Figure 2.1
Preoperative imaging in a patient with primary hyperparathyroidism. (a) High-resolution ultrasound identified a likely parathyroid adenoma between the left thyroid lobe and the left carotid artery. (b) Planar images from a sestamibi scan fail to convincingly localize a parathyroid adenoma. (c) SPECT-sestamibi images from the same patient at 15 min suggest a left lower parathyroid adenoma and agree with the ultrasound findings in (a). (d) Delayed SPECT-sestamibi images at 90 min show washout in the thyroid and enhancement of the parathyroid adenoma, convincingly localizing a left inferior parathyroid adenoma
2.2.2 Surgical Procedures
After the patient’s identity is confirmed and the operative site is marked, the patient is brought to the operating room. Most often, the procedure is done under general anesthesia, which results in patient comfort and an overall shorter operative procedure. After the induction of adequate general anesthesia, the patient is positioned with a roll behind the shoulders, with the neck in slight extension (Fig. 2.2). The arms should be tucked, allowing better access to the neck and shoulder area during the surgical procedure. A small transverse incision of approximately 2–3 cm is made sharply with a scalpel. The electrocautery setting should be at pure cut, at the lowest setting that allows efficient transection of tissues. Using electrocautery, dissection is carried down through the platysma muscle while avoiding transection or injury of deeper structures (Fig. 2.3). Using skin hooks to elevate the skin, a subplatysmal flap is developed, leaving the anterior jugular veins, strap muscles, and sternocleidomastoid muscles undisturbed. The platysma and subcutaneous tissue are retracted with a self-retaining retractor. The strap muscles are divided at the midline, exposing the thyroid lobe on the side where the adenoma was localized (Fig. 2.4). Retraction of the strap muscles is performed and dissection is carried out to mobilize the strap muscles off the mid-neck structures. A Babcock clamp is placed on the thyroid lobe after division of the middle thyroid vein, mobilizing the thyroid up into the incision (Figs. 2.5 and 2.6). Retraction of the thyroid allows for better exposure of the deeper structures and often helps mobilize the parathyroid gland up into the incision (Figs. 2.5 and 2.6b). The carotid artery should be identified by palpation but is not necessarily exposed. An appendiceal or lateral retractor is used to retract the carotid artery laterally, opening up the mid-neck space.
Anatomic dissection within the mid-neck space is directed by the preoperative imaging. An inferior parathyroid gland is usually found anterior and medial to the course of the recurrent laryngeal nerve and lateral or inferior to the edge of the thyroid. A superior parathyroid gland is often further posterior, and is most commonly superior and slightly lateral to the course of the recurrent nerve. Often the nerve is identified and exposed during the course of the dissection. Care should be taken to move neck structures away from the nerve, to leave the nerve undisturbed and along its normal course in the neck. Some surgeons employ nerve monitoring, but the routine use of nerve monitoring has not been shown to decrease the nerve injury rate [5]. The parathyroid adenoma, once identified, is mobilized using sharp and blunt dissection. Fibrous attachments are cut using monopolar electrocautery. The gland should be mobilized until it is attached by its pedicle. The pedicle is clamped, transected, and ligated with a 3-0 silk suture. The parathyroid adenoma is sent to pathology and frozen section is used to confirm the presence of hypercellular parathyroid tissue. Surgeons often omit the frozen section step, but ectopic thyroid tissue or enlarged lymph nodes could potentially be resected inadvertently, and frozen section can help to ensure that the parathyroid adenoma was removed.
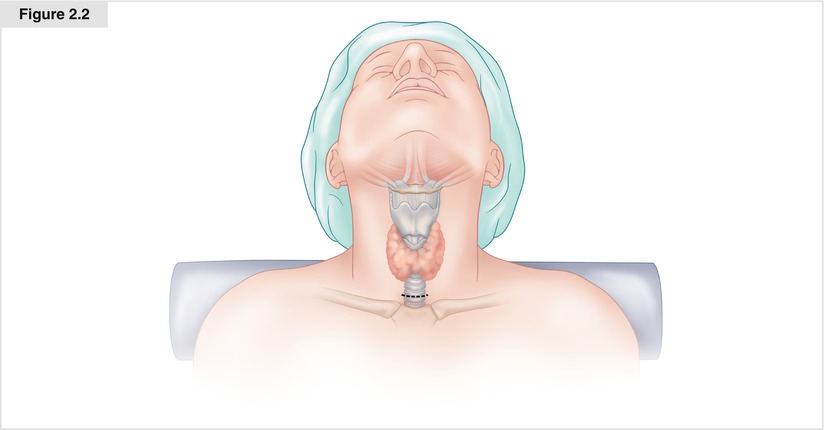
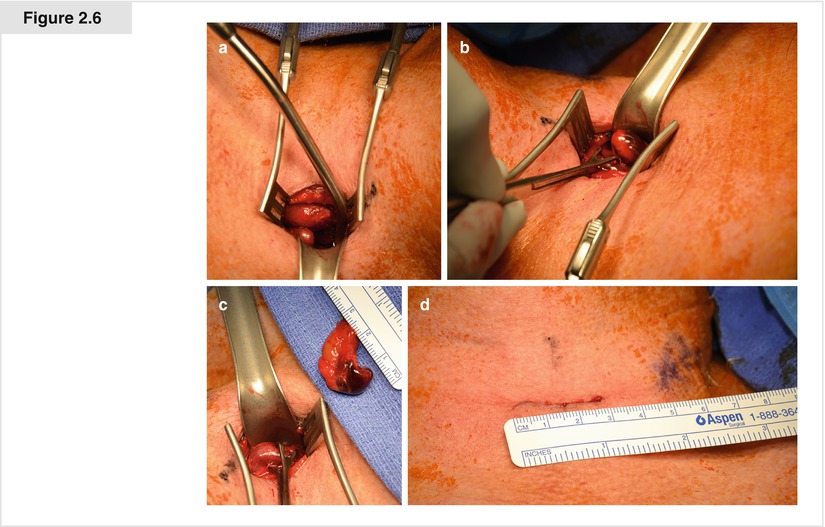
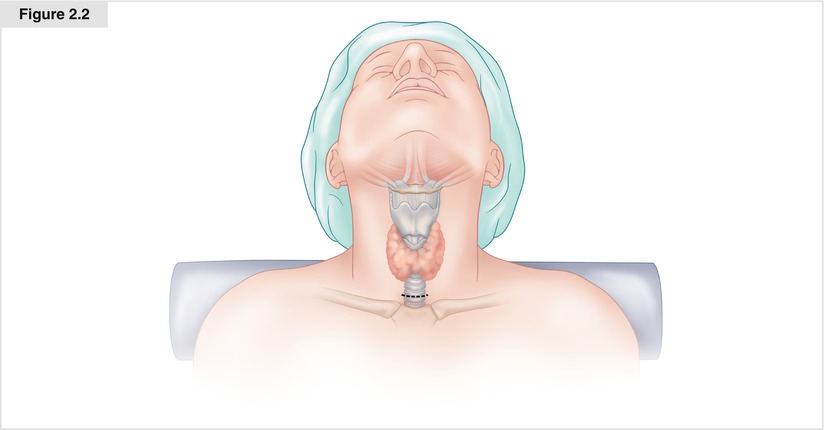
Figure 2.2
Positioning a patient for minimally invasive parathyroidectomy (MIP). The patient is positioned with a roll behind the shoulders to place the head in slight extension. A 2- to 3-cm incision is made approximately 1–2 cm above the sternal notch
Figure 2.3
Developing a subplatysmal plane. The skin and subcutaneous tissue are retracted using skin hooks. Using electrocautery, the platysma is dissected off the strap muscles. After developing a superior and inferior flap, the platysma is retracted with a self-retaining retractor
Figure 2.4
Mobilization of the strap muscles. The strap muscles are mobilized off the mid-neck structures, exposing the thyroid lobe on the side localized by preoperative imaging.
Figure 2.5
Mobilization of the thyroid and resection of the parathyroid adenoma. The thyroid lobe is retracted into the incision, exposing the deeper mid-neck structures. The parathyroid adenoma is identified by sharp and blunt dissection in the mid-neck space. The adenoma is mobilized and resected
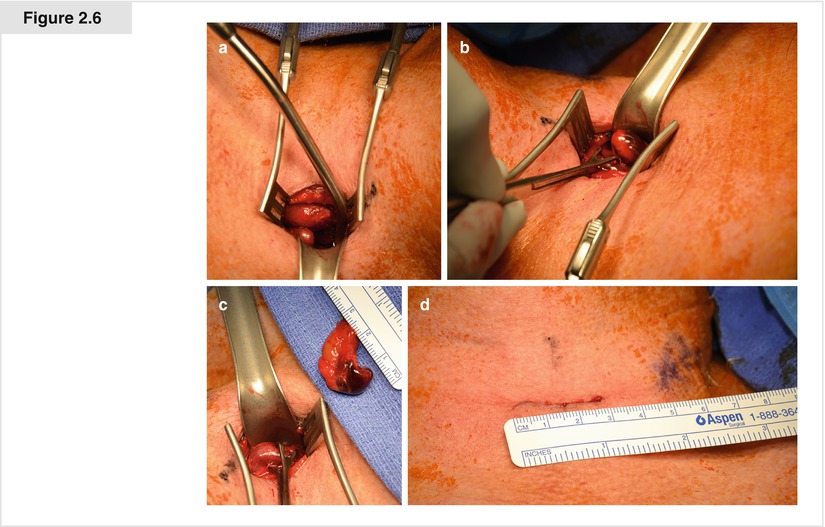
Figure 2.6




Example of an MIP operation. These operative photographs show successful MIP in the patient whose preoperative localization studies are shown in Fig. 2.1. (a) After retraction of the strap muscles, the left mid-neck structures are exposed and the parathyroid adenoma is identified. (b) The parathyroid adenoma is being mobilized. (c) The adenoma is resected; a Babcock clamp is seen on the thyroid lobe. (d) The incision is closed, completing successful MIP via an incision slightly less than 3 cm. The baseline intraoperative parathyroid hormone (IOPTH) in this patient at the time of neck incision was 137 pg/mL. The level 10 min after the adenoma was resected completely (c) was 31 pg/mL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree