Primary hyperparathyroidism is a disease that is caused by excess parathyroid hormone (PTH) secretion from 1 or more of the parathyroid glands. Surgery is the only cure. Traditional surgical management consists of a 4-gland cervical exploration. Development of imaging specific to identification of parathyroid glands and application of the rapid PTH assay to operative management have made more minimal exploration possible. There are distinct advantages and disadvantages of minimally invasive parathyroidectomy (MIP) and bilateral neck exploration (BNE). The advantages of MIP seem to outweigh those of BNE, and MIP has replaced BNE as the operation of choice by many surgeons.
Key points
- •
The gold-standard surgical management of primary hyperparathyroidism (1 0 HPT) is cervical exploration and identification of all 4 parathyroid glands.
- •
Imaging techniques, including ultrasound, sestamibi scans, and 4D-CT scans, have made identification of single parathyroid adenomas possible.
- •
Intraoperative parathyroid hormone (PTH) monitoring is a method to confirm biochemical cure before a patient leaves the operating room.
- •
There is some debate surrounding optimal surgical management of 1 0 HPT because cure rates between minimally invasive parathyroidectomy (MIP) and bilateral neck exploration (BNE) are equivalent.
- •
Advantages of MIP include reduced operative time, reduced recovery time, less postoperative pain, and lower complication rate with respect to injury to parathyroid glands and recurrent laryngeal nerves.
Introduction
1 0 HPT is a common disease, with a prevalence as high as 3%. Many advances in the surgical management of 1 0 HPT have been made since the first parathyroidectomy was performed by Felix Mandl in 1925. Traditional surgical management consists of identification of all 4 parathyroid glands through a transverse cervical incision. Better understanding of the disease, interest in the practice of endocrine neck surgery, and operative experience increased cure rates to greater than 95%. Surgery remains the only cure for 1 0 HPT because medical management ultimately fails.
As in other areas of surgery, there has been a shift from the standard 4-gland exploration to a more minimally invasive approach. The success rate of MIP rivals that of BNE. Questions remain as to which approach is better. This primarily depends on proved benefit of each operation over its shortcomings. With MIP, incisions are smaller and recovery time is improved, but these may be achieved at the cost of higher rates of persistence or recurrence. BNE may be less advantageous because MIP may achieve a similar outcome with fewer complications. This article seeks to define MIP and BNE and to compare them for advantages and disadvantages.
Patient evaluation
A diagnosis of 1 0 HPT is made when the serum calcium level is elevated in the setting of an inappropriately nonsuppressed PTH level. This results from overproduction of PTH by 1 or more of the parathyroid glands. The incidence of 1 0 HPT is increasing overall as the population in the United States has aged, with incidence rates ranging from 0.7% in the general population up to 3% in postmenopausal women. 1 0 HPT occurs at a higher rate in women, at a 2:1 ratio, and is the most common cause of hypercalcemia in the outpatient population. Overall rates of hypercalcemia have also increased as a result of a change in the calcium assay in the 1970s, leading to earlier diagnosis of hypercalcemia. Thus, the presentation of symptomatic 1 0 HPT changed from a disease that was typically associated with kidney stones and skeletal disease to one that is asymptomatic. Associated symptoms may include fatigue, polydipsia, polyuria, depression, generalize muscle weakness, joint pain, memory loss, nausea, and loss of appetite, although these subtle symptoms are often found in the general population as well.
Hypercalcemia may occur as a result of other conditions, such as malignancy, sarcoidosis, hyperthyroidism, and use of thiazide diuretics, and the diagnosis of 1 0 HPT involves a comprehensive evaluation to eliminate these conditions as a cause for hypercalcemia. 1 0 HPT results in an overproduction of PTH, which stimulates bone reabsorption, stimulates the production of vitamin D, inhibits renal excretion of calcium, and stimulates intestinal reabsorption. Typically, PTH and its relationship to serum calcium levels function in a negative feedback loop, where, once the calcium-sensing receptor in the parathyroid gland perceives adequate levels of PTH, hormone production ends. In 1 0 HPT, both serum calcium and PTH are elevated, or PTH is abnormally elevated relative to serum calcium level. This then differentiates it from other conditions, such as malignancy, benign familial hypocalciuric hypercalcemia, vitamin D deficiency, and sarcoidosis, where either calcium or PTH may be elevated independently. Careful interpretation of calcium levels relative to PTH levels is necessary because the laboratory findings may be subtle as in cases of normocalcemic hyperparathyroidism and normohormonal hyperparathyroidism.
Indications for surgical management of 1 0 HPT are outlined in consensus group guidelines written originally in 1990 and updated most recently in 2013.
The most current international consensus guidelines recommend surgery if any of the following criteria are met: age less than 50; calcium elevated to greater than 1 mg/dL above the upper limit of the normal range; reduced bone mineral density with T-score less than −2.5 at lumbar spine, total hip, femoral neck, or distal radius; creatinine clearance less than 60 mL/min; 24-hour urine calcium greater than 400 mg/d and increased stone risk by biochemical stone analysis; and presence of nephrolithiasis or nephrocalcinosis by imaging ( Table 1 ). Additionally, patients who prefer surgery or are unable or unwilling to commit to follow-up should undergo parathyroidectomy.
| Criterion | Indication for Surgery |
|---|---|
| Age | <50 |
| Calcium | >1 mg/dL above upper limit of normal range |
| BMD |
|
| Renal |
|
Surgical treatment options
Minimally Invasive Parathyroidectomy
Like many other surgical techniques, the approach to parathyroidectomy has evolved. Although traditional parathyroidectomy includes a transverse cervical incision and identification of all 4 parathyroid glands, a minimally invasive approach is performed through a limited incision with the goal of removing the preoperatively localized abnormal gland. A high degree of success is achieved as a result of both careful preoperative planning and because 85% of patients have a single parathyroid adenoma. MIP may have more than 1 meaning, however. MIP is most traditionally thought of as a parathyroidectomy done as a unilateral or focused neck exploration (FNE). Through a 2.5-cm transverse cervical incision, the preoperatively localized parathyroid adenoma is removed. Dissection is focused at the anatomically localized site. The procedure may be done under local or general anesthesia and is typically done as outpatient surgery. Success of surgery is confirmed biochemically by intraoperative PTH (IOPTH) monitoring. MIP may also mean minimally invasive video-assisted parathyroidectomy (MIVAP) or robotic-assisted parathyroidectomy, although FNE is the most widely applied technique. The majority of this discussion thus focuses on FNE. I 0 PTH monitoring and application of imaging techniques in patients with 1 0 HPT have made FNE possible.
The short half-life of PTH, ranging from 3 to 5 minutes, has made IOPTH monitoring a useful adjunct to parathyroid surgery, confirming a biochemical cure during operation. A rapid immunoradiometric assay was developed in 1987 and was successfully applied during parathyroidectomy in a small series of patients. These investigators suggested that a more limited approach might be taken in the surgical management of 1 0 HPT. Other groups applied the rapid assay routinely, and the FNE became a more widely accepted operation. Subsequently, criteria for interpretation of IOPTH results were developed. A PTH level is sampled at the outset of parathyroidectomy; levels are then obtained at timed intervals after removal of the adenoma. Initially implemented at the University of Miami, other criteria have been used by different groups. Biochemical cure is established when PTH falls by at least 50% of the highest pre-excision level and into the normal PTH range ; failure to do so may miss multigland disease. The critically important step of application of IOPTH is to use the same technique at each operation; use of a varied technique makes interpretation of results difficult and may lead to persistent disease. In cases of IOPTH not falling appropriately, the operation is converted to a BNE.
Imaging studies are used in the operative planning of FNE and are not used to make or confirm the diagnosis of 1 0 HPT. Instead, a decision is made to operate and subsequently localization studies are obtained. As the interventional radiologist John Doppman stated, “The only localization that a patient needs who has 1 0 HPT is the localization f an experienced surgeon.” There are multiple imaging modalities, however, available to the surgeon who plans FNE.
Sestamibi scintigraphy was the earliest routinely applied imaging modality in operative planning of FNE. Technetium 99m sestamibi is thought to be retained in the mitochondria of parathyroid adenomas, making visualization possible. Sestamibi localizes parathyroid adenomas in up to 90% of patients but may be unrevealing in patients with multigland disease or with small adenomas. Multidimensional imaging with the addition of single-photon emission CT (SPECT) to sestamibi scintigraphy improves sensitivity ( Fig. 1 ). False-positive studies may be a result of concomitant thyroid nodules or lymphadenopathy, and the addition of a second imaging tool, such as ultrasound, may improve identification of abnormal glands. Sestamibi-SPECT may be most useful in the identification of ectopic adenomas, such as those in the mediastinum.
Ultrasound is commonly used for localization of adenomas. Ultrasounds are portable, often available in a surgeon’s or endocrinologist’s office, do not expose patients to radiation, and cost less than nuclear medicine or multidimensional studies. The accuracy is similar to that of sestamibi-SPECT, at 70% to 80%. Concomitant thyroid pathology, including benign nodules and thyroid cancer, is identified on ultrasound in 30% to 50% of patients with 1 0 HPT, and ultrasound-guided fine-needle aspiration also may be used to aspirate suspected adenomas for PTH. When combined with sestamibi-SPECT, accuracy of localization of an adenoma increases to approximately 90%. Series demonstrate that concordant sestamibi-SPECT and ultrasound have operative cure rates of 98% to 99%, suggesting that this may be an alternative to IOPTH monitoring. The typical appearance of a parathyroid adenoma is shown in Fig. 2 .
High-resolution CT with and without intravenous contrast (4D-CT) and MRI can demonstrate parathyroid adenomas due to their contrast washout ( Fig. 3 ). 4D-CT is more sensitive than both ultrasound and sestamibi-SPECT for identification of adenomas and may be useful to detect multigland disease. MRI is an option for localization, although it is the least commonly used; this modality is best used in cases of reoperative parathyroidectomy.
Additional techniques for MIP include radioguided parathyroidectomy (RP), MIVAP, and robotic-assisted parathroidectomy. Like FNE, RP is an ambulatory procedure. Preoperatively patients are injected with technetium 99m sestamibi approximately 2 hours before the procedure, and a scan is performed the day of surgery. In the operating room, a gamma probe is used to measure activity of the excised tumor compared with the central neck. IOPTH may be additionally used to confirm biochemical success. MIVAP uses a small scope that is inserted through the primary incision or a separate trochar to remove the preoperatively localized adenoma. There is more than 1 described technique to this approach with similar success rates. Robotic assistance may be added to an endoscopic technique or used alone. Compared with FNE, MIVAP and robotic procedures add operative time and complexity as well as an increased cost. Although groups have achieved outcomes comparable to FNE, they are done in high-volume centers with a focus on these endoscopic and robotic procedures. The authors prefer FNE because it is a procedure applicable across different practice types.
Bilateral Neck Exploration
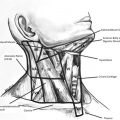
BNE is the traditional operation for 1 0 HPT and was the only option prior to the development of IOPTH testing and reliable of imaging studies. The surgical technique is essentially the same as MIP, although the operation is typically done through a larger incision, at a minimum of 3 cm. Parathyroid glands are identified by the operating surgeon as abnormal if they are either larger than typical size of 30 to 50 mg or have abnormal morphology. Most glands are identified in the expected anatomic location ; if not, the gland may be ectopic. The exploration then continues in the typical locations for ectopic parathyroid glands, including the thymus, anterior mediastinum, the tracheoesophageal groove and retroesophageal space extending into the posterior mediastinum, the carotid sheaths, and lastly the thyroid gland. All glands should be identified before any are removed. Excision may involve removal 1 to 3.5 glands, as described previously. IOPTH may be used as an adjunct to BNE and levels are interpreted in the same manner as in MIP to confirm biochemical cure.
BNE may be indicated rather than FNE in specific situations. Patients in whom FNE is intended but have negative imaging studies need to undergo 4-gland exploration. The risk of multigland disease is as high as 25% in these patients. Additionally, patients who have conditions in which multigland disease or multiple adenomas are expected should have BNE. These include multiple endocrine neoplasia (MEN) types 1 and 2a, familial 1 0 HPT, and lithium-induced hyperparathyroidism. Up to 90% of patients with MEN1 and 30% of patients with MEN2a have multiple adenomas in any of the 4 parathyroid glands and thus benefit from BNE. In patients predisposed to multigland disease, debulking abnormal glands rather than resection to achieve cure should be the goal, because MEN is a lifelong condition. Long-term lithium therapy may cause hyperparathyroidism; because it is a systemic therapy it may affect all 4 glands. Series demonstrate that more than half of patients treated with lithium have 1 0 HPT and benefit from BNE if treated operatively.
Surgeon preference may dictate the choice of BNE over FNE. This is a result of some published evidence that there is a higher failure rate of FNE, and that unilateral exploration may fail to identify multigland disease even with the addition of IOPTH. Some have reversed their preference of FNE versus BNE, stating that the rates of persistence and recurrence are unacceptably high; however, IOPTH was not used in this cohort. Furthermore, data suggest that BNE is more time-efficient in patients who do not localize preoperatively.
Comparison of focused neck exploration to bilateral neck exploration
In the United States, there is a trend toward the performance of FNE. Moreover, there is a trend in surgical training programs toward surgeon-performed ultrasound, use of IOPTH, and FNE. Thus, it is important to understand the differences in and outcomes of FNE and BNE.
Outcomes
Generally, both FNE and BNE are low-risk procedures associated with good outcomes. Complication rates overall are similar, likely because large published series are performed by high-volume surgeons. In a series of 184 patients who underwent FNE, the rate of persistent disease was 1.6%, permanent hypocalcemia 0.5%, and permanent vocal cord paralysis 1%. This is similar to other groups, with reported persistence rate of 1.5%, recurrence 6%, and permanent hypocalcemia 0.02%. In comparison, traditional BNE outcomes are also good, with rate of persistent disease of 6%. The rates of multigland disease in these reports were higher in patients who underwent BNE versus FNE (10% vs 3%) due to surgeon evaluation of abnormal-appearing glands. Similarly, other series have reported overall complication rates of up to 3%, including recurrent laryngeal nerve injury, postoperative hypocalcemia, and neck hematoma. Data from the endocrine surgery group at Yale University reveal that cure rates are improved with FNE versus BNE at 1.45% versus 3.1% with similar low rates of permanent hypocalcemia and recurrent laryngeal nerve injury. Additional series have compared these techniques through either randomized or retrospective data with similar findings. These results are compared from selected series in Table 2 .
| Series | Study Type | Outcome |
|---|---|---|
| Westerdahl & Bergenfelz, 2007 | Randomized | = Cure rate at 5 y |
| Bergenfelz et al, 2002 | Randomized | = Cure rate; increased cost and operative time in FNE; increased postoperative hypocalcemia with BNE |
| Slepavicius et al, 2008 | Randomized | = OR time and cure rate; increased cost with FNE; increased postoperative hypocalcemia with BNE |
| Aarum et al, 2007 | Randomized | = Cure rate; = complication rate; increased cost with FNE |
| Grant et al, 2005 | Retrospective | = Cure rate; = complication rate |
| Udelsman et al, 2011 | Retrospective | Increased cure rate and lower complication rate with FNE |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree