Highlights
- •
Serial mpMRI scans revealed upgrade to PIRADS≥3 in 31.4≥ cases with a PIRADS-2 index lesion.
- •
A PSA increase of ≥25% during follow-up was the only predictor of mpMRI upgrade.
- •
This information can be valuable for clinicians in deciding when to request a repeat mpMRI during follow-up.
Abstract
Introduction/Background
The natural history of prostate imaging reporting and data system (PIRADS) score 2 lesions on serial mpMRIs is largely unknown. Herein, we aimed to evaluate the patients with PIRADS-2 index lesions by using serial mpMRI scans to reveal the rates of mpMRI upgrade in PIRADS score and prostate cancer (PCa) detection.
Methods/Materials
All mpMRI scans with a PIRADS-2 index lesion from our mpMRI database were evaluated retrospectively. Data from 214 biopsy-naïve patients with a PIRADS-2 index lesion on the initial mpMRI who then underwent at least 1 follow-up mpMRI were reevaluated by an experienced uroradiologist and only those ( n = 172) who had a PIRADS-2 index lesion on the initial mpMRI according to PIRADS v2.1 were included in the study. mpMRI progression was defined as the detection of any PIRADS ≥3 lesion at follow-up mpMRI. Histopathological results were evaluated in patients undergoing biopsy upon mpMRI progression.
Results
A total of 172 patients with a mean age of 60.1 ± 8.6 years were evaluated. The median PSA at baseline mpMRI was 4.7 (IQR; 3.3–6.7) ng/dl. Overall mpMRI progression was detected in 54 patients (31.4%), 37 were upgraded to PIRADS-3, 16 to PIRADS-4, and one to PIRADS-5. Multivariate logistic regression analysis revealed that a PSA increase of ≥25% during follow-up was the only predictor of mpMRI upgrade ( P = 0.019, OR: 2.384). 30 out of 54 patients underwent a prostate biopsy and PCa was detected in 15 patients; 5 with ISUP grade 1, 10 with ISUP grade 2.
Conclusions
Almost half of the patients with a PIRADS-2 index lesion were upgraded to PIRADS ≥3 when evaluated with serial mpMRI when a PSA increase of ≥25% was observed during follow-up. PCa was detected in half of the patients who underwent a biopsy. Serial mpMRI can be recommended when monitoring patients with elevating PSA ≥25%, a prostate biopsy can be considered upon a mpMRI progression.
1
Introduction
Multiparametric magnetic resonance imaging of the prostate (mpMRI) has been fully integrated into clinical practice and routinely recommended in asymptomatic men with a serum prostate-specific antigen (PSA) level between 3 and 10 ng/dL to decide whether a prostate biopsy is indicated [ ]. In patients with a prostate imaging reporting and data system (PIRADS) 4 or 5 index lesion, the risk of prostate cancer (PCa) is considered high and a prostate biopsy is routinely performed. The PIRADS-3 index lesions are considered “the gray zone” and the decision to perform a prostate biopsy is made according to additional clinical parameters such as age, PSA density (PSAD), biopsy-naïve status, family history of PCa, and 4K test score [ , ]. In cases with PIRADS 1 or 2 index lesions, no further biopsy is recommended unless other clinical parameters did not indicate a high risk of PCa such as suspicion on digital rectal examination (DRE) or very high PSAD [ , ]. When these patients are followed up without prostate biopsy, they are monitored with additional serum PSA tests, and persistently high or even increasing PSA levels are frequently observed which creates a clinical dilemma whether additional mpMRI scans should be recommended or not.
Although PIRADS 1 and 2 lesions are considered negative mpMRI results, the distinction between the 2 is based on differences in morphological features and diffusion restriction characteristics, and PCa detection rates are known to be higher in PIRADS-2 lesions (compared with PIRADS-1 lesions) if a prostate biopsy was performed [ , ]. In this study, we aimed to investigate the mpMRI upgrade rates (to PIRADS ≥3) and PCa detection rates in patients with PIRADS-2 index lesion who underwent serial mpMRI scans during follow-up .
2
Patients and methods
We retrospectively investigated all cases with an PIRADS-2 index lesion from our mpMRI database between September 2012 and July 2022. The index lesion on a mpMRI was defined as the lesion with the highest PIRADS score and the largest size (in multifocal lesions with the same PIRADS score). The PIRADS scoring of the lesions was performed according to the up-to-date PIRADS scoring system at the time of the mpMRI scan (PIRADS v1, v2, and v2.1) by a team of uroradiologists ( n = 4) at our center [ , , ]. Biopsy-naïve patients with a PIRADS-2 index lesion ( n = 214) who underwent at least 1 follow-up mpMRI for their persistently high ( n = 62) or rising serum PSA level ( n = 135) or clinical suspicion (suspicion on DRE ( n = 5), family history ( n = 10), and a novel symptom such as hematospermia ( n = 2) were identified. The decision to perform another follow-up mpMRI was at the discretion of the attending urologist. All patient characteristics and the serum PSA values at the time of mpMRI scans were recorded. The serum PSA level was adjusted in patients under 5α-reductase inhibitor (5-ARI) medication for more than 6 months (multiplied by 2). PSA density was determined by dividing serum PSA by the prostate volume calculated from mpMRI. Prostate volume was measured with the ellipsoid formula using manual measurements from the largest cross-sectional dimensions. (anteroposterior × transverse × craniocaudal × π/6). The anteroposterior diameter was measured on the sagittal T2-weighted images as recommended by PIRADS version 2.1 [ ]. PSA velocity was defined as the change in serum PSA divided by the time (years) interval between sequential mpMRI scans. mpMRI progression was detected in 54 patients at follow-up mpMRI scans. A prostate biopsy was recommended in all patients who had an mpMRI upgrade. Out of 54 patients with a mpMRI upgrade, 8 were lost to follow-up. At a median follow-up of 28.9 months (IQR: 21.8–38.0) after the detection of mpMRI upgrade for the remaining 46 patients, 30 patients underwent prostate biopsy, 8 underwent transurethral prostate resection (TURP) instead of prostate biopsy (all had PIRADS-3 lesions) due to accompanying moderate-to-severe lower urinary tract symptoms, and 8 were monitored with additional serum PSA tests and mpMRI scans due to accompanying comorbidities or patient preference. Of those who underwent a prostate biopsy, 28 out of 30 patients underwent an MRI/US-fusion-targeted biopsy using the UroNav biopsy platform (Invivo corporation, Gainsville, FL) while the remaining 2 patients underwent in-bore biopsy using a commercially available biopsy device (Dyna TRIM; Invivo Corporation, Gainesville, FL, USA). Histopathological results of prostate biopsies and TURPs were recorded. Any International Society of Urological Pathology (ISUP) grade group (GG) ≥2 disease was considered as clinically significant PCa (csPCa). This study was conducted according to the principles of Helsinki and local ethics committee approval was obtained (Decision number: 2022.229.IRB1.084).
2.1
Multiparametric MRI protocol and image analysis
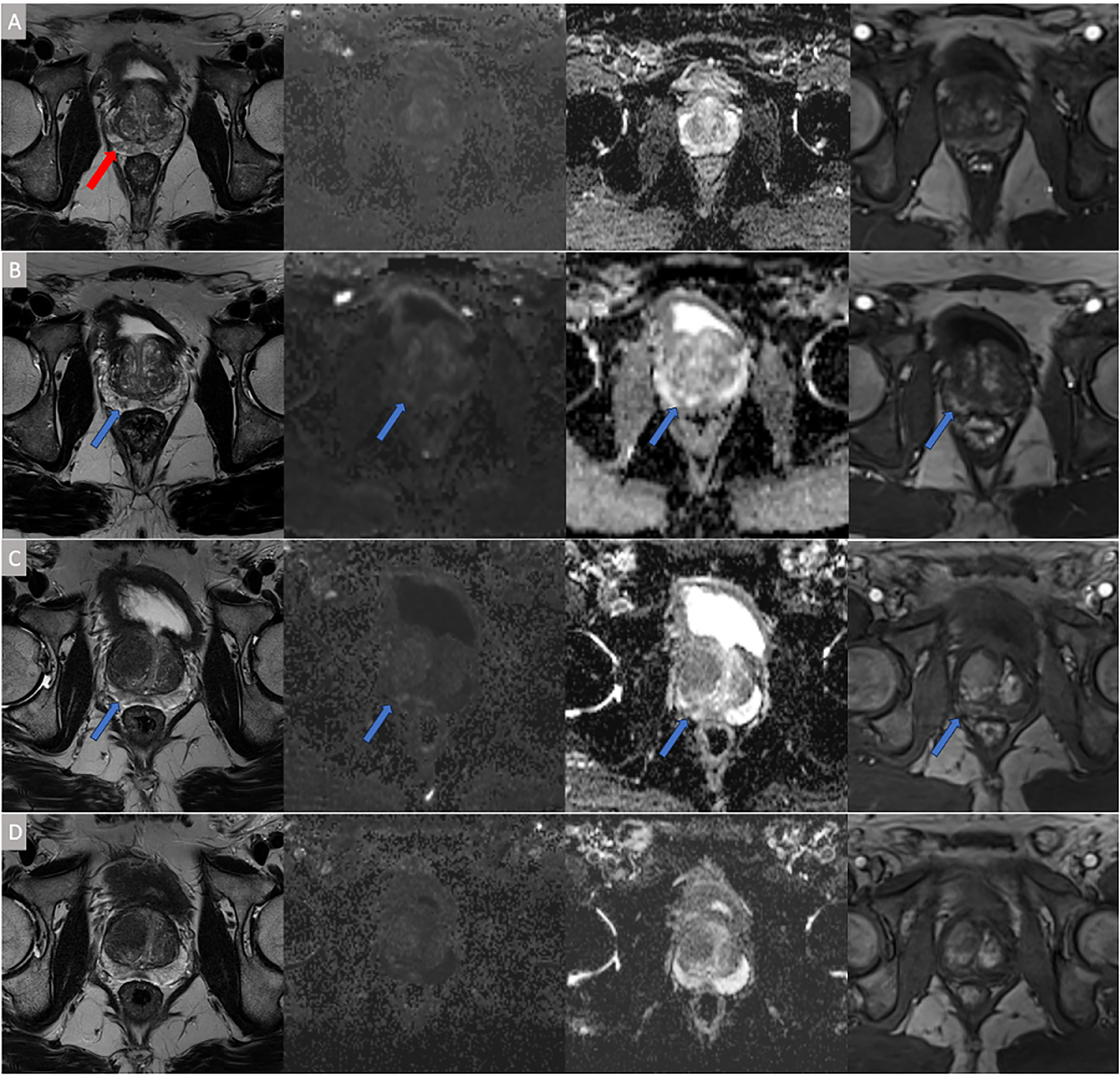
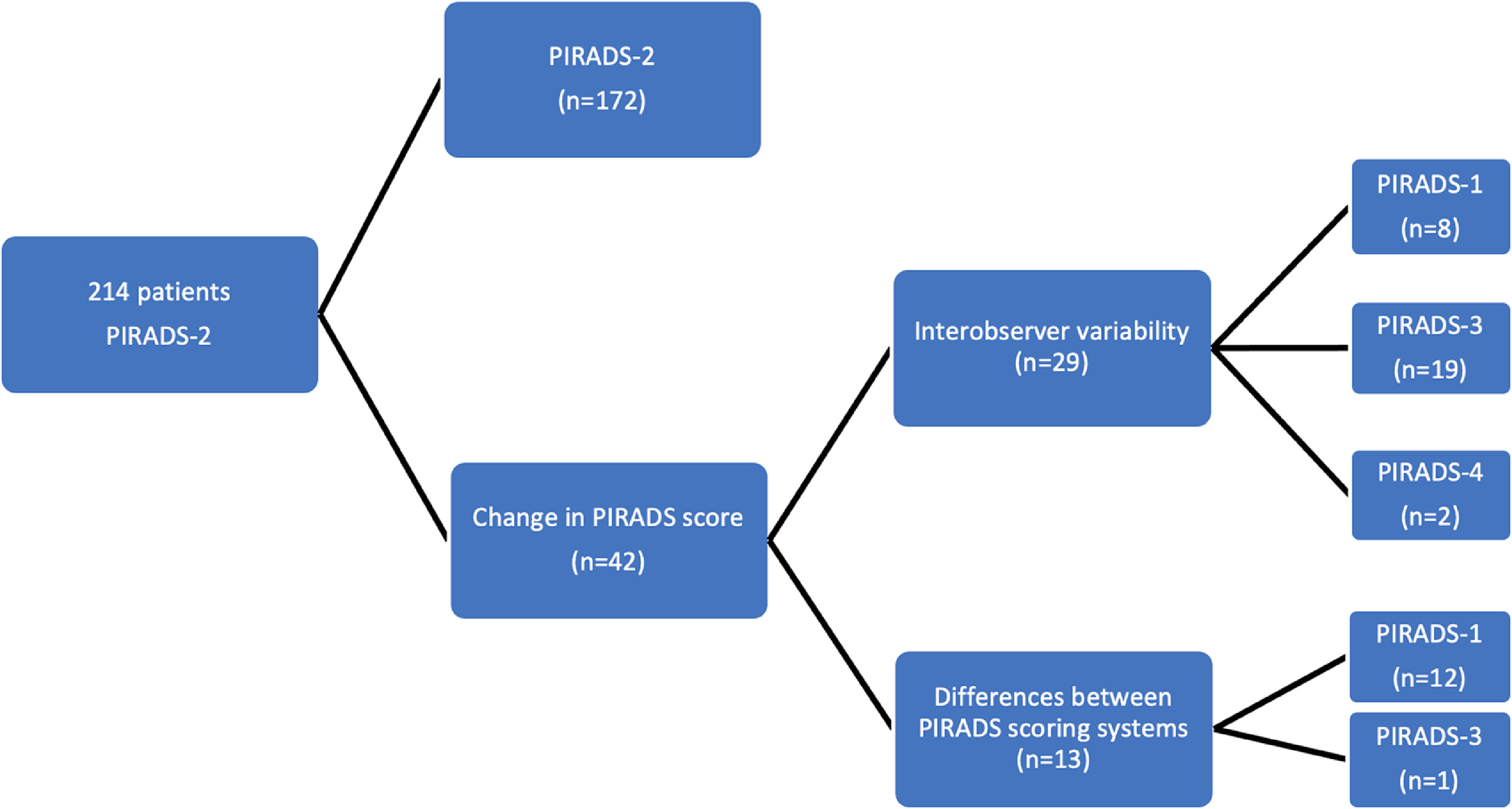
mpMRI was performed with a 3-T device (Magnetom Skyra; Siemens AG, Munich) using a 16-channel pelvic phased array coil. The PIRADS scoring system was utilized to classify prostatic lesions in all cases. PIRADS v1 was utilized until 2015, PIRADS v2.0 between 2015 and 2019, and PIRADS v2.1 has been used since March 2019 in our center. In patients who underwent serial mpMRI after detecting PIRADS-2 index lesions, baseline mpMRI, and follow-up mpMRI scans were re-evaluated by a uroradiologist (B.G) highly experienced in prostate MRI imaging (reporting mpMRI scans using PIRADS scoring system since 2012 with an average of 80 scans/month) according to PIRADS v2.1 to avoid evaluation alterations between different radiologists and different PIRADS scoring systems. The radiologist was blinded to clinical characteristics such as PSAD, PSA dynamics, or subsequent biopsy pathology results while re-evaluating the mpMRI scans. In 172 out of 214 (80.4%) patients, baseline mpMRI remained to harbor a PIRADS-2 index lesion after re-evaluation. In 13 cases (6.1%), PIRADS-score changed due to the differences between PIRADS v2.1 and the previous versions of PIRADS scoring systems (to PIRADS-1 in 12 cases and to PIRADS-3 in 1 case). In the remaining 29 cases (13.6%), the uroradiologist did not agree with the previous reporting and changed the PIRADS score of the index lesions; to PIRADS-1 in 8 cases (3.7%), to PIRADS-3 in 19 cases (8.8%), and to PIRADS-4 in 2 cases (0.9%). Therefore, 42 patients who did not have a baseline PIRADS-2 index lesion on mpMRI according to the PIRADS v2.1 scoring system were excluded from further analysis ( Fig. 1 ). mpMRI progression was defined as the detection of any PIRADS ≥3 lesion at follow-up mpMRI. For patients with mpMRI progression at follow-up scans, the nature of mpMRI progression was categorized as; the detection of a novel PIRADS ≥3 lesion or progression of a previous PIRADS-2 lesion due to an increase in diffusion restriction or an increase in size.
2.2
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences version 24 (SPSS Inc., Chicago IL, USA). Descriptive statistics were provided for all parameters using means and medians for continuous variables and proportions for categorical variables. Chi-square or Fisher’s exact test was utilized to compare proportions in different groups. The logistic regression analysis was performed to determine the predictors of mpMRI upgrade. Results were presented with odds ratios (OR) and 95% confidence intervals (CI). A P -value of less than 0.05 was considered statistically significant.
3
Results
3.1
Baseline characteristics and outcomes of serial mpMRI scans
A total of 172 patients with a mean age of 60.1 ± 8.6 years were included in the analysis. The median PSA at baseline mpMRI was 4.73 (IQR; 3.28–6.71) ng/dl. The median PSAD was 0.08 ng/ml 2 (IQR: 0.06–0.11). About 131 patients (76.2%) had 2 mpMRI scans, 27 (15.7) had 3, 10 had 4 (5.8%), and 4 (2.3%) had 5 scans. Overall mpMRI progression was detected in 54 patients (31.4%); 37 (68.5%) were upgraded to PIRADS-3 lesion, 16 (29.6%) to PIRADS-4, and 1 (1.9%) to PIRADS-5. In patients with mpMRI upgrade; a novel PIRADS ≥3 lesion was detected independently from previous PIRADS-2 index lesion in 30 cases (17.4%). In the remaining 24 cases (14%) the PIRADS-2 index lesion progressed to PIRADS ≥3 due to an increase in diffusion restriction (decrease in ADC) or size ( Fig. 2 ). The PIRADS score of the upgraded lesion was PIRADS-3 in the majority of the cases both in those who had upgraded from PIRADS-2 index lesion (70.8%) and in cases who had a novel PIRADS ≥3 lesion in the follow-up mpMRI scan (66.7%). mpMRI upgrade was more commonly observed among patients who underwent more than 1 mpMRI scans after the detection of PIRADS-2 index lesion, compared to those who had only 1 follow-up mpMRI scan (54% vs 24%, P < 0.001). The median time interval from baseline mpMRI to mpMRI upgrade was 22.81 mo (IQR: 13.07–31.42). mpMRI upgrade rate was notably higher in patients who experienced a PSA increase of ≥25% above their PSA level when a PIRADS-2 index lesion was initially detected compared to the remaining patients. (47% vs 27%, P = 0.017). Multivariate logistic regression analysis revealed that a PSA increase of ≥25% during follow-up was the only predictor of mpMRI upgrade ( P = 0.019, OR: 2.384) ( Table 1 ). Among patients with a PSA increase of ≥25%, there was no difference in PSA velocity between those with and without a mpMRI upgrade ( P = 0.111).