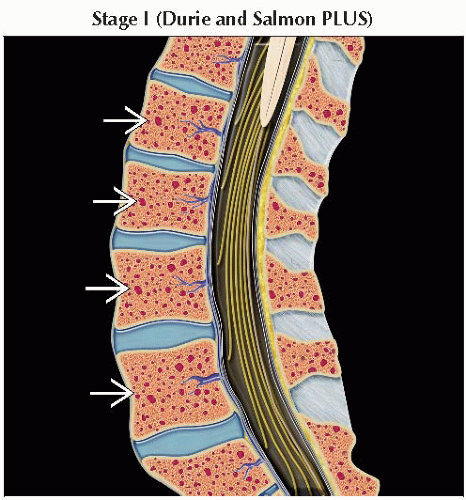
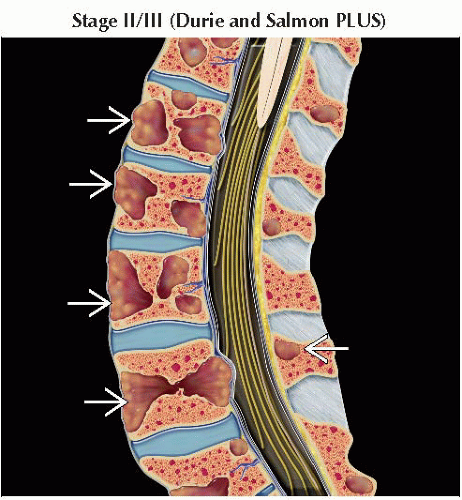
Durie and Salmon PLUS Staging System | ||||
Classification | Bone Marrow | Laboratory Parameters | Imaging Parameters1 | |
Monoclonal gammopathy of undetermined significance (MGUS): Not included in staging | < 10% plasma cells | No intra- or extramedullary disease | ||
Smoldering multiple myeloma (SMM): Stage IA2 | ≥ 10% plasma cells | All of the following: Hemoglobin > 10 g/dL; sCa++ ≤ 12 mg/dL; low M-component production; IgG < 5.0 g/dL; IgA < 3.0 g/dL; urine M-protein < 4g/24h | Limited disease (definition evolving) | |
Multiple myeloma (MM): Stages IB-III | ≥ 10% plasma cells &/or plasmacytoma + end organ damage3 | Variable by stage | Variable by stage | |
Stage IB2 | Same as stage IA | |||
Stage IIA/B2 | Neither stage I nor stage III | |||
Stage IIIA/B2 | 1 or more of the following: > Hemoglobin < 8.5 g/dL; sCa++ > 12 mg/dL; IgG > 7.0 g/dL; IgA > 5.0 g/dL; urine M-protein > 12g/24h | |||
1 The imaging appearance of bone marrow is variable. Patients with stage III myeloma by clinical criteria can have a normal MR appearance of bone marrow, which is associated with a more favorable prognosis. | ||||
International Staging System | |
Stage | Criteria |
I | Serum β2-microglobulin < 3.5 mg/L |
Serum albumin ≥ 3.5 g/dL | |
II | Not stage I or III |
III | Serum β2-microglobulin ≥ 5.5 mg/L |
The International Staging System is useful in imaging facilities without advanced imaging with MR or PET and as a measure of survival. Median survival for stage I: 62 months; stage II: 44 months; stage III: 29 months. | |
Heterogeneous plasma cell (PC) disorder
Characterized by bone marrow (BM) infiltration
Diagnosed by combination of blood tests, BM biopsy and aspirate, urine protein studies, and x-rays
Chemotherapy improves survival but is not curative unless an allogeneic transplant is performed
Based on increasing malignant potential
Monoclonal gammopathy (MG) of undetermined significance (MGUS)
Progression risk → multiple myeloma (MM) = 1% per year
< 3 g/dL serum M-protein & < 10% BM PCs
When progression occurs, it usually leads to MM or Waldenström macroglobulinemia
Potentially can also progress to
Primary amyloidosis
Chronic lymphocytic leukemia
Lymphoma
MG of borderline significance (MGBS)
Subclassification (not universally used)
Higher risk of progression to MM than MGUS
Difference = ↑ PC number in BM (10-30% for MGBS vs. < 10% for MGUS)
Smoldering multiple myeloma (SMM)
≥ 3g/dL serum M-protein & ≥10% BM PCs
No end organ damage (EOD) (asymptomatic)
Higher risk of progression to MM
Multiple myeloma
Symptomatic: EOD present
EOD includes any of the following (CRAB)
Calcium elevation
Renal insufficiency
Anemia
Bone abnormalities (lytic or osteopenic)
Nonsecretory
No elevated M-protein in urine or blood
Disease best followed by PET/CT
POEMS syndrome
Polyneuropathy, organomegaly, endocrinopathy, m-protein, skin changes
Sclerotic bone lesions
PC leukemia is characterized by > 20% circulating PCs at any time
Comments
Disorder with abnormal proliferation of BM PCs
Aggressiveness varies 2° to genetic alterations in PCs
Plasmacytoma generally refers to solitary lesion
Receptor activator of nuclear factor-κB ligand (RANKL) activates osteoclasts → bone resorption → hypercalcemia
Location
Bone marrow
Extramedullary plasmacytomas most commonly occur in upper respiratory tract
Unknown
Exposure to herbicides, insecticides, benzene, and ionizing radiation may contribute
Number of cases in USA per year
21,700 estimated new cases in 2012 with 10,710 deaths
Sex predilection
M>F
Most common primary bone malignancy
10% of all hematologic malignancies
2x ↑ incidence for African-Americans
Common translocations
Chromosomal abnormalities of 14 and 13 seen (˜ 50% of cases each)
Rarely hereditary
Multiple PC genetic subclassifications
Poor prognostic factors
Del chromosome (chr) 13 → retinoblastoma-1 (RB1) mutation
↑ PC proliferation index
Del chr 17p13 → inactivation of p53 tumor suppressor gene
t(4;14) → upregulation of fibroblast growth factor (FGF) receptor 3
t(14;16) → upregulation of MAF transcription factor
Neutral/favorable prognostic factors
Absence of poor prognostic factors, plus 1 of the following
t(11;14) → upregulation of cyclin D1
t(6;14) → upregulation of cyclin D3
Hyperdiploidy
Myelofibrosis
Fanconi syndrome type II (renal tubular acidosis)
Focal or widespread BM infiltration by genetically altered PCs
Focal extramedullary disease is termed plasmacytoma
H&E
% of BM PCs important for classification of MM
BM analysis: May be subject to sampling error
Aspirate can underestimate or overestimate number of PCs
BM biopsy more accurate
Special stains
Wright-Giemsa considered superior
CD138 immunohistochemistry most accurate
Typically positive for CD56, CD38, and CD138 and negative for CD19 and CD45
Solitary plasmacytoma
Detected via biopsy of solitary lesion
MR or FDG PET/CT used to exclude systemic disease
Radiographic skeletal survey (RSS)
20% of patients with normal axial MR showed extremity lesions by RSS
More sensitive than bone scan in 38%
Lytic lesions (< 5, 5-20, > 20) or osteopenia
Number of lytic lesions is important for staging
If RSS without lytic lesions
Whole-body MR vs. MR spine/pelvis
If no MR, FDG PET/CT preferred over CT alone
Bone scan
Insensitive for MM; of limited usefulness
CT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree