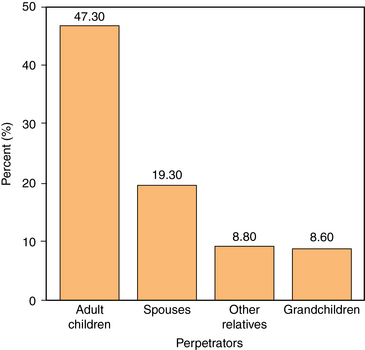
33 Upon completion of this chapter, the reader will be able to: • Know the caregiver, care recipient, and social factors associated with elder mistreatment. • Know the different types of abuse and neglect. • Recognize components of the history and physical examination that raise concern for possible abuse. • Explain and overcome barriers to the identification of abuse. Translating the definition of abuse (Box 33-1) to a diagnosis of abuse is not easy nor is it straightforward: It is often difficult to distinguish between injuries that occur through innocent mechanisms (e.g., tripping and falling) and those that occur as a result of abuse (e.g., being punched). Although some acts of commission or omission are blatantly abusive, there is no simple method to tell when some acts, such as poor care, cross the line to become abuse. However, this does not excuse the need to make a diagnosis at the earliest possible time. Primary care providers are in a unique position to prevent, recognize, and respond to mistreatment. They are often the first to identify both victim and perpetrator and, therefore, must be mindful of the possibility of abuse as well as be able to respond to its occurrence. Physicians are among the least likely to report suspicion of abuse to Adult Protective Services (APS).2 Best estimates suggest that between 1 and 2 million Americans age 65 and older have been the victim of elder mistreatment or neglect by a caregiver.1 Only 1 in 24 cases is reported to local authorities for intervention.3 Several studies have evaluated the prevalence of specific forms of elder mistreatment in community-dwelling older adults. The National Elder Mistreatment Study published in 2010 projected the prevalence of emotional mistreatment at 4.6%, physical mistreatment at 1.6%, sexual mistreatment at 0.6%, and financial abuse at 5.2% per year.4 Prevalence of verbal mistreatment has been found to be as high as 9%.5 Contrary to popularly held perceptions, family members, particularly adult children and spouses, are the most common perpetrators of abusive acts (Figure 33-1).2 Unfortunately, victims of abuse face increased mortality rates as compared to unabused patients.6 When all other risk factors are taken into account, elder abuse by itself imposes a threefold increase in the risk of death of community-dwelling older adults.7 These patients have more psychiatric and physical disorders manifested by increased numbers of hospitalizations and emergency department visits. With increased life expectancy, it is projected that the older adult population will almost double in size to 20% of the U.S. population by 2030.8 The pool of potential victims is growing at a rapid rate. Figure 33-1 Breakdown of suspected perpetrators of elder abuse. Note: Only 16% of perpetrators are nonfamily members. (Adapted from National Center on Elder Abuse. National Elder Abuse Incidence Study: Final report. Washington, DC: Department of Health and Human Services Administration for Children and Families and Administration on Aging; September 1998.) Risk factor assessment is important to identify potential elder mistreatment victims and initiate treatment. Risk factors are found in the victim, perpetrator, and sociocultural environment in which they are embedded (Box 33-2). Dementia is a known risk factor for mistreatment. In a study published in 2010, 47% of patients with dementia were found to be mistreated by their caregiver. Associated factors thought to increase the risk of abuse in people with dementia include caregiver depression, anxiety, and perceived burden of care; and care recipients with physically aggressive behaviors. This study found that when asked, caregivers of patients with dementia will acknowledge abuse.9 Alcohol and/or drug abuse among perpetrators of elder mistreatment is also common.10
Mistreatment and neglect
Incidence and impact
Risk factors and pathophysiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Oncohema Key
Fastest Oncology & Hematology Insight Engine

