Lymphatic mapping and sentinel lymph node (SLN) biopsy have become the standard of care for staging the axilla in patients with invasive breast cancer. Current histologic methods for SLN evaluation have limitations, including subjectivity, limited sensitivity, and lack of standardization. The discovery of molecular markers to detect metastases has been reported over the last 2 decades. The authors review the historical development of these markers and the clinical use of one of the molecular platforms in 478 patients at their institution. Controversies and future directions are discussed.
Development and use of sentinel lymph node staging in breast cancer
The presence of metastatic disease in the axillary lymph nodes (ALNs) of patients with breast cancer has long been considered the most important prognostic factor for patients with newly diagnosed breast cancer. The standard use of ALN dissection (ALND) has been to provide staging and prognostic information, as well as local control.
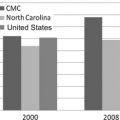
With vastly improved imaging techniques, primary breast cancer is being diagnosed earlier, at a smaller size, and with lower risk of having disease in the axilla. At present, approximately 24% of patients have positive nodes; therefore, the remainder derive no benefit from ALND.
The development of lymphatic mapping and selective sentinel lymph node (SLN) lymphadenectomy has allowed many patients to be spared the sequelae of a full ALND, which would provide no therapeutic benefit but risk numerous side effects, including lymphedema, dysesthesias, and discomfort.
Two major prospective studies as to the feasibility and accuracy of breast SLN biopsy were performed in National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32 and the American College of Surgeons Oncology Group (ACOSOG) Z0010 trials. These trials encouraged the participation of community cancer centers such as the Morton Plant Hospital, thus providing the opportunity for community surgeons around the country to partner with their academic colleagues in major national trials. In Z0010, 29% of patients were enrolled from community practices. SLN biopsy can identify for the pathologist those nodes most likely to contain metastases. These few nodes can undergo a more thorough and labor-intensive analysis; however, there is no standardized protocol. It is commonly accepted that more sampling leads to an upstaging of the nodes ( Table 1 ), but evaluation is also subjective with interpretive disparity even among expert pathologists.
| Author, Year | Increased H&E Cutting | Increase of Metastases Found (%) |
|---|---|---|
| Treseler & Tauchi, 2000 | Multistudy summary | 9–33 |
| Yared et al, 2002 | One 5-μm level vs ten 5-μm levels | 10 |
| Liu et al, 2000 | 1 level vs 3 additional H&E plus IHC | 19 |
| Cserni, 2002 | Five 5-μm levels (at 50–100 μm apart) vs complete node sectioning at 250 μm | 19–28 |
| Pargaonkar et al, 2003 | One 5-μm level vs 2 H&E and 3 IHC 5-μm levels | 8 |
| Motomura et al, 2002 | One 5 μm per node vs 1 level of H&E per 2 mm of node/additional H&E level plus IHC | 3/16 |
| Groen et al, 2007 | 1 level per node half vs 3 levels, 150 μm apart per node half | 12.5 |
Controversy also exists as to what size metastasis in a breast sentinel node is significant. The American Joint Committee on Cancer manual for cancer staging divides lymph node positivity into macrometastases 2 mm or greater, micrometastases 0.2 to less than 2 mm, and isolated tumor cells (ITCs). There is a relationship between the volume of disease in an SLN and the incidence of further axillary metastases ( Table 2 ). The general standard of care has been to complete an ALND for most patients with a positive SLN. If the SLN status can be determined intraoperatively, the surgeon can complete the ALND at the time of the first surgery.
| Size of SLN Metastasis | Incidence of Further Axillary Metastases (%) |
|---|---|
| >2 mm macrometastases | 45–79 |
| 0.2 and <2 mm micrometastases | 10–25 |
| <0.2 mm submicrometastases | 7–15 |
| Negative | ∼10 |
Current histologic methods for SLN evaluation have limitations. Histologic analysis on permanent section (PS) with hematoxylin and eosin (H&E) stain requires fixed tissue. This method is time consuming but allows high-quality morphologic analysis. PS has high specificity (99%–100%) and high sensitivity (85%–90%), but the latter depends on sampling thoroughness. Morphology is available, and size of metastases can be estimated. Unfortunately, there is no standard method for SLN processing and PS analysis. It is generally impractical to extensively sample each node for high sensitivity: usual methods examine only 2% to 5% of each node. PS is not intraoperative, and turnaround times vary greatly among different institutions. Histologic analysis requires an experienced pathologist, yet it still remains subjective. There are limitations identifying certain cancers such as lobular cell type. Immunohistochemistry (IHC) can be used in some cases to supplement PS analysis, especially to better identify cells expressing epithelial markers such as cytokeratins. However, IHC is not universally adopted, and there is no consensus as to its clinical significance.
Intraoperative methods for SLN evaluation include frozen section (FS) and touch imprint cytology (TIC). FS has moderate sensitivity (57%–74%) with high specificity (99%–100%) ( Table 3 ). There is some morphologic information available and a rough estimate of the size of metastases. FS is usually available in 10 to 30 minutes intraoperatively. Again, there is no standard method for FS. It lacks higher sensitivity because sampling is limited, staining is less distinct, interpretation is even more subjective than PS, and certain cancers are difficult to identify, for example, lobular cancer. Other drawbacks of FS are loss of tissue in the microtome and freezing artifact on later PS analysis.
| Author, Year | Number of Cases | Method | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Veronesi et al, 1997 Rahusen et al, 2000 Chao et al, 2002 Tanis et al, 2001 | 107 106 203 262 | Frozen section | 64 57 68 74 | 100 100 99 99 |
| Creager, 2002 Dabbs, 2004 Guldroz, 2010 | 646 748 387 | Touch preparation | 53 45 63 | 98 99 99 |
| Komenaka, 2010 | 107 | Frozen section Touch preparation | 74 61 | 100 100 |
Like FS, TIC also has moderate sensitivity (45%–63%) with high specificity (98%–100%) (see Table 3 ). There is no loss of tissue, and a 10- to 30-minute turnaround time allows intraoperative use. There is no standard method for TIC, and extensive sampling is not practical. TIC requires an expert cytopathologist, is subjective, is limited with the lobular subtype, and provides no size estimate. In a meta-analysis of sentinel node TIC in breast cancer by Tew and colleagues, 31 studies were included, with a pooled sensitivity of 63% (95% confidence interval [CI], 57%–69%) and a specificity of 99% (95% CI, 98%–99%). Patients with invasive lobular cancer or micrometastases are more likely to have a false-negative finding.
The less-than-optimal sensitivity and the wide performance variability of current intraoperative methods for SLN evaluation often result in a delayed diagnosis and the need for a second surgery to perform ALND. The need for a more accurate intraoperative test, as well as a more objective, more reproducible, and less time-consuming postoperative test has spurred several investigations in the field of molecular analysis of SLNs.
Development of molecular markers for SLN staging—a historical perspective
Molecular analysis of breast SLNs emerged in the scientific and clinical literature in the late 1990s with many research studies initially focused on identifying suitable molecular markers for metastatic disease. Molecular analysis of the SLN consists of studying gene expression at the messenger RNA (mRNA) level. Although the DNA of all genes is present in all cell types, only a few genes are expressed in any specific cell type with discrete production of mRNA and proteins. Theoretically, the detection of mRNA from genes not normally expressed in the lymph nodes indicates the presence of breast-derived cells or metastases.
Molecular analysis of the SLN involves extracting and purifying total mRNA from the homogenized lymph node followed by measuring mRNA levels of designated genes. Reverse transcription polymerase chain reaction (RT-PCR) produces a large number of copies of the chosen mRNA in vitro, which are then detected by gel electrophoresis (conventional RT-PCR) or by fluorescence measurement (real-time RT-PCR).
In general, molecular analysis has the potential to be more objective and reproducible than histologic analysis, as measuring gene expression is inherently less subjective than analyzing the morphology of cells. Because the entire node submitted is evaluated through the homogenization technique, molecular analysis evaluates more nodal tissue than typical histologic analysis, either intraoperatively or postoperatively.
In 1994, Schoenfeld and colleagues found that the cytokeratin 19 (CK19) gene was a good discriminator differentiating those lymph nodes involved by breast cancer metastasis. Their analysis, which involved the lengthy process of RT-PCR followed by gel electrophoresis and hybridization, revealed superior sensitivity compared with the IHC analysis of CK19. Noguchi and colleagues found that RT-PCR of the MUC1 and CK19 genes in an experimental setting allowed identification of 1 in 10 5 and 1 in 10 6 cancer cells, respectively. Using RT-PCR for MUC1 and CK19 to study pooled ALNs from 56 patients, gene expression was detected in 7 of the histologically negative patients and not detected in 1 histologically positive patient.
Both these initial studies as well as others showed that molecular analysis could achieve higher sensitivity than histologic analysis. In light of this higher sensitivity, the realization that some level of expression of the genes chosen for molecular analysis could be present in normal lymph node cells raised concern about potential false-positive results.
The melanoma-associated antigen 3 (MAGE-A3) marker sought to solve the specificity issue because this breast cancer gene is not expressed in any normal tissue. However, in the analysis by Wascher and colleagues, only 45% of the histologically positive lymph nodes demonstrated MAGE-A3 expression. Therefore, although the specificity of this marker is potentially high, its low sensitivity precluded its further development into a clinical marker. Unfortunately, no specific marker for metastatic breast cancer has been reported to date.
In 2001, Manzotti and colleagues evaluated 5 different genes in 146 SLNs from 123 patients and compared their expression with an extensive histologic analysis, which included 15 pairs of FS cut at 50- or 100-μm intervals for the entire length of the lymph node. Molecular analysis was performed on the intervening tissue slabs not used for histologic analysis. The sensitivity and specificity of the various markers varied, with MUC1 showing the highest specificity (100%) but the lowest sensitivity and mammoglobin (MG) showing the best combination of sensitivity (77.8%) and specificity (86%). The investigators concluded that the use of a multiple-marker RT-PCR assay had high concordance with an extensive histologic analysis. However, it was determined that further clinical follow-up of the patients was necessary to understand the full clinical implications of the molecular analysis.
All the molecular studies referenced up to this point used conventional RT-PCR. These studies often involved the use of nested PCR or a very large number of PCR cycles to improve sensitivity. These approaches have an inherent risk of contamination and only provide a qualitative analysis. The increasing use of real-time PCR in many laboratories in the early 2000s led to the development of more reproducible and quantitative assays. Real-time RT-PCR uses a closed tube system, reducing the risk of contamination. Real-time RT-PCR is quantitative and can discriminate between normal baseline gene expression and abnormally elevated gene expression such as found in the presence of metastases. Standardization of real-time PCR analyses can be accomplished by setting fixed analysis parameters and predetermined cutoffs.
In 2003, Inokuchi and colleagues studied 358 ALNs from 22 patients using real-time RT-PCR. The expression of CK19 was compared with that of a normally expressed control gene. Cutoff values were first established by comparing the relative expression of CK19 in normal versus histologically positive lymph nodes. Using this method, 100% of the histologically positive and 9% of the histologically negative lymph nodes were positive by RT-PCR; furthermore, 3 of 4 histologically negative but IHC-positive nodes were positive by RT-PCR. This and other similar studies started to highlight the potential for the use of real-time PCR in the molecular analysis of SLNs, as this method is less cumbersome than extensive sectioning of the node and can provide reproducible and quantifiable data.
Gillanders and colleagues and Mikhitarian and colleagues reported the findings of the MIMS (Minimally Invasive Molecular Staging of Breast Cancer) trial, a multi-institutional cohort study, where multimarker real-time RT-PCR analysis was applied to the analysis of SLNs and nonsentinel ALNs from 489 patients. The final report shows that the sensitivity of the combined pathologic and molecular SLN analysis to predict the metastatic status of ALNs was 92.8% compared with 84% for the pathologic analysis alone. The investigators also recognized the potential to tailor the molecular analysis so that the cutoff for positivity approximates the sensitivity of routine pathologic analysis or IHC.
Another important aspect of real-time molecular assays is their suitability for intraoperative use because of the extreme speed of this type of PCR. Raja and colleagues and Hughes and colleagues reported the development of a completely automated cartridge-based molecular assay using the GeneXpert system in collaboration with the diagnostic company Cepheid (Sunnyvale, CA, USA). With this system, the cartridge is capable of performing nucleic acid isolation starting from a filtered lysate containing the SLN tissue. The cartridge, using lyophilized reagents and a microfluidics system, can automatically perform all the steps necessary for real-time RT-PCR and detection. The markers used in this system are 2 target genes (TACSTD1 and PIP) and an endogenous control gene. In their latest article, the investigators report on the reproducibility studies performed at 3 different sites, as well as data for 29 positive and 30 negative control lymph nodes. Although the technical characteristics of this system are extremely intriguing, including the use of the bidirectional multiplexing strategy, it is unclear if any clinical studies have been initiated with this method.
In 2007, Tsujimoto and colleagues reported the application of a novel assay, termed OSNA (one-step nucleic acid amplification), for the detection and quantitative measurement of CK19 mRNA in breast cancer lymph nodes. OSNA is based on a technology developed in 2000 called reverse transcription loop-mediated isothermal amplification. With the OSNA assay, the lymph node tissue is solubilized and CK19 mRNA amplified without an intervening nucleic acid purification step. Amplification produces magnesium pyrophosphate, which is measured by turbidity. These features make OSNA a fast, simple technology that lends itself well to intraoperative use. The article by Tsujimoto and colleagues reports the establishment of cutoff values to distinguish macrometastases, micrometastases, and nonmetastases. The analysis for cutoff calculations was based on PS and IHC performed on serial frozen sections taken at 10-μm intervals and OSNA performed on alternating node sections. Macrometastases had CK19 expression greater than 5 × 10 3 copies/μL, micrometastases had from 2.5 × 10 2 to 5 × 10 3 copies/μL, and nonmetastases had fewer than 2.5 × 10 2 copies/μL. Clinical validation studies to address the performance of OSNA compared with 3-level histopathologic analysis reported an overall 98% concordance in the 2007 article and 93% concordance in a 2009 article by Tamaki and colleagues. Despite the use of only 1 molecular marker and no internal control gene, Tamaki and colleagues reported a specificity of 94.3% and a sensitivity of 87.7% in a multi-institutional trial involving 164 patients in Japan. Visser and colleagues evaluated OSNA in a study performed in the Netherlands on 32 patients and reported a sensitivity and specificity of 95.3% and 94.7%, respectively. Similar results were reported by Schem and colleagues in 2009 in a German study. A 2-year prospective clinical study of OSNA was conducted in the United States from 2007 to 2008, and the results have been presented by Feldman at the American Society of Breast Surgeons meeting in 2010. Results from 11 clinical sites evaluating 496 patients and 1044 SLNs showed an overall agreement between OSNA and reference pathology of 93.4% and 95.8% before and after discordant analysis, respectively. Sensitivity and specificity were 82.7% and 97.7%, respectively, after discordant analysis. Advantages of OSNA are its extreme speed and relative simplicity; the major disadvantage is that metastases of tumors not expressing CK19 are undetectable with this assay. OSNA indirectly allows the distinction between micrometastases and macrometastases, as the result of the test is reported as calculated CK19 copy number. This distinction potentially allows the surgeon to make an intraoperative decision regarding the performance of an ALND based on the size of the metastasis. The OSNA assay has received in vitro diagnostic product approval in Europe (CE mark) and in Asia and is commercially available through Sysmex (Mundelein, IL, USA).
Before the clinical development of the OSNA assay, Backus and colleagues reported their investigation to identify optimal gene expression markers for breast cancer metastasis in SLN. This study is the basis for the development of the first US Food and Drug Administration (FDA)-approved assay commercially available in the United States: the GeneSearch Breast Lymph Node (BLN) Assay (Veridex, LLC, Warren, NJ, USA). The initial investigation involved a genome-wide gene expression analysis, as well as the study of 7 putative breast-specific markers and 1 internal control gene. After testing various marker combinations on histologically positive and negative lymph nodes, the investigators concluded that the gene pair with the highest sensitivity, at a specificity of 94%, was CK19 and MG. Porphobilinogen deaminase (PBGD) was chosen as the internal control gene because of its constant level of expression in lymph nodes.
A large multi-institutional clinical trial sponsored by Veridex followed this initial study and was performed between July 2004 and December 2005. The trial consisted of 2 separate clinical studies: the first included 304 patients at 12 US sites and determined the appropriate cutoff levels for CK19 and MG; the second included 416 patients at 11 US sites for the clinical validation of the assay. The Morton Plant Hospital participated in both studies, with the largest number of patients recruited and investigated at this site. These data have been published in detail previously and are briefly reviewed here.
One of the major challenges of any molecular study of SLN is the appropriate calibration of the assay so that it does not detect clinically insignificant disease. For the BLN assay, the RT-PCR cutoffs were chosen so that micrometastases less than 0.2 mm would not yield positive results. Another challenge in the critical analysis of any molecular assay, including BLN, is that the tissue dedicated to molecular analysis is homogenized and therefore cannot be further analyzed morphologically. Any comparison between molecular and histologic analysis is therefore indirect, as it is performed on adjacent but not identical tissue portions. For the studies that led to the FDA approval of the BLN assay, PS analysis was considered the gold standard. To try to minimize sampling error, each node was sliced along the short axis into an even number of slabs 1.5 to 3 mm thick. The slabs used for histopathologic analysis were processed with PS, FS, or TIC as was standard at each institution and were used for patient management at each site. In addition, 3 extra PS slides were made from each tissue slab and were evaluated at a central pathology site; these slides consisted of three 4- to 6-μm thick sections collected at 3 levels, 150 μm apart.
In the validation series of 416 patients, when compared with PS, the assay detected 98% of metastases greater than 2 mm and 88% of metastases greater than 0.2 mm. Micrometastases were less frequently detected (57%), and assay-positive results in nodes found negative by histology were rare (4%). Disagreements seen between PS histology performed on adjacent node slabs and the molecular assay results were similar to the disagreements seen between histology performed on site slides versus central slides. Positive results of tests using additional molecular markers on nodes with positive BLN but overall negative histologic findings suggest that discrepancies were more likely due to sampling differences rather than to a false-positive result on BLN assay. In summary, the studies showed that BLN appeared to be a properly calibrated intraoperative molecular test that approaches the results obtained from PS histology. Compared with FS intraoperative testing, the assay showed improved sensitivity ranging from 10% to approximately 30%. In cases of invasive lobular carcinoma, FS sensitivity was 65.2% with a specificity of 97.8%, but the assay was 91.3% sensitive with a specificity of 95.7% (71 cases).
On July 17, 2007, the BLN assay received approval for clinical use from the FDA. The assay was labeled as a qualitative in vitro diagnostic test for the rapid detection of greater than 0.2 mm metastasis in nodal tissue removed from the sentinel node biopsies of breast cancer patients. Results from the assay could be used to guide intraoperative or postoperative decision making regarding removal of additional lymph nodes. The clinical use of the molecular assay began at Morton Plant Hospital on July 31, 2007. Analysis of that clinical use follows.
Development of molecular markers for SLN staging—a historical perspective
Molecular analysis of breast SLNs emerged in the scientific and clinical literature in the late 1990s with many research studies initially focused on identifying suitable molecular markers for metastatic disease. Molecular analysis of the SLN consists of studying gene expression at the messenger RNA (mRNA) level. Although the DNA of all genes is present in all cell types, only a few genes are expressed in any specific cell type with discrete production of mRNA and proteins. Theoretically, the detection of mRNA from genes not normally expressed in the lymph nodes indicates the presence of breast-derived cells or metastases.
Molecular analysis of the SLN involves extracting and purifying total mRNA from the homogenized lymph node followed by measuring mRNA levels of designated genes. Reverse transcription polymerase chain reaction (RT-PCR) produces a large number of copies of the chosen mRNA in vitro, which are then detected by gel electrophoresis (conventional RT-PCR) or by fluorescence measurement (real-time RT-PCR).
In general, molecular analysis has the potential to be more objective and reproducible than histologic analysis, as measuring gene expression is inherently less subjective than analyzing the morphology of cells. Because the entire node submitted is evaluated through the homogenization technique, molecular analysis evaluates more nodal tissue than typical histologic analysis, either intraoperatively or postoperatively.
In 1994, Schoenfeld and colleagues found that the cytokeratin 19 (CK19) gene was a good discriminator differentiating those lymph nodes involved by breast cancer metastasis. Their analysis, which involved the lengthy process of RT-PCR followed by gel electrophoresis and hybridization, revealed superior sensitivity compared with the IHC analysis of CK19. Noguchi and colleagues found that RT-PCR of the MUC1 and CK19 genes in an experimental setting allowed identification of 1 in 10 5 and 1 in 10 6 cancer cells, respectively. Using RT-PCR for MUC1 and CK19 to study pooled ALNs from 56 patients, gene expression was detected in 7 of the histologically negative patients and not detected in 1 histologically positive patient.
Both these initial studies as well as others showed that molecular analysis could achieve higher sensitivity than histologic analysis. In light of this higher sensitivity, the realization that some level of expression of the genes chosen for molecular analysis could be present in normal lymph node cells raised concern about potential false-positive results.
The melanoma-associated antigen 3 (MAGE-A3) marker sought to solve the specificity issue because this breast cancer gene is not expressed in any normal tissue. However, in the analysis by Wascher and colleagues, only 45% of the histologically positive lymph nodes demonstrated MAGE-A3 expression. Therefore, although the specificity of this marker is potentially high, its low sensitivity precluded its further development into a clinical marker. Unfortunately, no specific marker for metastatic breast cancer has been reported to date.
In 2001, Manzotti and colleagues evaluated 5 different genes in 146 SLNs from 123 patients and compared their expression with an extensive histologic analysis, which included 15 pairs of FS cut at 50- or 100-μm intervals for the entire length of the lymph node. Molecular analysis was performed on the intervening tissue slabs not used for histologic analysis. The sensitivity and specificity of the various markers varied, with MUC1 showing the highest specificity (100%) but the lowest sensitivity and mammoglobin (MG) showing the best combination of sensitivity (77.8%) and specificity (86%). The investigators concluded that the use of a multiple-marker RT-PCR assay had high concordance with an extensive histologic analysis. However, it was determined that further clinical follow-up of the patients was necessary to understand the full clinical implications of the molecular analysis.
All the molecular studies referenced up to this point used conventional RT-PCR. These studies often involved the use of nested PCR or a very large number of PCR cycles to improve sensitivity. These approaches have an inherent risk of contamination and only provide a qualitative analysis. The increasing use of real-time PCR in many laboratories in the early 2000s led to the development of more reproducible and quantitative assays. Real-time RT-PCR uses a closed tube system, reducing the risk of contamination. Real-time RT-PCR is quantitative and can discriminate between normal baseline gene expression and abnormally elevated gene expression such as found in the presence of metastases. Standardization of real-time PCR analyses can be accomplished by setting fixed analysis parameters and predetermined cutoffs.
In 2003, Inokuchi and colleagues studied 358 ALNs from 22 patients using real-time RT-PCR. The expression of CK19 was compared with that of a normally expressed control gene. Cutoff values were first established by comparing the relative expression of CK19 in normal versus histologically positive lymph nodes. Using this method, 100% of the histologically positive and 9% of the histologically negative lymph nodes were positive by RT-PCR; furthermore, 3 of 4 histologically negative but IHC-positive nodes were positive by RT-PCR. This and other similar studies started to highlight the potential for the use of real-time PCR in the molecular analysis of SLNs, as this method is less cumbersome than extensive sectioning of the node and can provide reproducible and quantifiable data.
Gillanders and colleagues and Mikhitarian and colleagues reported the findings of the MIMS (Minimally Invasive Molecular Staging of Breast Cancer) trial, a multi-institutional cohort study, where multimarker real-time RT-PCR analysis was applied to the analysis of SLNs and nonsentinel ALNs from 489 patients. The final report shows that the sensitivity of the combined pathologic and molecular SLN analysis to predict the metastatic status of ALNs was 92.8% compared with 84% for the pathologic analysis alone. The investigators also recognized the potential to tailor the molecular analysis so that the cutoff for positivity approximates the sensitivity of routine pathologic analysis or IHC.
Another important aspect of real-time molecular assays is their suitability for intraoperative use because of the extreme speed of this type of PCR. Raja and colleagues and Hughes and colleagues reported the development of a completely automated cartridge-based molecular assay using the GeneXpert system in collaboration with the diagnostic company Cepheid (Sunnyvale, CA, USA). With this system, the cartridge is capable of performing nucleic acid isolation starting from a filtered lysate containing the SLN tissue. The cartridge, using lyophilized reagents and a microfluidics system, can automatically perform all the steps necessary for real-time RT-PCR and detection. The markers used in this system are 2 target genes (TACSTD1 and PIP) and an endogenous control gene. In their latest article, the investigators report on the reproducibility studies performed at 3 different sites, as well as data for 29 positive and 30 negative control lymph nodes. Although the technical characteristics of this system are extremely intriguing, including the use of the bidirectional multiplexing strategy, it is unclear if any clinical studies have been initiated with this method.
In 2007, Tsujimoto and colleagues reported the application of a novel assay, termed OSNA (one-step nucleic acid amplification), for the detection and quantitative measurement of CK19 mRNA in breast cancer lymph nodes. OSNA is based on a technology developed in 2000 called reverse transcription loop-mediated isothermal amplification. With the OSNA assay, the lymph node tissue is solubilized and CK19 mRNA amplified without an intervening nucleic acid purification step. Amplification produces magnesium pyrophosphate, which is measured by turbidity. These features make OSNA a fast, simple technology that lends itself well to intraoperative use. The article by Tsujimoto and colleagues reports the establishment of cutoff values to distinguish macrometastases, micrometastases, and nonmetastases. The analysis for cutoff calculations was based on PS and IHC performed on serial frozen sections taken at 10-μm intervals and OSNA performed on alternating node sections. Macrometastases had CK19 expression greater than 5 × 10 3 copies/μL, micrometastases had from 2.5 × 10 2 to 5 × 10 3 copies/μL, and nonmetastases had fewer than 2.5 × 10 2 copies/μL. Clinical validation studies to address the performance of OSNA compared with 3-level histopathologic analysis reported an overall 98% concordance in the 2007 article and 93% concordance in a 2009 article by Tamaki and colleagues. Despite the use of only 1 molecular marker and no internal control gene, Tamaki and colleagues reported a specificity of 94.3% and a sensitivity of 87.7% in a multi-institutional trial involving 164 patients in Japan. Visser and colleagues evaluated OSNA in a study performed in the Netherlands on 32 patients and reported a sensitivity and specificity of 95.3% and 94.7%, respectively. Similar results were reported by Schem and colleagues in 2009 in a German study. A 2-year prospective clinical study of OSNA was conducted in the United States from 2007 to 2008, and the results have been presented by Feldman at the American Society of Breast Surgeons meeting in 2010. Results from 11 clinical sites evaluating 496 patients and 1044 SLNs showed an overall agreement between OSNA and reference pathology of 93.4% and 95.8% before and after discordant analysis, respectively. Sensitivity and specificity were 82.7% and 97.7%, respectively, after discordant analysis. Advantages of OSNA are its extreme speed and relative simplicity; the major disadvantage is that metastases of tumors not expressing CK19 are undetectable with this assay. OSNA indirectly allows the distinction between micrometastases and macrometastases, as the result of the test is reported as calculated CK19 copy number. This distinction potentially allows the surgeon to make an intraoperative decision regarding the performance of an ALND based on the size of the metastasis. The OSNA assay has received in vitro diagnostic product approval in Europe (CE mark) and in Asia and is commercially available through Sysmex (Mundelein, IL, USA).
Before the clinical development of the OSNA assay, Backus and colleagues reported their investigation to identify optimal gene expression markers for breast cancer metastasis in SLN. This study is the basis for the development of the first US Food and Drug Administration (FDA)-approved assay commercially available in the United States: the GeneSearch Breast Lymph Node (BLN) Assay (Veridex, LLC, Warren, NJ, USA). The initial investigation involved a genome-wide gene expression analysis, as well as the study of 7 putative breast-specific markers and 1 internal control gene. After testing various marker combinations on histologically positive and negative lymph nodes, the investigators concluded that the gene pair with the highest sensitivity, at a specificity of 94%, was CK19 and MG. Porphobilinogen deaminase (PBGD) was chosen as the internal control gene because of its constant level of expression in lymph nodes.
A large multi-institutional clinical trial sponsored by Veridex followed this initial study and was performed between July 2004 and December 2005. The trial consisted of 2 separate clinical studies: the first included 304 patients at 12 US sites and determined the appropriate cutoff levels for CK19 and MG; the second included 416 patients at 11 US sites for the clinical validation of the assay. The Morton Plant Hospital participated in both studies, with the largest number of patients recruited and investigated at this site. These data have been published in detail previously and are briefly reviewed here.
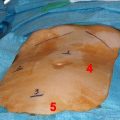
One of the major challenges of any molecular study of SLN is the appropriate calibration of the assay so that it does not detect clinically insignificant disease. For the BLN assay, the RT-PCR cutoffs were chosen so that micrometastases less than 0.2 mm would not yield positive results. Another challenge in the critical analysis of any molecular assay, including BLN, is that the tissue dedicated to molecular analysis is homogenized and therefore cannot be further analyzed morphologically. Any comparison between molecular and histologic analysis is therefore indirect, as it is performed on adjacent but not identical tissue portions. For the studies that led to the FDA approval of the BLN assay, PS analysis was considered the gold standard. To try to minimize sampling error, each node was sliced along the short axis into an even number of slabs 1.5 to 3 mm thick. The slabs used for histopathologic analysis were processed with PS, FS, or TIC as was standard at each institution and were used for patient management at each site. In addition, 3 extra PS slides were made from each tissue slab and were evaluated at a central pathology site; these slides consisted of three 4- to 6-μm thick sections collected at 3 levels, 150 μm apart.
In the validation series of 416 patients, when compared with PS, the assay detected 98% of metastases greater than 2 mm and 88% of metastases greater than 0.2 mm. Micrometastases were less frequently detected (57%), and assay-positive results in nodes found negative by histology were rare (4%). Disagreements seen between PS histology performed on adjacent node slabs and the molecular assay results were similar to the disagreements seen between histology performed on site slides versus central slides. Positive results of tests using additional molecular markers on nodes with positive BLN but overall negative histologic findings suggest that discrepancies were more likely due to sampling differences rather than to a false-positive result on BLN assay. In summary, the studies showed that BLN appeared to be a properly calibrated intraoperative molecular test that approaches the results obtained from PS histology. Compared with FS intraoperative testing, the assay showed improved sensitivity ranging from 10% to approximately 30%. In cases of invasive lobular carcinoma, FS sensitivity was 65.2% with a specificity of 97.8%, but the assay was 91.3% sensitive with a specificity of 95.7% (71 cases).
On July 17, 2007, the BLN assay received approval for clinical use from the FDA. The assay was labeled as a qualitative in vitro diagnostic test for the rapid detection of greater than 0.2 mm metastasis in nodal tissue removed from the sentinel node biopsies of breast cancer patients. Results from the assay could be used to guide intraoperative or postoperative decision making regarding removal of additional lymph nodes. The clinical use of the molecular assay began at Morton Plant Hospital on July 31, 2007. Analysis of that clinical use follows.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree