Fig. 13.1
MIVAP: Left inferior laryngeal nerve and left superior parathyroid adenoma
Thanks to the central access, MIVAP allows contralateral parathyroid glands exploration through the same skin incision when necessary (suspicious of multiglandular disease because of inadequate IO-PTH decrease, two enlarged glands found at unilateral exploration, inadequate preoperative localization studies, etc.). Once identified, the parathyroid adenoma is bluntly dissected under endoscopic view using spatulas and a spatula shaped aspirator (Karl STORZ, Tuttlingen, Germany). The pedicle of the adenoma is usually clipped with titanium clips or tied with conventional ligature. After cutting the pedicle, the adenoma is extracted through the skin incision (Fig. 13.2). IO-PTH assay is used to confirm the removal of all pathologic parathyroid tissue. After checking for hemostasis the strap muscles and the platysma are closed. The skin is closed by a nonresorbable subcuticular running suture or by skin sealant. No drain is used.
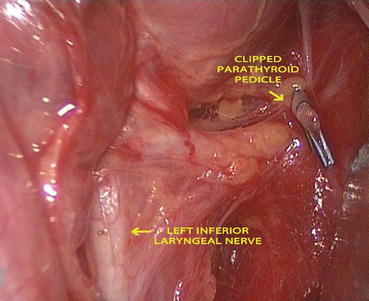
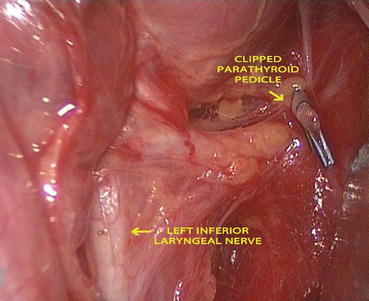
Fig. 13.2
Operative field after left superior video-assisted parathyroidectomy
13.3 Indications
Patients with sporadic pHPT in whom a single adenoma is suspected based on preoperative imaging studies (MIBI-scan and ultrasonography) are ideal candidates for MIVAP. Parathyroid adenoma larger than 3 cm is usually excluded because of the theoretical risk of capsular rupture and consequent parathyromatosis due to difficult dissection and extraction [26, 27].
At the beginning of the experience exclusion criteria included previous neck surgery, persistent or recurrent hyperparathyroidism, mediastinal adenomas, and concomitant large goiter. With the increasing experience, selection criteria for MIVAP have been widened. Patients with concomitant nodular goiter can undergo MIVAP if the usual inclusion criteria for the video-assisted thyroidectomy are met [28]. Moreover, in selected cases, patients with previous neck surgery or intrathymic/retrosternal adenomas can be selected for MIVAP. Because bilateral neck exploration is possible through the same access, MIVAP can be performed both in patients with suspected multiglandular disease and in patients with uncertain preoperative localization [27].
The rate of patients with sporadic pHPT who are candidates for MIVAP varies (37–71 %) [15, 26] due to different incidence of coexisting thyroid diseases that may require a conventional approach [15].
13.4 Experience and Complications
Conversion rate is highly variable ranging from 0.9 % [15] to 25 % [31]. The more frequent indications to conversion are bleeding, inadequate IO-PTH decrease, false preoperative localization, difficult to localize/dissect the parathyroid adenoma(s), suspicious of malignancy, and ectopic localization of the pathologic gland. Proper patient selection and surgical team experience are able to lower the conversion rate even in regions with reported endemic goiters [15, 28].
Also the operative time strongly depend on surgical team skill and experience. Indeed, it has been demonstrated that the operative time decreases significantly with increasing experience and it is comparable or even shorter than that of conventional operation [15, 26, 32].
Several large retrospective series have reported on the short- and medium-term outcome of MIVAP. In 350 cases of MIVAP in 6 years, Miccoli et al. [26] reported a cure rate of 98.3 %. At a medium follow-up of 35.1 months, 4 patients had persistent disease due to false-positive IO-PTH. Complications occurred in 14 patients: 2.7 % transient hypocalcemia, 0.8 % permanent nerve palsy, and 0.3 % postoperative bleeding [26]. Others have reported similar results in smaller series [21, 23]. In our previous published series of 107 cases of MIVAP we reported a success rate of 98.1 % with persistent disease in 2 patients (1.9 %) [15]. We reported a 11.1 % rate of temporary hypocalcemia with no permanent hypoparathyroidism, and no other complications [15].
13.5 Advantages and Disadvantages
MIVAP presents some technical advantages compared with other endoscopic or video-assisted techniques [27]. First of all, this technique combines the advantages related to the endoscopic magnification with those due to its similarity with the conventional surgery. Indeed, the operative procedure reproduces all the steps of the open procedure. The excellent visualization of the neck structures due to the 2–3 fold endoscopic magnification permits easy identification of the laryngeal nerve and parathyroid glands. In a recently published prospective randomized trial, the mean time for adenoma localization was significant shorter for the group of patients who underwent MIVAP compared with patients operated on with an open minimally invasive technique [7].
Another merit of the technique is the possibility to perform a bilateral neck exploration when necessary through the same central access. This characteristic in part explains the very low conversion rate reported in different series [15, 26]. The possibility to perform a bilateral neck exploration produces two main effects on the restrictive inclusion criteria. Indeed, MIVAP can also be performed in case of unavailability of intra-operative PTH monitoring or in case of inadequate preoperative localization studies, because of the possibility to explore all the parathyroid sites [15, 33]. Another advantage of the central access is the possibility of associate thyroid resection, even bilateral, when necessary. Because of the high prevalence of multinodular goiter in some countries, this technical characteristic allowed experienced surgeons to increase the rate of patients eligible for a video-assisted procedure in selected patients. In our experience, with the high prevalence of goiter in Italian population, this allowed us to treat both thyroid and parathyroid diseases simultaneously in more than 30 % of the patients [28].
Moreover, the video-assisted access could imply a better cosmetic result and a less postoperative pain. Indeed, several comparative studies have demonstrated the advantages of MIVAP to reduce the postoperative pain, improve the cosmetic result and the patient satisfaction over both conventional and open non-endoscopic minimally invasive parathyroidectomy [7, 8].
Some criticisms about technical aspects for MIVAP still exist and are mainly related to the operative time. However, it has been demonstrated in large retrospective series [15, 26] and also in small comparative, randomized trials [7] that the operative time does not represent a limit.
Another technical problem is the number of members of the surgical team. The fact that two assistants are necessary to accomplish the MIVAP can represent an important concern for the application and diffusion of the procedure, at least in some surgical setting.
On the other hand, the main technical limitation of MIVAP is still represented by the volume of parathyroid adenoma and of the eventually associated goiter. Dissection and extraction of large adenomas through a small incision can result in capsule rupture with the theoretical risk of parathyromatosis [15]. In contrast, previous neck surgery and the absence of a clear preoperative localization are not contraindications for MIVAP.
13.6 Avoiding Complications
In spite several reports have demonstrated that thyroid and parathyroid procedure are safely performed by residents operating under supervision and newly established surgical consultant, there is a significant inverse relationship between the number of procedures performed and the complication rate [34]. In other words patient volumes and surgical skill play an important role in reducing complications rate, as in other fields of surgery.
Obviously, lower complications rate are obtained in third care referral centers, where dedicated surgical teams and well-trained endocrine surgeons are provided and hospital facilities allow adopting all the measures and tools known by the medical community as the gold standard for patients treatment.
When the procedure is performed under optimal conditions combined with meticulous operative skill by surgeons who have been adequately trained, the incidence of complication should be at a minimum [34]. Nonetheless, complication may occur, not only because of surgical errors, but also for factor related to the patients or the disease itself.
13.6.1 Postoperative Hematoma
Data from the literature concur to demonstrate that the rate of postoperative major bleeding requiring surgical revision after video-assisted parathyroidectomy approaches the 0 % and only a few cases have been reported [15, 26, 34]. Even in absence of any significant difference in terms of postoperative complications in the published comparative studies [27], it could be inferred that the limited dissection, which characterizes these techniques, has the potential benefit to reduce the risk of this complication. These results could be biased by strict selection criteria for these procedures and the possible reduction of the postoperative bleeding could be related to the absence of other possible risk factors. Postoperative bleeding could be prevented by eliminating the cause in the majority of the patients. A meticulous surgical technique and hemostasis are mandatory to avoid or reduce the risk of this complication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree