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-18 protocol was one of the earliest and largest randomized trials of neoadjuvant versus adjuvant chemotherapy for women with operable breast cancer. This study randomized 1523 women to surgery followed by 4 cycles of AC (doxorubicin 60 mg/m 2 and cyclophosphamide 600 mg/m 2 ) or preoperative AC followed by surgery. The planned surgical approach was determined before randomization. All women who were 50 years of age or older were treated with tamoxifen after the completion of chemotherapy and those treated with breast conservation received whole breast radiation therapy. The primary objective of the B-18 study was to determine if neoadjuvant chemotherapy resulted in improved overall survival (OS) and disease-free survival (DFS) as compared with delivery of the same chemotherapy in the adjuvant setting. Secondary aims were to evaluate the effect of neoadjuvant chemotherapy on response in the primary tumor, response in axillary lymph nodes, and facilitation of breast conservation. The investigators found no difference in OS or DFS in women treated with preoperative chemotherapy as compared with those treated with adjuvant chemotherapy. This finding has persisted after 16 years of follow-up. Patients in the preoperative AC group showed 79% objective clinical response, 43% clinical partial response, 36% clinical complete response, and 13% pathologic complete response (pCR) after treatment. This group also had increased incidence of pathologically negative axillary nodal disease and rates of breast conservation. There was a nonstatistically significant trend in increased ipsilateral breast tumor recurrence (IBTR) following preoperative chemotherapy. pCR and posttreatment pathologic negative nodal status emerged as strong predictors of both OS and DFS.
Similar to the NSABP B-18 trial, the European Organization Research and Treatment of Cancer Trial 10902 examined neoadjuvant chemotherapy in women with operable breast cancer as compared with adjuvant therapy. This study randomized 698 women to 4 cycles of preoperative FEC (fluorouracil 600 mg/m 2 , epirubicin 60 mg/m 2 , and cyclophosphamide 600 mg/m 2 ) followed by surgery or the same regimen postoperatively. The investigators found no difference between the treatment groups in OS, progression-free survival, or time to local-regional recurrence. They observed an overall response rate of 49% in the preoperative chemotherapy group with 6.6% of patients experiencing complete clinical response and 3.7% with pCR. They also showed an increased survival advantage with pCR that was not demonstrated with complete clinical response. There was a significant down-sizing in clinical tumor size to less than 2 cm in the preoperative arm from 14% at diagnosis and 47% after treatment compared with 14% and 26% in the postoperative arm, respectively. In the preoperative group, 23% of patients initially planned for mastectomy underwent breast conservation.
A meta-analysis evaluating 9 randomized trials addressing outcomes after neoadjuvant and adjuvant chemotherapy in 3946 patients reached similar conclusions. Investigators reported no difference in OS, disease progression, and distant disease recurrence between the 2 groups. There was a 22% increased relative risk of local-regional recurrence with neoadjuvant chemotherapy. Although this was a statistically significant finding, it was attributed to 3 trials in which patients were not obligated to surgery after complete clinical response and received radiation therapy only. This finding underscores the importance of operative intervention in patients with complete clinical response for maintenance of local control. pCR varied from 4% to 29% reported in 5 studies. In addition, there was a higher rate of breast conservation in the preoperative chemotherapy group. A more recent meta-analysis reviewing 14 trials randomizing a total of 5500 women to neoadjuvant chemotherapy or adjuvant chemotherapy confirmed these findings. Local-regional recurrence, after exclusion of the studies omitting surgical management, was similar among the neoadjuvant and adjuvant chemotherapy groups.
Although these trials did not find increased survival rates following neoadjuvant chemotherapy as hypothesized, they asserted an equivalence of survival benefit with neoadjuvant treatment as compared with the adjuvant setting. In addition, they established the role for neoadjuvant chemotherapy in decreasing the primary tumor burden and facilitating breast conservation without increased risk of local recurrence. Importantly, they demonstrated tumor response as a strong predictor of outcome as evidenced by the association of pCR and survival.
Introduction of Taxanes
The addition of taxanes to an anthracycline-based regimen in the preoperative setting was evaluated in the NSABP B-27 protocol. This study, initiated in 1995, randomized 2411 women with operable breast cancer to receive 4 cycles of preoperative AC followed by surgery, preoperative AC and docetaxel (100 mg/m 2 ) followed by surgery, and preoperative AC followed by surgery and postoperative docetaxel. The primary objective was to determine if the addition of docetaxel could increase OS and DFS. Additional objectives included the effect of preoperative docetaxel in local-regional control, pCR, pathologic axillary down-staging, and breast-conserving surgery.
The investigators found significantly increased rates of objective clinical response (86% vs 91%, P <.001) and pCR (13% vs 26%, P <.001) with the addition of neoadjuvant docetaxel to AC. Also observed were decreased rates of pathologically positive nodes and no further increase in the rates of breast conservation. Again, no difference in OS and DFS was found with the addition of preoperative or postoperative docetaxel. However, patients who experienced a pCR and those who were found to have pathologically negative nodes after treatment continued to show an associated survival benefit.
The above studies suggest that it is not the timing of chemotherapy but rather the chemosensitivity and responsiveness of the tumor influencing OS.
Prognostic significance of tumor response
Perhaps the most intriguing implication of preoperative chemotherapy is the ability to observe in vivo tumor chemosensitivity and the prognostic impact of tumor response.
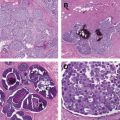
Pathologic Complete Response (pCR)
Neoadjuvant chemotherapy trials have revealed the phenomenon of pCR, defined as no residual invasive tumor on pathologic assessment after therapy. Virtually every study examining the impact of pCR after neoadjuvant chemotherapy for breast cancer has demonstrated an associated survival benefit. Furthermore, neoadjuvant chemotherapy has the potential to decrease the axillary nodal disease burden significantly with 23% of patients converting from clinically node-positive to pathologically node-negative after treatment with anthracycline-based chemotherapy. Patients who achieve pCR in the primary tumor are more likely to have negative pathologic axillary nodal status and the degree of axillary nodal involvement after chemotherapy is highly predictive of outcome.
Discrepancies exist in the literature in defining pCR with some studies reporting pCR in the breast only and others defining pCR as complete response in the breast and axillary nodes, the latter being the currently accepted definition. Importantly, it is only the residual invasive component and not the presence of carcinoma in situ that influences outcome. Factors found to be associated with an increased likelihood of pCR include age less than 40, smaller tumors (<2.0 cm), ductal histology, high nuclear grade tumors, high rate of cellular proliferation (Ki-67), estrogen receptor negativity, triple negative subtype, and human epidermal growth factor receptor 2 (HER2)-positive disease. Although associated with improved survival overall, a small percentage of patients who achieve pCR will develop disease recurrence and distant disease. Significant factors associated with distant metastasis after pCR include clinical stage IIIB or higher, premenopausal status, and 10 or less lymph nodes examined.
The presence of pCR has emerged as a powerful predictor of patient outcome and is used as a surrogate endpoint for prognosis in many clinical trials. As such, pCR has entered into contemporary policy with the recent adoption for use in accelerating drug approval by the Food and Drug Administration.
Prognosis After Neoadjuvant Chemotherapy
In patients who do not achieve pCR, the residual cancer burden (RCB) can be a useful tool to predict survival. This continuous value incorporates 4 parameters that hold prognostic significance after neoadjuvant chemotherapy: the primary tumor dimension, cellularity of the invasive cancer, size of largest nodal metastasis, and number of positive lymph nodes. Increasing RCB values after chemotherapy are associated with increased risk of 5-year distant relapse. When stratified by extent of residual disease, one study showed rates of distant relapse at 5 years were 2.4% in those with minimal residual disease (RCB-I) and 53.6% in those with extensive residual disease (RCB-III). Furthermore, in patients with minimal or no detectable residual disease (RCB-0 or RCB-I) at 5 years, the prognosis was similar to those with pCR. Conversely, patients with extensive residual disease (RCB-III) carried a poor prognosis independent of the type of chemotherapy, adjuvant hormonal therapy, or pathologic stage. In comparison with posttherapy American Joint Committee on Cancer (AJCC) stage group, the RCB was able to classify patients with stage II disease further into 3 distinct groups and stage III disease into 2 distinct groups with different prognoses.
Traditionally, prognosis has been informed by pretreatment TNM (tumor-node-metastasis) clinical stage based on the AJCC system. In the neoadjuvant setting, prognosis is influenced by response to therapy and biologic markers that are not incorporated in traditional staging systems. To address this disparity, a system specifically incorporating the pretreatment clinical stage and posttreatment pathologic stage after neoadjuvant chemotherapy has been described. The Clinical-Pathologic Scoring (CPS) system stratifies patients into groups with increasing CPS scores associated with decreasing 5-year distant metastasis-free survival and disease-specific survival (DSS). A second system, CPS + EG, incorporating estrogen receptor (ER)-negative status and nuclear grade 3 tumors as independent risk factors for poor prognosis, was developed. The CPS + EG system provided refinement of 5-year DSS from 23% to 99% compared with 61% to 92% by clinical stage and 58% to 95% by pathologic stage and recurrence-free survival (RFS) with 5-year RFS rates from 15% to 95% ( P <.001). This system was subsequently validated in an independent cohort, suggesting generalizability among varying institutions with differing populations and practice patterns.
The RCB index and CPS + EG staging system provide further refinement of prognosis by response beyond pCR status to stratify and predict patient outcomes after neoadjuvant chemotherapy. They are prospective tools for clinicians available on-line that can assist with decision-making and advising patients regarding individualized outcome.
Impact of Molecular Subtype on pCR
Determining molecular tumor subtype (luminal, basal, HER2-positive, and normal-like) and approximation of subtype by immunochemistry reveal consistently distinct behavior by subtype in response to neoadjuvant chemotherapy. Generally, more aggressive tumor biology is associated with higher pCR rates and these patients have improved outcomes. Patients with more favorable subtypes are less likely to achieve pCR with neoadjuvant chemotherapy. A meta-analysis of 30 studies examining pCR after neoadjuvant chemotherapy in 11,695 patients found an overall pooled estimate pCR of 19.2% when studies with unknown subtype were excluded. Tumor subtype was strongly associated with pCR% and odds of achieving pCR were 7 times higher for those with HER2-positive/hormone receptor (HR)-negative and 5 times higher for triple-negative subtypes in comparison with the HR-positive subtype. Estimates of pCR were 8.3% in the HR-positive/HER2-negative subtype, 18.7% in the HER2-positive/HR-positive subtype, 38.9% in the HER2-positive/HR-negative subtype, and 31.1% in the triple negative subtype ( P = .002).
Negative HR status has been associated with increased chemosensitivity and improved pCR as compared with HR-positive disease. However, regardless of HR status, pCR has been shown to result in improved progression-free survival and OS when compared with those who do not achieve pCR. This finding is challenged by a pooled analysis of 6377 patients treated with anthracycline-taxane-based neoadjuvant chemotherapy demonstrating variation in the prognostic impact of pCR by tumor factors. In low proliferative subgroups, including lobular histology, grade 1 disease, and positive HR status, achieving pCR conferred no predictive power in DFS or OS. In contrast, in those with ductal histology, grade 2 or 3 tumors and negative HR status, pCR was associated with improved DFS and OS, suggesting that pCR may not be a suitable endpoint in luminal A and luminal B/HER2-negative subtypes.
Some studies have documented a change in HR or HER2 receptor status when biopsy samples are compared with tissue samples obtained from the same patient after neoadjuvant chemotherapy. Change in HR status from positive to negative after neoadjuvant chemotherapy was evaluated in 259 patients from the Shanghai Cancer Center. This study found a positive to negative change in HR status in 15.2% of tumors. In the cases with a change in HR status, there was a higher proportion of tumors with increased Ki-67 index as compared with tumors showing no change in HR status. In addition, the 5-year DFS and OS rates were significantly lower in the group with change in HR status (43.2% and 60.4%, respectively) as compared with the group with no change (67.9% and 81.8%, respectively). Similarly, loss of HER2 amplification after neoadjuvant chemotherapy with trastuzumab has been associated with decreased 3-year RFS as compared with patients who retain HER2 amplification (50.0% vs 87.5%, P = .041).
Neoadjuvant Therapy in Patients with HER2-positive Tumors
Trastuzumab, a humanized monoclonal antibody targeted against the extracellular domain of the HER2 receptor, has revolutionized the treatment of women with HER2-positive breast cancer with increased survival rates reported in the metastatic and adjuvant settings when used in combination with chemotherapy. In the neoadjuvant setting, significantly increased rates of pCR have been observed in patients treated with trastuzumab and chemotherapy versus chemotherapy alone. In a small trial conducted by Buzdar and colleagues, the increased pCR when trastuzumab was combined with chemotherapy was so dramatic (65.2% vs 26.3%, P = .016) that after review by the data and safety monitoring board, the control arm of this phase III, randomized study was terminated prematurely.
Several groups have investigated the use of anti-HER2 therapies in the neoadjuvant setting ( Table 1 ). In the NeOAdjuvant Herceptin (NOAH) trial, women with locally advanced breast cancer were randomized to trastuzumab (loading dose of 8 mg/m 2 followed by 10 cycles of 6 mg/m 2 ) in addition to neoadjuvant chemotherapy (3 cycles of doxorubicin 60 mg/m 2 plus paclitaxel 150 mg/m 2 followed by 4 cycles of paclitaxel 175 mg/m 2 followed by 3 cycles of cyclophosphamide 600 mg/m 2 , methotrexate 40 mg/m 2 , and fluorouracil 600 mg/m 2 ) versus neoadjuvant chemotherapy alone. Trastuzumab was given for 1 year postoperatively. Patients receiving neoadjuvant trastuzumab experienced an increased pCR in the breast and axillary lymph nodes as compared with those treated with chemotherapy alone (38% vs 19%, P = .001). The investigators reported an improved 3-year event-free survival (71% vs 56%, P = .013) with low cardiac toxicity in those patients receiving concurrent trastuzumab with chemotherapy. The use of neoadjuvant trastuzumab was also associated with a trend toward increased breast-conserving surgery (23% vs 13%, P = .07) without an increase in local recurrence, particularly in patients with noninflammatory breast cancer and HR-negative disease.
| Study | Clinical Stage | Neoadjuvant Regimen | n | pCR (%) | DFS (%) | OS (%) |
|---|---|---|---|---|---|---|
| Buzdar et al, 2005, 2007 | II and IIIA | P → FEC | 19 | 26.3 | 85.3 | NR |
| [P → FEC] + H | 23 | 65.2 | 100 | |||
| P = .016 | P = .041 | |||||
| GeparQuattro, 2010 | III | [EC → T or EC → TX or EC → T → X] + H | 445 | 40 | NR | NR |
| NOAH, 2010 | III | AP → P → CMF | 113 | 19 | 56 | 79 |
| [AP → P → CMF] + H | 115 | 38 | 71 | 87 | ||
| P = .004 | P = .013 | P = .114 | ||||
| TECHNO, 2011 | II and III | EC → [P + H] | 217 | 38.7 | 77.9 | 89.4 |
To address the need for concurrent administration of trastuzumab in combination with anthracyclines to achieve high pCR rates, the American College of Surgeons Oncology Group (ACOSOG) Z1041 trial compared pCR rates in the breast for 280 women with operable or locally advanced breast cancer randomized to FEC-75 (fluorouracil 500 mg/m 2 , epirubicin 75 mg/m 2 , and cyclophosphamide 500 mg/m 2 ) followed by paclitaxel (80 mg/m 2 ) with trastuzumab (4 mg/kg first dose, 2 mg/kg subsequent doses) [sequential group] to women treated with paclitaxel with trastuzumab followed by FEC-75 with trastuzumab [concurrent group]. There was no difference in the breast pCR rates between the 2 groups (56.5% vs 54.2%), suggesting that trastuzumab does not need to be delivered concurrently with anthracyclines to achieve high pCR rates. Although cardiac toxicities were low in both arms, further follow-up is needed to assess the cardiac safety of these regimens.
More recently, other HER2-targeted therapies have also been examined in the neoadjuvant setting with and without chemotherapy. The HER2-positive arm of the GeparQuinto trial compared trastuzumab plus chemotherapy with lapatinib plus chemotherapy in the neoadjuvant setting. This trial randomized 620 women with HER2-positive breast cancer and found pCR rates of 30.3% in the trastuzumab arm and 22.7% in the lapatinib arm (odds ratio [OR] 0.68, 95% confidence interval [CI] 0.47–0.97, P = .04), concluding that trastuzumab was superior to lapatinib as HER2-directed monotherapy in the neoadjuvant setting.
Other trials have investigated dual HER2 targeting in the neoadjuvant setting with lapatinib, pertuzumab, and trastuzumab, all of which have differing mechanisms of action ( Table 2 ) and toxicity ( Table 3 ). The NeoALTTO trial, a multicenter phase III trial randomized 455 women to receive either lapatinib, trastuzumab, or the combination in addition to paclitaxel. The investigators found significantly increased breast pCR rates (51.3% vs 29.5%, OR 2.6, 97.5% CI 1.50–4.58, P = .0001), breast and axilla pCR rates (46.8% vs 27.6%, OR 2.39, 97.5% CI 1.36–4.26, P = .0007), and an increased proportion of patients with pathologically negative axillary lymph nodes after surgery (73% vs 58.6%, P = .0115) in the lapatinib plus trastuzumab arm as compared with the trastuzumab-only arm. There was no difference between the lapatinib-only and the trastuzumab-only arms. Toxicity was highest in the lapatinib-treated groups with diarrhea and hepatic toxicity limiting therapy or prompting dose adjustments. Similarly, the NeoSphere study, a randomized multicenter phase II trial investigating the addition of pertuzumab to trastuzumab with or without docetaxel, found a doubling of pCR rates in women treated with dual HER2 therapy in comparison with trastuzumab and chemotherapy alone (45.8% vs 29%, P = .0141). Of note, in the treatment arm whereby patients received dual HER2-targeted therapy without any chemotherapy, the pCR rate was 16.8%, suggesting some patients may benefit from HER2-directed therapy alone without chemotherapy.
| Study | Clinical Stage | Neoadjuvant Regimen | n | pCR (Breast) (%) | pCR (Breast & Axilla) (%) |
|---|---|---|---|---|---|
| NeoALTTO, 2012 | II and IIIA | Lapatinib → lapatinib + P | 154 | 24.7 | 20 |
| H → H + P | 149 | 29.5 ∗ | 27.6 ∗ | ||
| Lapatinib + H → lapatinib + H + P | 152 | 51.3 ∗ | 46.8 ∗ | ||
| ∗ P = .0001 | ∗ P = .0007 | ||||
| NeoSphere, 2012 | II and III | H + T | 107 | 29 ∗ | 21.5 |
| Pertuzumab + H + T | 107 | 45.8 ∗ | 39.3 | ||
| Pertuzumab + H | 107 | 16.8 | 11.2 | ||
| Pertuzumab + T | 96 | 24 | 17.7 | ||
| ∗ P = .0140 | |||||
| CHER-LOB, 2012 | II and IIIA | [P → FEC] + H | 36 | NR | 25 |
| [P → FEC] + lapatinib | 39 | 26.3 | |||
| [P → FEC] + H + lapatinib | 46 | 46.7 | |||
| P = .019 | |||||
| TBCRC 006, 2013 | II and IIIA | Lapatinib + H | 113 | 27 | NR |
| TRYPHAENA, 2013 | II and III | [FEC → T] + H + pertuzumab | 72 | 61.6 | 50.7 |
| FEC → [T + H + pertuzumab] | 75 | 57.3 | 45.3 | ||
| Carboplatin + H + pertuzumab | 76 | 66.2 | 51.9 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree