Surgical resection remains the treatment of choice for primary pancreatic neuroendocrine tumors (PNETs), because it is associated with increased survival. Minimally invasive procedures are a safe modality for the surgical treatment of PNETs. In malignant PNETs, laparoscopy is not associated with a compromise in terms of oncologic resection, and provides the benefits of decreased postoperative pain, better cosmetic results, shorter hospital stay, and a shorter postoperative recovery period. Further prospective, multicenter, randomized trials are required for the analysis of these minimally invasive surgical techniques for the treatment of PNETs and their comparison with traditional open pancreatic surgery.
Key points
- •
Surgical resection is the only curative treatment of pancreatic neuroendocrine tumors (PNETs).
- •
Minimally invasive procedures are a safe modality for the surgical treatment of PNETs.
- •
Laparoscopy does not compromise oncologic resection, and is associated with decreased postoperative pain, better cosmetic results, a shorter hospital stay, and a shorter postoperative recovery period.
- •
The overall 5-year and 10-year survival rates for all PNETs are approximately 65% and 45%, respectively.
Introduction
Pancreatic neuroendocrine tumors (PNETs) are a heterogeneous group of neoplasms that have an incidence of 1 per 100,000 individuals per year, and account for 1% to 2% of all pancreatic neoplasms. PNETs can develop at any age, but they are more frequently seen in patients between the fourth and sixth decades of life. Although most tumors are considered sporadic, about 10% to 30% of cases present in patients with familial syndromes such as multiple endocrine neoplasia type 1 (MEN1),von Hippel-Lindau, neurofibromatosis type 1, and tuberous sclerosis, among other more rare syndromes. PNETs can be classified into functional and nonfunctional tumors. Functional tumors are usually detected early because of the symptoms caused by hormonal production. Nonfunctional tumors are more common, but given the absence of hormonal symptoms these tumors are found incidentally or in more advanced stages of the disease, with larger tumors causing mass effect, invading surrounding tissues or presenting with metastatic disease.
Surgical resection of the primary tumor remains the treatment of choice for PNETs, because it is associated with increased survival. With the advancement of minimally invasive techniques, an increasing number of laparoscopic surgical resections for pancreatic neuroendocrine tumors are currently performed. Low-risk PNETs in the body and the tail of the pancreas are suitable for minimally invasive surgery, with enough evidence in the literature supporting better outcomes of the laparoscopic approach compared with open surgery. However, minimally invasive pancreatic surgery has not yet been widely accepted as the gold standard for all pancreatic resections. Most recently, robotic surgical techniques across different specialties have slowly gained popularity, although the existing experience is only based on reports of small series. This article provides an insight into well-established minimally invasive procedures and also those that slowly have gained popularity over the last few years. It also reviews and discusses the different minimally invasive surgical techniques with their benefits and limitations.
Introduction
Pancreatic neuroendocrine tumors (PNETs) are a heterogeneous group of neoplasms that have an incidence of 1 per 100,000 individuals per year, and account for 1% to 2% of all pancreatic neoplasms. PNETs can develop at any age, but they are more frequently seen in patients between the fourth and sixth decades of life. Although most tumors are considered sporadic, about 10% to 30% of cases present in patients with familial syndromes such as multiple endocrine neoplasia type 1 (MEN1),von Hippel-Lindau, neurofibromatosis type 1, and tuberous sclerosis, among other more rare syndromes. PNETs can be classified into functional and nonfunctional tumors. Functional tumors are usually detected early because of the symptoms caused by hormonal production. Nonfunctional tumors are more common, but given the absence of hormonal symptoms these tumors are found incidentally or in more advanced stages of the disease, with larger tumors causing mass effect, invading surrounding tissues or presenting with metastatic disease.
Surgical resection of the primary tumor remains the treatment of choice for PNETs, because it is associated with increased survival. With the advancement of minimally invasive techniques, an increasing number of laparoscopic surgical resections for pancreatic neuroendocrine tumors are currently performed. Low-risk PNETs in the body and the tail of the pancreas are suitable for minimally invasive surgery, with enough evidence in the literature supporting better outcomes of the laparoscopic approach compared with open surgery. However, minimally invasive pancreatic surgery has not yet been widely accepted as the gold standard for all pancreatic resections. Most recently, robotic surgical techniques across different specialties have slowly gained popularity, although the existing experience is only based on reports of small series. This article provides an insight into well-established minimally invasive procedures and also those that slowly have gained popularity over the last few years. It also reviews and discusses the different minimally invasive surgical techniques with their benefits and limitations.
Diagnosis
Insulinoma
Insulinomas are the most common functional neuroendocrine tumors of the pancreas as well as the most common cause of hypoglycemia related to endogenous hyperinsulinemia. Most insulinomas are benign, small (<2 cm) tumors with only 10% of cases usually presenting as malignant lesions. They are typically solitary lesions distributed evenly throughout pancreas, except in association with MEN1 syndrome, when they tend to be multifocal. The clinical signs and symptoms of insulinomas are divided into 2 categories. Neuroglycopenic symptoms, which are a direct result of hypoglycemia, may include weakness, confusion, visual disturbances, and in extreme cases seizures and comas. Autonomic symptoms, which are a consequence of catecholamine release from hypoglycemia, include diaphoresis, palpitations, anxiety, and tremor.
Establishing a diagnosis of insulinoma has classically relied on satisfying the criteria of the Whipple triad: (1) hypoglycemia (plasma glucose level <50 mg/dL), (2) neuroglycopenic symptoms, and (3) prompt resolution of symptoms following administration of glucose. At present, biochemical measurement of plasma glucose, insulin, C peptide, and proinsulin levels during a 72-hour fast can detect up to 99% of insulinomas and has become the gold standard of diagnosis. However, in more than 97% of cases, biochemical testing in conjunction with a supervised 48-hour fast is sufficient to diagnose an insulinoma. Other conditions, such as the factitious use of insulin or oral hypoglycemic agents, can be ruled out through the measurements of plasma proinsulin, C peptide, and sulfonylurea.
Gastrinoma
Gastrinomas, along with insulinomas, account for most functional PNETs. Most of these tumors are found sporadically, although 20% to 30% are found in conjunction with MEN1. They are the most common pancreatic tumor found in patients with MEN1. Gastrinoma syndrome, also known as Zollinger-Ellison syndrome, has a slight male preponderance and is most commonly diagnosed in the fifth decade of life. Patients most often present with peptic ulcer disease, particularly multiple ulcers and ulcers that are resistant to medical treatment. Up to 75% of patients present with diarrhea, and occasionally this is the chief complaint. Most (up to 60%–90%) of these lesions are malignant, with up to 20% to 30% presenting with liver metastasis at the time of diagnosis. Ninety percent of gastrinomas are found within the gastrinoma triangle, which is formed by the borders of the second and third portions of the duodenum inferiorly, the junction of the cystic and common bile duct superiorly, and the junction between the neck and body of the pancreas medially.
The biochemical diagnosis of gastrinomas can be difficult because many conditions can cause hypersecretion of gastrin, such as the use of proton pump inhibitors, renal failure, and gastric outlet obstruction. Nonetheless, initial testing should be targeted at measuring serum gastrin levels. Increased fasting serum gastrin levels (>500 pg/mL) should prompt further testing, whereas levels greater than 1000 pg/mL are highly suspicious for gastrinoma. A finding of normal gastrin levels is often sufficient to rule out the syndrome. A high fasting serum gastrin level should prompt provocative testing to confirm the diagnosis, most commonly using secretin or calcium gluconate infusion. Secretin does not stimulate the secretion of gastrin from G cells of the stomach; however, it does lead to hypersecretion of gastrin from gastrinomas. An increase in fasting serum gastrin levels to more than 200 pg/mL is assumed to be diagnostic.
Glucagonoma
Glucagonomas, the alpha-cell counterparts of insulinomas, are rare tumors of the pancreas. Unlike insulinomas, these tumors are typically bulky, large malignant lesions, often localized to the body and tail of the pancreas. The most common presenting symptoms include mild glucose intolerance manifesting as diabetes mellitus, weight loss, normocytic anemia, and a distinct skin rash, referred to as necrolytic migratory erythema. Biochemical diagnosis is established through the serum measurement of glucagon, with levels greater than 500 pg/mL characteristic of glucagonomas.
Vasoactive Intestinal Peptideoma
Vasoactive intestinal peptideomas (VIPomas) are exceedingly rare tumors, with an estimated incidence of only 1 in 10 million per year. Approximately 70% of patients present with malignant tumors, as shown by hepatic, distant, or lymph node metastasis. Most tumors are at least 3 cm, with a mean of about 5 cm at initial presentation. Most tumors are found primarily in the body and tail of the pancreas; however, tumors can be identified in the head as well as outside the pancreas. Nearly all patients present with watery diarrhea, with most patients also presenting with hypokalemia and achlorhydria, hence the designation of WDHA syndrome. The diagnosis is established through the measurement of increased fasting serum vasoactive intestinal peptide levels (75–150 pg/mL) in the setting of secretory diarrhea.
Somatostatinoma
Neuroendocrine tumors of the pancreas secreting somatostatin are the rarest of the PNETs, with an incidence of only 1 in 40 million people per year. Most tumors are located in the head of the pancreas; however, it is common to find a lesion within the tail or outside the pancreas. At initial presentation, tumors are large (>5 cm) and nearly half are malignant. Somatostatinomas may lead to diarrhea and/or steatorrhea, cholelithiasis, and diabetes mellitus. However, most commonly patients typically present with signs or symptoms directly related to the tumor, such as abdominal pain, weight loss, or intestinal obstruction. The diagnosis is established through measurement of fasting plasma somatostatin levels, with a level greater than 160 pg/mL strongly suggestive of a somatostatinoma, particularly in the presence of a mass seen on imaging.
Preoperative evaluation
Localization
Management of PNETs depends heavily on a thorough preoperative evaluation. Various imaging studies, including MRI, computed tomography (CT), PET, endoscopic ultrasonography (EUS), and octreotide scans play an important role in localizing the primary tumor and identifying potential sites of metastases. Imaging is also important to assess response to treatment and as a screening tool for recurrence. The utility of each imaging modality differs based on the tumor type.
CT scanning is the most widely accepted and used imaging modality for localizing and staging PNETs. Compared with nonfunctional PNETs, functional PNETs are typically small at the time of diagnosis, creating more of a challenge for proper identification. These smaller tumors seldom alter the contour of the pancreas; therefore obtaining thinly sliced images enhances the ability to detect smaller tumors and should be used routinely. Fidler and colleagues showed that multiphasic imaging with early and late arterial phases as well as portal venous–phase CT had a higher sensitivity for detecting islet cell tumors. The classic CT findings of islet cell tumors are an isodense lesion during the precontrast phase and a hyperattenuating mass in both the arterial and portal venous phases ( Fig. 1 ). Depending on the biology and characteristics of the tumor, they may be more apparent during either phase.
Insulinomas are typically small on presentation and particularly difficult to diagnose. Up to 10% to 20% of these lesions are not identifiable during surgical exploration, which emphasizes the importance of preoperative localization of these tumors. With the use of more advanced helical, thinly sliced, multidimensional CT scanning, insulinomas are diagnosed with a sensitivity of 94%; combined with EUS, the sensitivity of identifying insulinomas in one study was 100%. Gastrinomas, like insulinomas, tend to be small at presentation and are more difficult to find when they are present in extrapancreatic locations. They often do not alter the contour of the pancreas. As described earlier, 90% of gastrinomas are found within the gastrinoma triangle and careful attention should be given to this area during imaging review. Other functioning tumors, namely VIPomas, somatostatinomas, and glucagonomas, as well as nonfunctioning neuroendocrine tumors of the pancreas, are often easier to identify because they commonly present as large, malignant lesions. They tend to show central necrosis, discrete nodular calcifications, and cystic areas. Unlike pancreatic adenocarcinomas, PNETs are hypervascular tumors and rarely cause ductal obstruction.
MRI can play a complimentary role to CT imaging, particularly for small tumors. Relative to the pancreas, PNETS frequently present as low-intensity lesions on T1-weighted sequences and high-intensity lesions on T2-weighted sequences ( Fig. 2 ). MRI has been effective at identifying PNETs with a sensitivity of about 93% (range, 85%–100%) and a specificity of about 88% (range, 75%–100%) among 7 studies. Magnetic resonance cholangiopancreatography can be included for the local assessment of PNETs to evaluate the relation of the tumor to the pancreatic and main bile duct.
EUS should be performed in every patient in whom minimally invasive surgery is recommended. EUS provides useful anatomic information that may influence the operative plan, especially pertaining to the pancreatic ductal and vascular anatomy. Fine-needle aspiration can be readily performed if indicated to assist with PNET diagnosis; this is especially helpful in the setting of multifocal disease. Similar to MRI, one of the benefits of EUS is the lack of patient exposure to radiation. Ultrasonography can now be performed with intravenous contrast enhancement using microbubbles, which can be highly effective in depicting smaller tumors, and provides a method to perform needle biopsies for diagnosis, if needed. The first study to report the efficacy of EUS in localizing PNETs was done in 1992 by Rösch and colleagues, showing a sensitivity and specificity of 82% and 92%, respectively, among 50 patients. EUS is particularly useful for identification of small pancreatic tumors as small as 2 to 5 mm, particularly insulinomas and gastrinomas. Despite the various benefits of EUS, it is a more invasive form of imaging study than the other modalities already listed and is highly operator sensitive.
PET imaging has been gaining popularity but may be difficult to obtain because most third party payers do not reimburse for PET scanning. Although the use of PET imaging is controversial, there is emerging evidence that increased intensity, and therefore glucose metabolism, in PNETs indicates a higher likelihood of tumor invasion and metastasis, and poorer prognosis. One study showed that most patients with PET-positive lesions also had early progressive disease. Although not yet conclusive, PET imaging may play an important role in the future in predicting outcomes and management of PNETs.
Patient Selection and Choice of Procedure
Surgical resection is the only curative treatment of patients with PNETs. Surgery may also alleviate symptoms from hormonal production of functioning tumors or symptoms caused by the mass effect frequently seen with nonfunctioning tumors. The planned surgical procedure is mainly mandated by the preoperative localization studies, but it may change according to intraoperative findings. No consensus has been established regarding the indications of minimally invasive surgery for the treatment of PNETs; however, the presence of a malignant PNET could represent a relative contraindication for a minimally invasive approach. Laparoscopic surgery for small and solitary PNETs is feasible and safe. Laparoscopic enucleation is generally recommended in well-circumscribed lesions smaller than 3 cm, with noninvasive features and a peripheral location without involvement of the main pancreatic duct. If the tumor is in close proximity to the main pancreatic duct, enucleation is not recommended in light of its high incidence of pancreatic fistula.
Solitary insulinomas are particularly amenable to laparoscopic enucleation because of their small size and benign nature. Intraoperative laparoscopic ultrasonography is routinely performed to confirm tumor location and its relationship to the pancreatic duct and peripancreatic vessels, in order to plan the margin of resection before enucleation ( Fig. 3 ). If enucleation is not possible, a formal pancreatic resection is recommended. In tumors involving the head of the pancreas, pancreaticoduodenectomy is indicated. Pancreaticoduodenectomy has proved to be among the most complex procedures in general surgery, with high rates of morbidity and mortality. However, many studies have shown the effectiveness and safety of this procedure when performed through minimally invasive techniques in high-volume institutions by experienced surgeons.
In tumors that are located in the body or tail of the pancreas, which are not amenable for enucleation, laparoscopic distal pancreatectomy (LDP) is the procedure of choice. There are 3 variations of the distal pancreatectomy: spleen-preserving distal pancreatectomy with splenic vessel preservation, spleen-preserving distal pancreatectomy without splenic vessel preservation, and distal pancreatectomy with splenectomy. The anatomic relationship between the tumor within the pancreatic body or tail and the splenic vessels and hilum are factors that determine the appropriate procedure to perform. In addition, the presence or suspicion of a malignant tumor favors a more aggressive approach.
Surgical technique
Enucleation (Head)
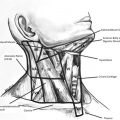
Once the laparoscopic ports have been placed, exposure of the pancreas is accomplished by opening the gastrocolic ligament, thereby gaining access to the lesser sac. Subsequently, intraoperative laparoscopic ultrasonography is performed to help accurately localize the tumor, rule out the presence of additional lesions, and to identify the exact location of the tumor and its relation to the pancreatic duct and major vessels. Special care is taken to avoid injury to the pancreatic duct and the mesenteric/splenic vessels during the dissection. The use of a combination of blunt dissection, electrocautery, and high-energy cautery devices are recommended to perform the enucleation. Bleeding is common during enucleation ( Fig. 4 ). A drain is almost routinely left in the surgical bed.
Enucleation (Body and Tail)
Laparoscopic ports are placed and laparoscopic ultrasonography is performed for tumor localization and its relationship with surrounding structures. The spleen is mobilized superiorly and laterally while the splenic flexure is taken down inferiorly. When the tumor is located anteriorly, an opening is created in the anterior visceral peritoneum of the pancreas and careful dissection is performed between the tumor and the normal pancreatic parenchyma until successful enucleation of the mass is accomplished. For tumors located in the posterior aspect of the pancreatic body or the tail, the inferior margin of the pancreas is dissected and the pancreas is mobilized and lifted up, allowing exposure of the posterior pancreatic surface ( Fig. 5 ). After enucleation, the tumor bed must be examined for any evidence of pancreatic duct injury. Tumors located in the distal portion of the tail of the pancreas are in close proximity to the pancreatic duct. Therefore, if in doubt about potential ductal injury, a distal pancreatectomy should be performed.
Laparoscopic Distal Pancreatectomy (Spleen-preserving with Splenic Vessel Preservation)
When possible, spleen-preserving distal pancreatectomy with splenic vessel preservation is performed for distal tumors; however, this procedure requires more advanced technical expertise, with separation of the splenic vessels from the pancreatic parenchyma (see Fig. 5 ), and division of the branching vessels supplying the pancreas. As a result, this procedure is associated with a longer operating time. The pancreatic tail is exposed as described earlier. Special care is taken to preserve the short gastric and the left gastroepiploic vessels. After mobilizing the inferior margin of the pancreas, the pancreas is mobilized and lifted up, allowing exposure of the posterior pancreatic surface (see Fig. 5 ).
At this time, the superior mesenteric vein (SMV) and the splenic vein can be identified forming the portal vein ( Fig. 6 ). Blunt dissection around the splenic vein is performed, with ligation of the small tributaries coming from the pancreas. After identification and preservation of the splenic artery, the pancreas is divided to the left of the SMV using an endoscopic stapler device. The body/tail of the pancreas is then anteriorly retracted, allowing separation of remaining small bridging vessels between the pancreas and the splenic vessels. The resection is completed after reaching the splenic hilum. A surgical drain is left in the surgical bed in proximity to the pancreatic stump.
Laparoscopic Distal Pancreatectomy (Spleen-preserving Distal Pancreatectomy Without Splenic Vessel Preservation)
This procedure follows the same course mentioned earlier until obtaining visualization of the posterior aspect of the pancreas and the confluence of the splenic vein and SMV.
At this time, the splenic vein and artery are clipped and ligated. The pancreas is then divided with an endoscopic stapler. The pancreatic body and tail are retracted upwards (along with the attached splenic artery and vein), and the vessels between the pancreatic tail and the splenic hilum are clipped and divided. Blood supply to the spleen depends on the short gastric and left gastroepiploic vessels; therefore, special care is taken to preserve these vessels; this is crucial for the success of this procedure.
Laparoscopic Distal Pancreatectomy with Splenectomy
This procedure is similar to the previous technique (spleen-preserving distal pancreatectomy without splenic vessel preservation) with a few exceptions. Unlike in spleen-preserving procedures, the short gastric and left gastroepiploic vessels can be ligated. In addition to mobilizing the splenic flexure, the lateral attachments of the spleen are divided up to the left crus of the diaphragm, allowing medialization of the spleen. The splenic vessels can be divided separately if an easy plane of dissection is encountered or along with the pancreas if separation of the vessels is difficult. The specimens are removed en bloc from the abdominal cavity in an endoscopic specimen bag. A surgical drain is left in the surgical bed in proximity to the pancreatic stump.
Laparoscopic Central Pancreatectomy
The initial dissection is performed laparoscopically through 5 trocars. Once the anterior surface of the gland is cleared from the head distal to the lesion, a tunnel over the portal vein is created. The lesion is resected with an endoscopic stapler on the proximal margin and cautery on the distal margin with care to avoid thermal injury to the duct. The reconstruction is then performed via a pancreaticogastrostomy or with Roux-en-Y pancreaticojejunostomy reconstruction.
Laparoscopic Pancreaticoduodenectomy
One of the largest series of laparoscopic pylorus-preserving pancreaticoduodenectomy comes from 100 consecutive cases performed in Korea. In their first 10 cases, reconstruction was partially performed extracorporeally, whereas the last 90 cases were performed completely intracorporeally. The patient was positioned supine with the surgeon on the patient’s right and the assistant and scrub technician on the left. The operator ports were placed in the right flank area and 1 near the umbilicus with a camera placed in between in the right lower quadrant. Assistant ports were placed in the left flank area.
After evaluation of the abdomen, the gastrocolic omentum was dissected to allow entry into the lesser sac. The hepatic flexure was mobilized and the duodenum was kocherized. The pancreatic dissection began at the inferior border and was continued over the retropancreatic portal vein. The duodenum was mobilized to the ligament of Treitz and the duodenum was transected 2 cm distal to the pylorus. Next, the common bile duct was isolated within the hepatoduodenal ligament. A cholecystectomy was performed separately. The common bile duct was divided and the common hepatic artery was dissected from the pancreas. The gastroduodenal and right gastric arteries were transected with 2 titanium clips and the pancreas was divided at the neck with an endoscopic linear stapler or Harmonic scalpel. With retraction of the pancreatic head toward the right side of the patient, the intrapancreatic portal vein was dissected. The jejunum was divided 10 to 15 cm distal to the ligament of Treitz with another load of the endoscopic stapler. An endoscopic linear stapler or ultrasonic shears was used to divide the soft tissue and arterial branches between the superior mesenteric artery and the uncinate process to complete the resection.
For totally intracorporeal laparoscopic pancreaticoduodenectomy (LPD), a pancreaticojejunostomy was performed using the double-layered, end-to-side dunking method in normal-sized ducts or using the duct-to-mucosa method in dilated pancreatic ducts. An intracorporeal laparoscopic choledochojejunostomy was performed using interrupted absorbable sutures and an extracorporeal knot pusher in the initial cases and continuous suturing for later cases, except for very small ducts. An internal stent was used if the diameter of the common bile duct was too small. Duodenojejunostomies and jejunojejunostomies were performed intracorporeally or extracorporeally using the specimen extraction site from the umbilical port site. Closed suction drains were placed near the pancreaticojejunostomy and choledochojejunostomy sites.
Robotic Surgery
Robotic systems were first introduced in the late 1990s, and since then the popularity and number of robotic procedures has increased exponentially. Since its first reported application in 2003, the appeal of robotic pancreatic surgery has increased. The most popular robotic-assisted minimally invasive surgical platform (da Vinci system, Intuitive Surgical, Sunnyvale, CA) offers multiple advantages, such as, a three-dimensional high-definition view with significant magnification of the surgical field; elimination of tremor with improved dexterity, particularly with the use of articulating instruments that provide 540° range of motion; stereotactic binocular visualization; and improved surgeon comfort.
Most series reporting their experience of robotic surgery describe similar techniques to those listed earlier through the laparoscopic technique. Zeh and colleagues reported their series of 51 robotic-assisted pancreaticoduodenectomies performed at the University of Pittsburgh, 9 of which were performed for neuroendocrine tumors. They emphasized the importance of teamwork in obtaining a successful outcome. They also admitted to several limitations of robotic surgery compared with standard laparoscopic surgery, including the difficulty of working in multiple abdominal quadrants with the robot; frequent collisions between the arms of the robot caused by their large size and suboptimal positioning; the inability to change the position of the table once the robot is docked, preventing gravity from being used as a retractor of viscera; and the lack of tactile feedback. Future generations will potentially address some of these issues, thus improving the flow of robotic-assisted surgery.
Radiofrequency Ablation for Pancreatic Neuroendocrine Tumors
With the goal of developing less invasive techniques, the use of radiofrequency ablation (RFA) has been proposed for the treatment of PNETs, because it has been applied for the treatment of adenocarcinomas of the pancreas. More specifically, the use of RFA has been proposed in those patients with PNETs who are ineligible for surgical resection. Radiofrequency ablation can be performed percutaneously under ultrasonography guidance or intraoperatively. The available experience on this procedure is limited and the evidence has been documented in a recent study. The use of RFA is associated with known adverse effects, which include thermal-induced pancreatitis as well as potential injuries to surrounding tumor structures such as the duodenum, pancreatic duct, and major blood vessels.
In the only prospective pilot study currently available, the use of RFA in selective PNETs has shown encouraging results. The study included 10 patients (7 women and 3 men) aged 38 to 75 years old, with 3 functioning PNETs (1 gastrinoma and 2 insulinomas) and 7 nonfunctioning PNETs. Tumor size ranged from 0.9 to 2.9 cm in diameter. Selective criteria to receive treatment with RFA included patients with pathologically confirmed PNETs, those patients ineligible for or who refused surgery, single tumors less than or equal to 3 cm in diameter, and tumor location greater than 1 cm from the wall of the stomach, intestine, or bile ducts. The ultrasonography-guided RFA was performed percutaneously in 7 cases, endoscopically in 1, and intraoperatively in 2 patients.
Endoscopic Ultrasonography-directed Alcohol Ablation
Ethanol ablation has also been used as a treatment modality for PNETs. Ethanol has gained interest as an ablative agent because it is inexpensive and readily available. Alcohol ablation works by causing coagulation necrosis of the tumor as a result of cellular dehydration, protein denaturation, and vascular occlusion. Major limitations of alcohol ablation include the possibility of late recurrence, incomplete ablation, and risk of progression during follow-up. As with RFA, ethanol ablation has the potential to cause acute pancreatitis. In a pilot study performed on 11 patients with 14 tumors by a group in Korea, 3 patients developed postoperative pancreatitis. Seven (54%) of the 13 tumors responded to treatment, with the remainder showing residual viable enhancing tissue at 3-month radiologic imaging follow-up.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree