99 David P. Steensma and Richard M. Stone • The myelodysplastic syndromes (MDS) are a group of clonal marrow failure syndromes originating in a hematopoietic progenitor or stem cell. Approximately 25% to 30% of MDS cases progress to acute myeloid leukemia (AML), which is defined by 20% or more marrow blasts. • Approximately 50% of MDS cases are associated with a karyotypic abnormality, usually chromosomal aneuploidy. • Recurrent MDS-associated somatic mutations are now recognized in more than 25 genes. Some of these mutations have prognostic value independent of existing risk stratification tools. • The most important risk factor for MDS is aging. The risk of developing MDS increases greatly after age 65 years. The median age at diagnosis in the United States is approximately 71 years. • Approximately 10% to 15% of MDS cases arise as a consequence of therapeutic or environmental exposure to a DNA damaging agent; these are termed secondary or therapy-related MDS. In patients who had been exposed to ionizing radiation or alkylating agents, abnormalities of chromosomes 5 and 7 are common. Patients treated with topoisomerase II inhibitors may develop rearrangements of the MLL gene at 11q23 or the MECOM (MDS1/EVI1) locus on chromosome 3q21q26. • Patients who develop MDS before age 40 years without a recognized toxin exposure may have a germline DNA repair defect or congenital marrow failure syndrome, such as Fanconi anemia or dyskeratosis congenita. Chromosome breakage analysis and telomere length analysis is appropriate in such patients. • The 2008 World Health Organization (WHO) classification of MDS, refined from the 2001 WHO and 1982 French–American–British (FAB) MDS classifications, defines several subtypes of MDS with varying risk of AML progression or death. The specific diagnosis depends on the proportion of marrow blasts, the number of cell lineages involved by disease, and the presence or absence of ring sideroblasts or chromosome 5q deletion. • Minimal diagnostic criteria for MDS (after exclusion of other causes of cytopenias) include either: 10% or more dysplastic cells in one or more myeloid lineages, increased marrow blasts (≥5%), or the presence of a cytogenetic abnormality or another marker of clonal hematopoiesis. • The incidence of MDS is at least 4 cases per 100,000 persons per year in the United States. Most patients have lower-risk disease at the time of initial diagnosis. • Not all marrow dysplasia represents MDS. Other causes of cytopenias and abnormal cell morphology must be considered in the initial evaluation of patients, such as nutritional deficiency (e.g., vitamin B12, folate, copper), inflammation, excessive alcohol use, human immunodeficiency virus infection, and non-MDS neoplasms. • In ambiguous cases, the presence of an MDS-associated cytogenetic abnormality, such as deletion of chromosome 5q, can confirm the diagnosis. • Several prognostic tools, including the 2012 Revised International Prognostic Scoring System (IPSS-R), are in widespread use and aid in risk stratification and therapy choice. In general, older patients with higher blast proportion, more severe cytopenias, and higher-risk cytogenetic results have a poorer outlook. • Complications of peripheral blood cytopenias and functional cell defects, including infection and hemorrhage, are the most common causes of death in MDS. Progression to AML following MDS occurs in 25% to 30% of cases and is usually fatal. • In lower-risk cases, supportive care alone may be appropriate. Epoetin or darbepoetin may alleviate MDS-associated anemia. • Anemia of MDS associated with chromosome 5q deletion frequently responds to lenalidomide. Thrombocytopenic patients respond less well. • Chronic red blood cell transfusion can lead to iron overload and is an adverse prognostic marker. The appropriate use of iron chelation therapy in MDS is controversial. • Azacitidine has been demonstrated to improve survival compared with supportive care in higher-risk MDS. Another DNA methyltransferase inhibitor, decitabine, can also induce hematologic and cytogenetic responses. • Allogeneic stem cell transplantation is the only potentially curative therapy, and should be considered for patients with higher-risk MDS who are younger than age 75 years and have a matched donor. Second- or Third-Line Therapies • Once azacitidine or decitabine fail the patient, or if relapse occurs after a stem cell transplantation, the outlook is very poor, with a median survival less than 6 months. There is currently no established second-line therapy for MDS. Clinical trial enrollment is especially important for this patient group. The term myelodysplastic syndromes (MDS) describes a heterogeneous group of acquired bone marrow failure syndromes that are collectively characterized by clonally restricted and ineffective hematopoiesis.1 MDS-associated ineffective hematopoiesis results in peripheral blood cytopenias, despite a bone marrow that is frequently normocellular or hypercellular when compared with age-matched controls. In addition, MDS carry a variable risk of progression to acute myeloid leukemia (AML), which is currently defined by the World Health Organization (WHO) as the presence in the marrow of 20% or greater blast cells with myeloid lineage markers—that is, immature, neoplastic cells that express myeloid-associated cell surface antigens—that are positive cytochemically for myeloperoxidase, Sudan black, or nonspecific esterase, or which express AML-associated chromosomal or molecular abnormalities.2 MDS are a relatively recently identified group of medical conditions, and the terminology used to describe these disorders has historically been varied and at times confusing, including nonspecific eponyms such as “di Guglielmo syndrome,” which was once used to describe any erythroid-dominant myeloproliferation.3,4 A detailed history of the evolving concept of MDS and key discoveries contributing to the current state of understanding was recently published.5 In 1938, Rhoads and Barker in New York described 100 patients with anemia who failed to improve during therapy with hematinics such as iron salts or liver extract.6 These patients were described as having “refractory anemia”; a few of them may have had MDS. The term refractory anemia, although coined more than 7 decades ago and in a different context, persists to the present day, even though the anemia of MDS is, fortunately, not always “refractory” to contemporary therapies. A link between a cytopenic prodrome and subsequent development of overt AML was established by French investigators, including Chevalier in the early 1940s and this association was highlighted by Block and Jacobsen in Chicago in their landmark description of “preleukemic acute human leukemia” in 1953.7,8 Björkman in Sweden described acquired sideroblastic leukemia in 1956, which would later become understood as another form of MDS, while by the 1960s chronic myelomonocytic leukemia (CMML) was recognized as a potential precursor state for acute leukemias with monocytic differentiation.9,10 In 1973, Saarni and Linman published the first case series of 143 patients with MDS, which was then termed “preleukemia.”11 By the time of the first formal classification of the acute leukemias by the French–American–British (FAB) Co-Operative Group (in 1976, 3 years after Saarni and Linman’s report), the term “preleukemia” had begun to fall out of favor, as most patients with “preleukemia” never went on to develop leukemia, yet were still at risk for death from complications of disease-associated cytopenias and functional neutrophil or platelet defects.12,13 After a brief vogue for the term “dysmyelopoietic syndromes,” the seminal 1982 FAB classification (Table 99-1), described further below, used the term “MDS,” a moniker that has been with us ever since.14 Table 99-1 French–American–British (FAB) Classification of Myelodysplastic Syndromes (1982) AML, acute myeloid leukemia; MDS, myelodysplastic syndrome. *In the FAB classification, RARS is additionally defined by ≥15% ring sideroblasts among erythroid precursors, and CMML is additionally defined by ≥1 × 109/L peripheral blood monocytes. Adapted from Bennett JM, Catovsky D, Daniel M-T, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 1982;51:189–199. Although the terminology used by clinicians and pathologists to describe MDS is more consistent than it was 30 years ago, confusion about the precise biological nature of MDS continues. Even though MDS are clearly neoplastic—numerous AML-associated acquired genetic mutations are present in MDS cells, and most of the hematopoietic cells are clonal at the time of MDS diagnosis, long before progression to leukemia15,16—some doctors continue to describe MDS to their patients as peculiar forms of anemia or as marrow failure syndromes without using the word “cancer,” and cancer-specific insurance policies routinely exclude coverage for MDS diagnoses.17,18 The Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute and its associated cancer registries began formally tracking MDS only in 2001.19,20 Diagnosis of MDS can be difficult; choice of therapy, even more so.21 Patient outcomes also vary widely, with the highest-risk patients with MDS having a median survival of only a few months, while those afflicted with the most indolent forms of disease are likely to live for a decade or more.22 (Increasing recognition of this diversity in clinical course and accompanying biological heterogeneity accounts for why the singular usage “myelodysplastic syndrome” is steadily shifting to the plural term, “syndromes.”) Therefore diagnosis and subsequent care of the patient require coordination among a pathologist with morphologic expertise who can diagnose the condition with confidence if characteristic cellular changes are present; a cytogeneticist or molecular pathologist who can reliably identify typical subcellular and genetic abnormalities associated with MDS; a clinical hematologist-oncologist able to assess the patient’s risk and individualize therapy; and, in some cases, a multidisciplinary team experienced in bone marrow and stem cell transplantation. The incidence of MDS has proven difficult to estimate accurately.23 In the United States, early SEER data following initial inclusion of MDS in the program in 2001 suggested an incidence of approximately 3.3 to 3.6 cases per 100,000 people per year in the general population, and 20 cases per 100,000 persons in individuals older than age 65 years.19,20 These SEER data also indicated that the incidence of MDS may be increasing over time, either because of greater recognition of these diseases or a genuine increase in disease frequency. Based on these United States registry data, it has been estimated that approximately 10,000 to 15,000 patients are diagnosed with MDS in the United States each year.19,20 However, a study of Medicare claims data (Medicare is a U.S. government health care payer) suggested a much higher incidence of MDS, approximately 75 cases per 100,000 persons older than age 65 years.24 Although this analysis may be confounded by the use of MDS codes on claims in order to justify use of certain therapies for incompletely evaluated cytopenic patients, if the Medicare data are accurate, more than 45,000 patients in the United States are diagnosed with MDS each year, and the prevalence of these diseases in the United States exceeds 100,000 persons, placing MDS among the most common hematologic malignancies.25 The incidence of MDS rises sharply after the age of 70 years, and physician surveys indicate that the median age at diagnosis in the United States is approximately 70 to 72 years.26 The United States data described above are consistent with reports from other Western countries, including Germany, Sweden, the United Kingdom, and France.29–29 In contrast, Eastern European and Asian patients are significantly younger at the time of MDS diagnosis, and also present with different distributions of MDS subtypes, compared to patients in Western countries.30–33 This observation suggests that the natural history of MDS varies in different regions, either because of background genetics of the population or distinct environmental exposures. MDS are more common in men than in women, possibly related to past patterns of occupational exposures.19,20 However, a specific subtype of MDS associated with isolated deletion of the long arm of chromosome 5 [del(5q)] and marrow morphology, including hypolobated megakaryocytes, the so-called “5q− syndrome,” is more common in women than in men.34 Aging is by far the most important risk factor for development of MDS, likely because of the progressive accumulation of somatic mutations of hematopoietic stem cells across the human life span.35 Eventually, as such somatic mosaicism emerges, certain patterns of mutation may give hematopoietic cells a growth and survival advantage, and the expanded clone of cells is then at risk for acquiring additional mutations that augment its malignant potential.36 The risk of developing MDS is increased after exposure to organic solvents and hydrocarbons, including benzene, likely as a result of acceleration of DNA mutagenesis by such agents.39–39 Even low-level occupational benzene exposure has been associated with hematologic toxicity.38 Polymorphisms in DNA repair enzymes or of the detoxification enzyme NADPH : quinine oxidoreductase (NQO1) may alter patients’ sensitivity to DNA damaging chemicals.40,41 Other exposures that are encountered more commonly by the general population than benzene may also influence MDS risk.42 For instance, case-control studies suggest an increased risk of MDS in association with family history of hematopoietic cancer, tobacco smoking, and exposure to potentially harmful chemicals (i.e., agricultural chemicals, petroleum products, hair dyes or solvents), while higher educational attainment or moderate consumption of wine may be protective.43–46 Compared with de novo MDS, secondary MDS related to an occupational or environmental exposure is more closely associated with an abnormal karyotype.46 In general, families of patients with MDS can be reassured that their risk for developing MDS is minimally increased compared to the general population. However, rare cases of familial MDS and AML have been reported,47 particularly in patients with germline RUNX1 mutations, who usually have a prodrome of thrombocytopenia.48 A rare granulocyte colony-stimulating factor (G-CSF) receptor polymorphism (CSF3R gene) also may predispose affected persons to high-risk MDS.49 Germline mutations in CEBPA are another cause of hereditary AML (albeit usually without an MDS prodrome), underscoring the genetic heterogeneity of familial MDS and AML.50,51 In a few families, MDS or AML with monosomy 7 has been reported in multiple individuals in the absence of either phenotypic abnormalities or any history of hematologic disorders. The genetic cause for this is unknown, although childhood monosomy 7 mosaic syndrome predisposes to MDS.52 Other families with recurrent MDS/AML and still-mysterious genetics exhibit a distinct gene expression pattern in affected versus unaffected family members, particularly in genes encoding factors involved in signal transduction.53 Recently, germline mutations in the GATA2 transcription factor were described in association with MDS, monocytopenia, and a risk of mycobacterial infection or lymphedema (“MonoMAC syndrome”).54,55 MDS may be idiopathic and arise de novo, or may instead be secondary to a recognized exposure to a DNA-damaging agent.56–60 So-called secondary or therapy-related MDS (t-MDS) represents approximately 10% to 15% of MDS cases overall, and has a similar poor prognosis to secondary AML (t-AML), such that the WHO classes t-MDS and t-AML together as a single disorder.61 t-MDS/AML has been linked to several classes of exposure, which trigger disease via distinct genetic pathways.62 Common causes of t-MDS/AML include treatment with drugs that alkylate DNA bases (e.g., chlorambucil, melphalan, cyclophosphamide), therapeutic or accidental exposure to ionizing radiation, treatment with inhibitors of topoisomerase II (e.g., etoposide, or anthracyclines such as doxorubicin), or environmental or occupational exposure to other miscellaneous DNA toxins such as kerosene or benzene.46 Combined exposures, such as the combination of radiation therapy with chemotherapy (particularly with alkylating agents), increases the risk of t-MDS/AML compared with single exposures. MDS has also has been reported after exposure to fludarabine.63,64 MDS may rarely evolve from another hematologic disorder, particularly polycythemia vera after treatment with radiophosphorus or busulfan.65 Patients’ sensitivity to DNA damaging agents and inherent risk for t-MDS/AML after an exposure may vary. For instance, specific polymorphisms in the methylene tetrahydrofolate reductase (MTHFR) gene, encoding a protein critical for DNA synthesis, are associated with a higher risk of t-MDS/AML after treatment with cyclophosphamide, particularly in patients with breast cancer.66 The median latency period for t-MDS/AML after exposure to alkylating agents is 5 to 7 years, and the risk appears to be dose-dependent.67,68 In general, t-MDS/AML after alkylating agent or radiation exposure is characterized by deletions or unbalanced translocations, commonly involving chromosome 5 (particularly 5q31) or chromosome 7.69 By contrast, t-MDS or AML after exposure to topoisomerase inhibitors is distinct from that following alkylating agents in several ways: these cases are much less common than alkylating agent or radiation-induced t-MDS/AML; the latency period is shorter (median: 1 to 3 years); disease more frequently manifests with overt leukemia without a preceding MDS phase; a balanced translocation, often involving the MLL gene at 11q23 or the MECOM locus at 3q21q26, is more likely than chromosomal deletion or aneuploidy; and the complete response rate to antileukemia therapies may be higher, although the long-term prognosis is still poor.70,71 It can be challenging in some cases to prove a connection between a suspect exposure and subsequent development of MDS or AML, but the presence of a complex karyotype (i.e., three or more acquired chromosome abnormalities) or abnormalities of chromosomes 5 and 7 or 11q23 suggests t-MDS/AML. The predisposing exposure does not need to be recent. Even more than 50 years after the 1945 atomic weapon discharge over Nagasaki, for instance, the incidence of MDS continued to be higher in exposed persons than in unexposed controls.33 High-dose chemotherapy and autologous stem cell transplantation (SCT) represent a strong risk factor for subsequent development of t-MDS/AML. For instance, after autologous SCT for malignant lymphoma, the risk of t-MDS/AML at long-term follow-up in some series exceeds 10%, although the use of non–total-body irradiation-containing conditioning regimens may reduce this risk to some degree.72–76 The nature of pretransplantation therapy influences the risk of t-MDS/AML after autologous SCT.77,78 In one study, the risk of MDS after radioimmunotherapy with 131I tositumomab for lymphoma did not appear to be increased above the risk for those who had not received radioimmunotherapy.79 There is also a substantial risk of MDS after allogeneic SCT, but because the most common indications for allogeneic SCT in the United States are MDS and AML and related myeloid neoplasms, the contribution of the procedure itself to subsequent development of “t-MDS/AML” is often difficult to determine. However, cases of posttransplant “relapse” of MDS have been reported with different karyotypes from pretransplant disease, suggesting that they may represent a different (and in some cases donor-derived) dominant clone from the original disease.80 The use of G-CSF in children with congenital neutropenia may increase the incidence of secondary MDS and AML, but this remains controversial, because congenital neutropenia carries an inherent risk of MDS, and without the use of G-CSF many children would die of infection early in life and would not live long enough to develop MDS.83–83 Similarly, an increased incidence of t-MDS/AML was reported in studies of long-term maintenance therapy with lenalidomide for multiple myeloma, but again the causality is unclear, and lenalidomide may improve myeloma survival allowing more time for secondary neoplasms to develop.84 t-MDS/AML has also been reported as a complication following dose dense breast cancer therapy that includes G-CSF support.59 MDS are rare in children and represent only approximately 5% of hematologic malignancies in patients younger than age 18 years.85,86 When MDS do arise in children, they are usually either secondary to prior treatment of a neoplasm, or are associated with a congenital marrow failure syndrome or germline DNA repair defect, such as Li-Fraumeni syndrome (TP53 germline mutation), Shwachman-Bodian-Diamond syndrome (SBDS germline mutation), or Bloom syndrome (BLM1 germline mutation).87–91 Children with the marrow failure syndrome Fanconi anemia (>13 genes responsible) are at markedly increased risk of developing MDS, and because up to one-third of Fanconi anemia patients have no physical stigmata, the possibility of Fanconi anemia should be considered in all patients diagnosed with MDS before age 40 years without an obvious predisposing cause.89 Dyskeratosis congenita, a congenital marrow failure syndrome caused by germline mutations in genes encoding proteins responsible for telomere maintenance (e.g., DKC1, TERT and TERC), carries a higher risk of aplastic anemia than MDS, though acquired MDS often have altered telomere dynamics.90,92 Children who develop MDS without excess blasts but who appear to lack a predisposing congenital syndrome are provisionally classified by the WHO (see “Therapy: Immunosuppressive Therapy”) as having “refractory cytopenia of childhood” (MDS-RCC).93 Prognostic tools and classification systems useful for adult MDS often perform poorly in pediatric subgroups.96–96 The bone marrow in pediatric MDS is often hypocellular, rather than the hypercellular marrow typical in adults, and there is also a high incidence of unfavorable biological features such as monosomy 7 in childhood MDS.85 The MDS subtypes refractory anemia with ring sideroblasts (RARS) and 5q− syndrome are rare in children, but several types of congenital sideroblastic anemia can potentially be confused with MDS. These congenital syndromes include sideroblastic anemia caused by germline mutations of the X-linked gene ALAS2, which encodes the enzyme responsible for the first and rate-limiting step in heme biosynthesis. Germline ALAS2 mutations can also present late in life as a result of acquired skewing of X chromosome inactivation patterns and can be confused with RARS, but they do not carry a risk of progression to AML.97,98 Although historically there has been considerable confusion about the fundamental nature of MDS, since the WHO revised its classification of neoplastic disease in 1999, MDS have been clearly recognized as malignancies, that is, as forms of cancer.17,99 Hematopoiesis is clonal in MDS, and while clonality alone is not equivalent to malignancy, survival in patients with MDS is diminished compared with healthy controls, even in the lowest-risk cohorts.100 DNA damaging agents can predispose to MDS by accelerating mutation acquisition, and evolving idiopathic somatic mosaicism also puts patients at risk as described above, but the underlying cause of MDS is unknown in most cases, and there is no single unifying pathophysiology. Historically, MDS has been difficult to model in the laboratory, because there are no truly representative MDS cell lines and only a limited number of preclinical models—just a few recently constructed murine models, such as an NUP98-HOXD13 transgenic mouse and an interesting “stromal dysfunction” mouse that evolves an MDS-like syndrome after knockout of Dicer1 in osteoprogenitor cells rather than hematopoietic progenitors.101–104 Only in the present era of high-throughput resequencing has a clear picture of MDS pathogenesis and clonal architecture begun to emerge.16,105 Despite the limitations of a lack of cell line or preclinical models, a functional model of MDS molecular pathogenesis is suggested by the clinical behavior of the disease—namely, the progressive transformation of a committed myeloid hematopoietic stem cell with acquisition of successive genetic abnormalities, and clonal expansion, leading to the “classic” clinical phenotype (i.e., hypercellular bone marrow with increased angiogenesis and apoptosis, abnormal cytogenetics, cytopenias, and transformation to higher-risk forms of disease including frank AML).108–108 Intramedullary apoptosis mediated by death receptors and their ligands, such as tumor necrosis factor-α, Fas, or TRAIL (tumor necrosis factor-related apoptosis-inducing ligand), may help explain the “paradox of MDS,” in which a hypercellular marrow is associated with peripheral blood cytopenias.111–111 In the subset of patients with 5q− syndrome, global gene expression profiling and other experiments indicate a stem cell origin for the disease, and the clonal “leukemic” stem cells (sortable via their CD34+, CD38 absent or low, CD90+ expression pattern) persist during therapy with lenalidomide and serve as a nidus for relapse.112,113 It seems highly likely that a stem cell origin is also applicable for other MDS subtypes. The marrow microenvironment may harbor such stem cells in a protective niche and support perpetuation of disease, and the stromal cells may themselves be defective or mutated.102,114,115 Gene expression profiling experiments using complementary DNA microarray technology were the first high-throughput technique to demonstrate biological heterogeneity matching the clinical diversity of patients with MDS, but specific pathophysiological insights from gene expression profiling have been limited because of the difficulty in separating clones and in distinguishing primary “driver” and reactive “passenger” changes in gene expression.116–119 In patients with lower-risk MDS, array-based single-nucleotide polymorphism (SNP) analysis has demonstrated uniparental disomy and copy number changes, and the presence of such abnormalities in patients with a normal karyotype may portend a poorer prognosis.120–123 More recently, whole-genome DNA sequencing efforts focused on the architecture of hematopoiesis in MDS demonstrate that more than 80% of cells are clonal at the time of diagnosis and that in a darwinian process, clones compete for dominance in the marrow, with the hardiest clones surviving and ultimately contributing to leukemia.16 Most patients with MDS are now known to harbor multiple point mutations in coding regions of genes expressed in CD34+ cells at the time of diagnosis, and it seems likely that several mutations with complementary pathobiological function are required for the full clinical picture to emerge.15,28,124 Detection of the presence of these mutations can aid in clinical diagnosis in ambiguous cases.21 The first mutations described in MDS primary cells in 1987 were in the RAS G-protein–coupled signaling pathway.125,126 As of 2012, a quarter-century later, more than 25 different recurrent mutations are recognized, and several of these have prognostic significance independent of existing models.28 Common recurrent mutations (Table 99-2) involve factors important for cell proliferation such as receptor tyrosine kinases and their downstream mediators (e.g., NRAS, KRAS, BRAF, JAK2), pre–messenger RNA splicing (e.g., SF3B1, SRSF2, U2AF1), transcription and cell differentiation (e.g., RUNX1, WT1, PHF6), DNA damage repair (e.g., TP53), and especially epigenetic patterning (e.g., TET2, EZH2, DNMT3A, IDH1/2, ATRX).127–134 The functional consequences and details of interactions between these factors are only just beginning to be understood, and may depend on sequence of mutation acquisition and allele burden. Although a model of inactivation or mutation of tumor suppressor genes has been proposed as a contributor to MDS biology, and may account for the clinical response to DNA hypomethylating agents as described below, the principal tumor suppressors responsible for MDS, if they exist, have not yet been identified.135 Table 99-2 Somatic Mutations in Single Genes Detectable in MDS
Myelodysplastic Syndromes
Introduction
History and Terminology
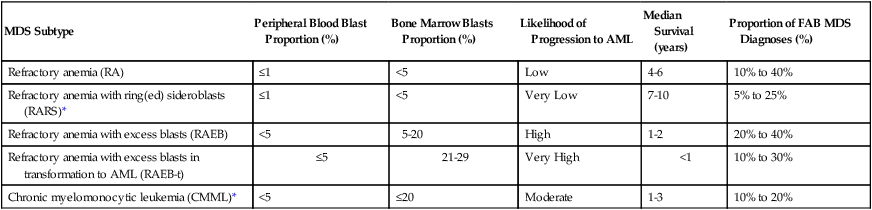
MDS Subtype
Peripheral Blood Blast Proportion (%)
Bone Marrow Blasts Proportion (%)
Likelihood of Progression to AML
Median Survival (years)
Proportion of FAB MDS Diagnoses (%)
Refractory anemia (RA)
≤1
<5
Low
4-6
10% to 40%
Refractory anemia with ring(ed) sideroblasts (RARS)*
≤1
<5
Very Low
7-10
5% to 25%
Refractory anemia with excess blasts (RAEB)
<5
5-20
High
1-2
20% to 40%
Refractory anemia with excess blasts in transformation to AML (RAEB-t)
≤5
21-29
Very High
<1
10% to 30%
Chronic myelomonocytic leukemia (CMML)*
<5
≤20
Moderate
1-3
10% to 20%
Epidemiology and Etiology
General Observations
Environmental and Occupational Exposures
Familial Myelodysplastic Syndromes
Therapy-Related Myelodysplastic Syndromes
Stem Cell Transplantation and Granulocyte Colony-Stimulating Factor Contributing to Myelodysplastic Syndromes
Pediatric Myelodysplastic Syndromes
Pathogenesis and Biology
Stem Cell Origin and Microenvironment
Expression Profiling and Point Mutations
Recurrently Mutated Genes
Mutation Frequency in MDS
Prognostic Impact
Additional Notes
PRE-MRNA SPLICING FACTORS (COMPONENTS OF THE SPLICEOSOME)
SF3B1
15% to 20%
Neutral to favorable
Strongly associated with the presence of ring sideroblasts (75% to 80% of RARS cases); often co-occurs with DNMT3A mutations
U2AF1
10% to 15%
Neutral to adverse
Often co-occurs with del(20q)
SRSF2
10% to 15%
Adverse
More frequent in CMML (25% to 30%), often co-occurs with RUNX1 or ASXL1 mutations
ZRSR2
5% to 10%
Neutral to adverse
U2AF2, SFRA1, PRPF40B, SF1
~5%
?
EPIGENETIC MODIFIERS (ALTER DNA METHYLATION OR HISTONE/CHROMATIN MODIFICATIONS)
TET2
20%
Neutral
More frequently observed in in CMML (~40%)
DNMT3A
10% to 15%
Adverse
In AML, is associated with lack of chemoresponsiveness
IDH1, IDH2
<5%
Variable
More frequent in AML than in MDS; when seen with NPM1 in AML, better prognosis
ASXL1
10% to 20%
Adverse
More frequent in CMML (~40%)
EZH2
6%
Adverse
More frequent in CMML (~12%)
KDM6A (UTX)
<1%
?
Rare in MDS, more frequent in CMML
PHF6
?
?
ATRX
Rare
?
Associated with acquired α−thalassemia and hemoglobin H inclusion bodies
TRANSCRIPTION FACTORS ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access