Miscellaneous Chemotherapeutic Agents
M. Sitki Copur
Scott Nicholas Gettinger
Sarah B. Goldberg
Hari A. Deshpande
HOMOHARRINGTONINE AND OMACETAXINE
Homoharringtonine and its congener, harringtonine, are cephalotaxine esters isolated from the evergreen tree Cephalotaxus hainanensis, which are distributed throughout southern and northeastern China. The two differ only by a single methylene group, but both have a similar activity against murine leukemia.1 The primary action of homoharringtonine appears to be the inhibition of protein synthesis and chain elongation through binding to 80S ribosome in eukaryotic cells.2 DNA effects may also be important, involving a block in progression of cells from G1 phase into S phase and from G2 phase into M phase.3 Homoharringtonine exhibits a triphasic plasma decay with a terminal half-life of 65.3 hours and apparent volume of distribution of 2.4 L/kg.4 In early phase I studies, homoharringtonine was administered as a 10 to 360 minute infusion daily for 10 days.5 Dose-limiting cardiovascular toxicity with hypotension began 4 or more hours after drug administration, which was alleviated by interrupting the infusion or by fluid administration and prolonging the duration of administration. Initial clinical studies with homoharringtonine in China showed activity against acute myeloid leukemia (AML) and chronic phase chronic myeloid leukemia (CML).6 Variable activity was observed in the initial series of phase II trials in pediatric and adult patients with acute leukemia. In early studies of homoharringtonine, a continuous intravenous (IV) infusion at 2.5 mg/m2 per day for 10 to 14 days per month induced complete hematologic and cytogenetic responses in 72% and 31% of patients, respectively, with chronic phase CML.7
The greater availability of homoharringtonine led to its further testing and the development of a semisynthetic cephalotaxine ester, omacetaxine mepesuccinate.2 The mechanism of action of omacetaxine includes inhibition of protein synthesis and is independent of direct Bcr-Abl binding. In vitro, it reduces protein levels of the Bcr-Abl oncoprotein and Mcl-1, an antiapoptotic B-cell lymphoma 2 (Bcl-2) family member. The antileukemic effect of omacetaxine is not affected by the presence of mutations in Bcr-Abl.8 Omacetaxine is absorbed following subcutaneous administration of 1.25 mg/m2 twice daily for 11 days with a mean half-life of 6 hours, and a volume of distribution of 141 +/−93.4 L. A phase 2 trial assessed the efficacy of omacetaxine in CML patients with T315I and tyrosine-kinase inhibitor failure. Patients received subcutaneous omacetaxine 1.25 mg/m2 twice daily on days 1 through 14, every 28 days until hematologic response or a maximum of 6 cycles, and then days 1 through 7 every 28 days as maintenance. Complete hematologic response was achieved in 77%, with a median response duration of 9.1 months. Of patients, 23% achieved a major cytogenetic response, including a complete cytogenetic response in 16%. Hematologic toxicity included thrombocytopenia (76%), neutropenia (44%), and anemia (39%) and was typically manageable by dose reduction. Nonhematologic adverse events were mostly grade 1/2 and included infection, diarrhea, and nausea.9
L-ASPARAGINASE
L-Asparaginase (L-asparagine aminohydrolase, EC 3.5.1.1), which catalyzes the hydrolysis of the essential amino acid L-asparagine to L-aspartic acid and ammonia, is a naturally occurring enzyme in some microorganisms.10,11 Although cancer cells depend on an exogenous source of L-asparagine for survival, normal cells can synthesize asparagine. In addition to the depletion of L-asparagine, it may exert its antitumor activity through a glutaminase effect, depleting essential glutamine stores and leading to the inhibition of DNA biosynthesis. It comes in three preparations, two of which are native forms purified from bacterial sources, Escherichia coli and Erwinia carotovora. A third preparation, pegylated (PEG)-L-asparaginase, is a chemically modified form of the enzyme in which native E. coli L-asparaginase has been covalently conjugated to polyethylene glycol.12
After an intramuscular (IM) injection, peak plasma levels, approximately one-half of those achieved with IV administration, are reached within 14 to 24 hours. Plasma protein binding is 30%. The pharmacokinetics vary depending on the source of the enzyme.13 Pharmacokinetic studies in newly diagnosed children with acute lymphocytic leukemia (ALL) have shown peak serum concentrations in the range of 1 to 10 IU/mL in 24 to 48 hours of a single dose of 2,500 to 25,000 IU/m2 of the enzyme derived from E. coli. After a single dose of 25,000 IU/m2, peak serum levels are reached within 24 hours. PEG-L-asparaginase, when administered at a dose of 2,500 IU/m2, achieves peak drug levels at 72 to 96 hours and has a significantly longer half-life (5.7 days) than the E. coli L-asparaginase preparation.13 Clinical trials have demonstrated the efficacy, safety, and tolerability of PEG-L-asparaginase administered intramuscularly, subcutaneously, or intravenously as part of multiagent chemotherapy regimens in the management of newly diagnosed and relapsed pediatric and adult ALL. L-Asparaginase can antagonize antineoplastic effects of methotrexate if given concurrently or immediately before. These two drugs should be administered sequentially at least 24 hours apart. L-Asparaginase has also been shown to inhibit the metabolic clearance of vincristine and can result in increased neurotoxicity. Toxicity is less pronounced if L-asparaginase is administered after vincristine. Hypersensitivity reactions occur in up to 25% of patients as a skin rash and urticaria or serious anaphylactic reactions. The risk increases with repeat exposure, and as a single-agent use without steroids. PEG-L-asparaginase is less immunogenic than the native nonpegylated forms of the enzyme. A number of other side effects are observed that are secondary to the inhibitory effects of L-asparaginase on cellular protein synthesis. Decreased serum levels of insulin, key lipoproteins, and albumin have been reported. L-Asparaginase can cause alterations in thyroid function tests as early as 2 days after an administered dose, possibly secondary to a reduction in the serum levels of thyroxine-binding globulin. Alterations in coagulation parameters with prolonged thrombin time, prothrombin time, and partial thromboplastin time have been observed. Patients treated with L-asparaginase are at an increased risk for bleeding or thromboembolic
events.14 L-Asparaginase is contraindicated in patients with a prior history of pancreatitis, because there is a 10% incidence of acute pancreatitis. Neurologic toxicity includes lethargy, confusion, agitation, hallucinations, and/or coma. In contrast to the other anticancer agents used to treat ALL, myelosuppression is rare.
events.14 L-Asparaginase is contraindicated in patients with a prior history of pancreatitis, because there is a 10% incidence of acute pancreatitis. Neurologic toxicity includes lethargy, confusion, agitation, hallucinations, and/or coma. In contrast to the other anticancer agents used to treat ALL, myelosuppression is rare.
BLEOMYCIN
Bleomycin is a glycopeptide antibiotic produced by the bacterium Streptomyces verticillus. The most active chemotherapeutical forms are bleomycin A2 and B2.15 The effect of bleomycin is cell cycle specific, because its main effects are mediated in the G2 and M phases of the cell cycle.16 The exact mechanism for DNA strand scission has been suggested to be due to bleomycin’s chelating of metal ions (primarily iron) and producing a pseudoenzyme that reacts with oxygen to produce superoxide- and hydroxide-free radicals, thus cleaving DNA. Alternatively, bleomycin may bind at specific sites in the DNA strand and induce scission by abstracting the hydrogen atom from the base, resulting in strand cleavage as the base undergoes a Criegee-type rearrangement, or bleomycin may form an alkali-labile lesion.17 Bleomycin is used in the treatment of Hodgkin lymphoma (as a component of the ABVD and BEACOPP regimen), squamous cell carcinomas, and testicular cancer; in the treatment of plantar warts,18 as a means of effecting pleurodesis,19 as well as an intralesional agent with electrochemotherapy in the management of cutaneous malignancies.20
The oral bioavailability is poor. It must be administered via IV or IM routes. The initial distribution half-life is 10 to 20 minutes with a terminal half-life of 3 hours. Bleomycin can be administered via the intracavitary route to control malignant pleural effusions or ascites, or both. Approximately 45% to 55% of an administered intracavitary dose of bleomycin is absorbed into the systemic circulation. Elimination is primarily via the kidneys, and approximately 60% to 70% of an administered dose is excreted unchanged in the urine. Dose reductions are required if creatinine clearance is less than 25 mL per minute.
Bleomycin-induced pneumonitis, the dose-limiting toxicity of the drug, occurs in 10% of patients, and is dependent on the cumulative dose.21 The risk increases in patients older than 70 years and in those who receive a total cumulative dose greater than 400 U. In addition, patients with an underlying lung disease, prior irradiation to the chest or mediastinum, and exposure to high concentrations of inspired oxygen are at increased risk. Increased use of granulocyte colony-stimulating factor (G-CSF) has been paralleled by an increased incidence of bleomycin-induced pulmonary toxicity. The exacerbating effects of G-CSFs seem to be associated with a marked infiltration of activated neutrophils along with the lung injury caused by the direct effects of bleomycin.22,23 In a retrospective review, 18% of a total of 141 patients with Hodgkin lymphoma treated with a bleomycin-containing regimen developed pulmonary toxicity. G-CSF use was one of the key factors associated with the development of this complication, and omission of bleomycin had no impact on clinical outcomes.24 Similarly the combination of brentuximab vedotin and ABVD was associated with excessive pulmonary toxicity, indicating that brentuximab vedotin and bleomycin should not be used together.25
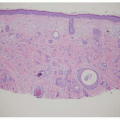
Patients with bleomycin-induced pulmonary toxicity may present with cough, dyspnea, dry inspiratory crackles, and infiltrates on chest radiograph. Pulmonary function testing is the most sensitive approach to monitor patients, and pulmonary function tests should be obtained at baseline and before each cycle of therapy, with a specific focus on the carbon monoxide diffusion capacity and vital capacity. A decrease greater than 15% in either diffusion capacity of carbon monoxide or vital capacity should mandate immediate discontinuation of bleomycin. Early clinical trials and isolated case reports suggest that bleomycin-induced acute hypersensitivity reactions occur in 1% of patients with lymphoma and less than 0.5% of those with solid tumors. The reactions are mainly characterized by high-grade fever, chills, hypotension, and, in a few cases, cardiovascular collapse, which can lead to death. The exact mechanism of these reactions is unclear, but is thought to be related to the release of endogenous pyrogens from the host cells. Supportive care, including hydration, steroids, antipyretics, and antihistamines, may resolve the symptoms.
Clinicians should monitor their patients for any signs and symptoms of acute hyperpyrexic reactions during bleomycin administration. Because the onset of the reactions can occur with any dose of bleomycin and at any time, routine test dosing does not seem to predict when drug reactions may occur.26 Mucocutaneous toxicity presents as mucositis, erythema, hyperpigmentation, induration, hyperkeratosis, and skin peeling, which may progress to ulceration, and usually develops in the 2nd and 3rd week of treatment and after a cumulative dose of 150 to 200 U of the drug. Levels of bleomycin hydrolase are relatively low in lung and skin tissue, perhaps offering an explanation as to why these normal tissues are more adversely affected by bleomycin. Myelosuppression and immunosuppression are relatively mild. In rare cases, vascular events, including myocardial infarction, stroke, and Raynaud phenomenon, have been reported.
PROCARBAZINE
Originally prepared as a monoamine oxidase inhibitor, procarbazine is a prodrug, which after oxidation of the hydrazine in the liver, undergoes a complex enzymatic and chemical breakdown to its alkylating and methylating species.27,28 The precise mechanism of action is uncertain, but may involve damaging the DNA, RNA or transfer RNA, and the inhibition of protein synthesis. Procarbazine is a cell-cycle phase-nonspecific antineoplastic agent. This agent was initially approved by the U.S. Food and Drug Administration (FDA) in 1969 as part of the MOPP (mechlorethamine, vincristine, procarbazine, and prednisone) regimen for the treatment of Hodgkin lymphoma. Since then, it has also demonstrated clinical activity in non-Hodgkin lymphoma, cutaneous T-cell lymphoma, and brain tumors.
Procarbazine is rapidly and completely absorbed from the gastrointestinal tract. Following oral administration, peak drug levels are reached within 10 to 15 minutes. Procarbazine crosses the blood-brain barrier and rapidly equilibrates between plasma and cerebrospinal fluid after oral administration. Peak cerebrospinal fluid drug concentrations are reached within 30 to 90 minutes after drug administration. The biologic half-life of procarbazine hydrochloride in both plasma and cerebrospinal fluid is approximately 1 hour. Procarbazine is metabolized to active and inactive metabolites by chemical breakdown in an aqueous solution and the liver microsomal P-450 system. Approximately 70% of procarbazine is excreted in urine within 24 hours, and less than 5% to 10% of the drug is eliminated in an unchanged form.29,30
A careful food and drug history is required before starting a patient on procarbazine therapy, because there are several potential drug-drug and drug-food interactions. Patients should avoid tyramine-containing foods, such as dark beer, wine, cheese, yogurt, bananas, and smoked foods. Procarbazine produces a disulfiramlike reaction with concurrent use of alcohol. Acute hypertensive reactions may occur with coadministration of tricyclic antidepressants and sympathomimetic drugs. Concurrent use of procarbazine with antihistamines and other central nervous system (CNS) depressants can result in CNS and/or respiratory depression.
Dose-limiting toxicity is myelosuppression, more commonly thrombocytopenia, and the nadir in platelet count is generally observed at 4 weeks. Patients with glucose-6-phosphate dehydrogenase deficiency can develop hemolytic anemia while receiving procarbazine therapy. Stepwise dose increments over the first few days of drug administration may minimize gastrointestinal intolerance. On rare occasions, procarbazine may induce interstitial pneumonitis, which mandates the discontinuation of therapy. Azoospermia and infertility after treatment with MOPP can be attributed, in part, to procarbazine. Procarbazine is associated with an increased risk of secondary malignancies, especially acute leukemia.
VISMODEGIB
Vismodegib (Erivedge, GDC-0449, Genentech) is a first-in-class, small-molecule inhibitor of the Hedgehog pathway. It binds to and inhibits smoothened, a transmembrane protein that is involved in Hedgehog signaling.31 Pharmacodynamic downmodulation in the Hedgehog pathway was shown by a 90% decrease in transcription factor Gli1 mRNA in basal-cell carcinoma biopsy specimens of patients treated for a month. One-month vismodegib treatment also significantly reduced tumor proliferation, as assessed by Ki-67 expression, but did not change apoptosis, as assessed by cleaved caspase 3. The extent of Gli1 downmodulation does not seem to correlate with pharmacokinetic levels of vismodegib in individual patients. Vismodegib is absorbed from the gastrointestinal tract, with an oral bioavailability of 32%. Food does not affect drug exposure. Elimination is mainly hepatic, with excretion in feces. The median steady-state concentration is not changed by increasing the dose from 150 mg to 270 mg, and the median time to steady state is 14 days. The half-life is estimated at 8 days after a single dose. Intermittent doses (e.g., three times per week or once per week) were associated with a decrease of 50% and 80% in effective plasma levels of unbound drug, respectively, thus reinforcing the recommended dose and schedule of 150 mg orally daily.32 Vismodegib is approved for the treatment of adults with metastatic basal-cell carcinoma that has recurred following surgery or in those who are not candidates for surgery and who are not candidates for radiation.33
No dose-limiting toxic effects or grade 5 events have been observed. However, 54% of patients receiving vismodegib discontinued the medication owing to side effects, and only one out of give eligible patients was able to continue vismodegib for 18 months. Abdominal pain, fatigue, weight loss, dysgeusia, and anorexia were reasons for discontinuation of the drug. When vismodegib was withdrawn, dysgeusia and muscle cramps ceased within 1 month, and scalp and body hair started to regrow within 3 months. Other side effects reported include hyponatremia, dyspnea, muscle spasm, atrial fibrillation, aspiration, back pain, corneal abrasion, dehydration, keratitis, lymphopenia, pneumonia, urinary tract infection, and a prolonged QT interval.34
ADO-TRASTUZUMAB EMTANSINE
Ado-trastuzumab emtansine (T-DM1), is a HER2-targeted anti-body-drug conjugate (ADC). It is a novel compound composed of trastuzumab, a stable thioether linker, and DM1. DM1, a derivative of maytansine, is a microtubule polymerization inhibitor with activity similar to that of vinca alkaloids. T-DM1 is taken up into cells after binding to HER2, allowing for cytotoxic drug delivery specifically to cells overexpressing HER2. It has a drug-to-antibody ratio of approximately 3.5:1. T-DM1 is administered intravenously every 3 weeks and has been tested in a phase I trial at doses ranging from 0.3 to 4.8 mg/kg. The maximally tolerated dose is 3.6 mg/kg, which was the dose used in further phase II-III trials. T-DM1 is metabolized by the liver, via CYP3A4/5, and has a half-life of 3.5 days.35
T-DM1 is approved for use in patients with metastatic HER2-positive breast cancer who have received prior trastuzumab and a taxane. This approval was based on the results of the EMILIA trial, which randomized 991 patients with HER2-positive unresectable, locally advanced or metastatic breast cancer to T-DM1 3.6 mg/kg IV every 21 days or lapatinib 1,250 mg daily plus capecitabine 1,000 mg/m2 on days 1 through 14 every 21 days. All patients were previously treated with trastuzumab and a taxane. T-DM1 resulted in a progression-free survival of 9.6 months compared to 6.4 months for lapatinib plus capecitabine (hazard ratio [HR] 0.65; 95% confidence interval [CI] 0.55 to 0.77; p <0.001). The response rate and overall survival was also higher with T-DM1 compared to lapatinib plus capecitabine.36
Although maytansine itself is associated with significant toxicity, T-DM1 is very well tolerated overall, which is likely due to the targeted nature of the compound. Side effects from T-DM1 include thrombocytopenia, hepatotoxicity, hypersensitivity/infusion reactions, and cardiotoxicity. Nausea, fatigue, headaches, and anemia are also common. The left ventricular ejection fraction should be monitored prior to and at least every 3 months during therapy because of the potential for cardiac dysfunction.
SIROLIMUS AND TEMSIROLIMUS
Sirolimus (rapamycin) was isolated from the soil bacteria Streptomyces hygroscopicus, in the mid 1970s.37 This bacterial macrolide later became the preferred immunosuppressant for kidney transplantation, because it was mildly immunosuppressive; however, in contrast to cyclosporine A, it did not enhance tumor incidence.38 Sirolimus is the prototypic inhibitor of the mammalian target of rapamycin (mTOR), a serine/threonine protein kinase that is a highly conserved regulatory protein involved in cell-cycle progression, proliferation, and angiogenesis.39 Signaling pathways both upstream and downstream of mTOR have been shown to be commonly dysregulated in cancer. mTOR functions through two main mechanisms, depending on the presence and activity of the mTOR-associated protein complexes, mTORC1 and mTORC2. Sirolimus and its analog compounds, temsirolimus and everolimus, form a complex with the FK-binding protein (FKBP) and inhibit activation of a subset of mTOR proteins residing within mTORC1. In contrast, mTORC2 holds mTOR in a form that is not as readily inhibited by these rapamycin analogs, and upregulation of mTORC2 may represent a mechanism by which resistance can develop to this class of compounds.
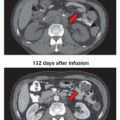
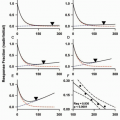
Temsirolimus (CCI-779), a novel functional ester of sirolimus, is a water-soluble dihydroxymethyl propionic acid compound that rapidly undergoes hydrolysis to sirolimus after IV administration, reaching peak concentrations within 0.5 to 2.0 hours.40 This drug is widely distributed in tissues, and steady-state drug levels are reached in 7 to 8 days. Temsirolimus is metabolized primarily in the liver by CYP3A4 microsomal enzymes to yield sirolimus as the main metabolite. The terminal half-life of temsirolimus is 17 hours, whereas that of sirolimus is approximately 55 hours. When bound to temsirolimus, mTOR is unable to phosphorylate the key protein translation factors, such as 4E-BP1 and S6K1, leading to translational inhibition of several critical regulatory proteins involved in cell-cycle control. Several other cellular proteins involved in the regulation of angiogenesis, such as hypoxia-inducible factor-1α (HIF-1α) and vascular endothelial growth factor (VEGF), are suppressed through mTOR inhibition by temsirolimus.
Phase I studies of temsirolimus have investigated various schedules and doses, ranging from 7.5 mg to 220 mg given as weekly 30-minute infusions.40 A phase II study in patients with cytokinerefractory renal cell cancer (RCC) investigated the efficacy and safety of three different dose levels (25 mg, 75 mg, and 250 mg, respectively) administered on a weekly schedule. This study showed promising antitumor activity for all three dose levels with no significant difference in efficacy or toxicity.41 As a result, the 25-mg dose was eventually selected as the monotherapy dose for further study. A phase III randomized trial compared interferon, temsirolimus, and the combination of the two agents in previously untreated patients with advanced RCC who had at least three of six poor prognostic features.42 Once-weekly IV temsirolimus, 25 mg, prolonged the median overall survival of patients with poor prognostic features by 49% from 7.3 months (95% CI, 6.1 to 8.8 months) in the interferon arm to 10.9 months (95% CI, 8.6 to 12.7 months) in the temsirolimus arm (P = .008). The temsirolimus arm also had a prolonged median progression-free survival of 5.5 months compared to 3.1 months in the interferon arm (P <.001). Moreover, temsirolimus was effective for both clear cell and non-clear cell histologies.43,44
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree