Fig. 15.1
The camera is handled by an assistant who can rotate it in order to better expose the site of dissection
Harmonic scalpel is particularly useful when a VA-CCD is carried out because it can easily coagulate and cut all the lymphatic vessels, reducing the operating time and the risk of lymphatic leaks.
For what concerns the patient position and the composition of the surgical staff we refer to the chapter describing MIVAT.
For VA-CCD general anaesthesia with orotracheal intubation is required.
VA-CCD is accomplished, during MIVAT, through the same skin access, a small (1.5–2 cm) skin incision performed in the midline, usually just below (1 cm) the cricoid cartilage. Such a cranial position of the skin incision, that is of utmost importance to perform MIVAT because it permits a good exposure and a safe control of the superior vessels peduncle, does not represent an obstacle to approach the lymph nodes located in the upper mediastinum. In fact an optimal preparation of the upper and lower subcutaneous flaps, consents to open the cervical linea alba as far as possible and permits the small skin access to move on the deepest planes, under the skilled use of the retractors, letting the endoscopic instruments and the camera easily reach both the upper six level lymph nodes and the lower ones. In such a way it is possible to perform a complete VI level neck dissection removing all the lymph nodes and the fatty tissue from the bone hyoid superiorly, the innominate artery inferiorly, the pre-vertebral fascia dorsally, and between carotid arteries laterally [25].
The dissection is carried out by a blunt technique using the same two dedicated instruments called spatulas, previously mentioned for MIVAT. VA-CCD is carried out under endoscopic vision, selectively clipping and cutting, or directly cutting with an ultrasound knife system (Ultracision®), the lymphatic vessels. It is very important to accurately control the tip of the instrument to avoid any injury of the recurrent nerves and trachea. The magnification (two- to threefold) of the endoscope permits a quite easy identification of the nerves and parathyroid glands (Fig. 15.2).
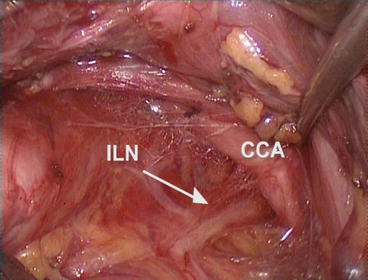
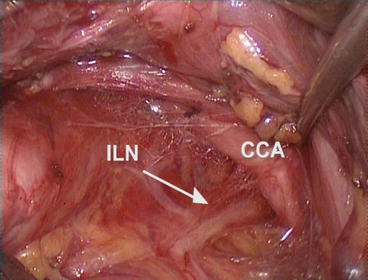
Fig. 15.2
The magnification (two- to threefold) of the endoscope permits a quite easy identification of the nerves and parathyroid glands. ILN inferior laryngeal nerve; CCA common carotid artery
Nonetheless, as highlighted above in our introduction, the endoscope enables the identification of enlarged lymph nodes and consequently not only influences the surgeon’s decision making but, during the procedure, allows a more accurate dissection (Fig. 15.3).
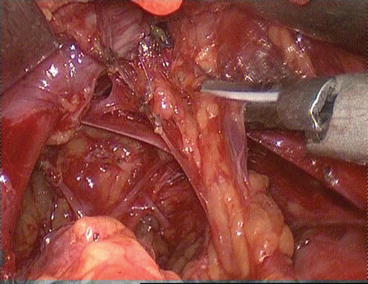
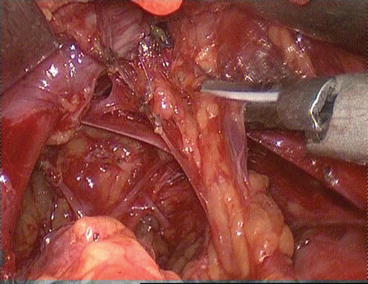
Fig. 15.3
The endoscope enables the identification of enlarged lymph nodes allowing a more accurate dissection
After checking the haemostasis the strap muscles are sutured along the midline as well as the platysma. The skin is closed by means of a not re-absorbable subcuticular running suture or by a skin sealant. Usually no drainage is left inside.
15.4 Personal Experience and Complications
A total of 161 VA-CCD were attempted between January 2000 and June 2014. No conversion to the conventional procedure was necessary.
Pathological studies showed DTC pT1 in 101 cases, pT2 in 6 cases and pT3 in 54 cases. Lymph node metastases were found in 79 patients (41 pT1, 2 pT2, 36 pT3).
Postoperative complications included 2 cases of transient (1.2 %) recurrent laryngeal nerve palsy, 63 cases of transient hypocalcemia (39.1 %) and 3 cases of definitive hypoparathyroidism (1.8 %). No definitive recurrent laryngeal nerve palsy, no postoperative hematoma and no wound infection occurred.
References
1.
2.
3.
Mourad M, Saab N, Malaise J et al (2001) Minimally invasive video-assisted approach for partial and total thyroidectomy: initial experience. Surg Endosc 15:1108–1111PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree