Step
Action
1
Insert endoscope
2
Dilate to 16 m with balloon dilator, if necessary
3
Place hemoclip 2 cm at planned distal end of stent
4
Insert wire and remove endoscope
5
Under fluoroscopic guidance, place stent over wire and advance distal end to hemoclip
6
Reintroduce endoscope and confirm placement
Stent placement has been shown to improve dysphagia scores immediately post-procedure, thus allowing patients to increase their oral nutritional intake. Over time, patients demonstrate weight gain [8], better tolerance of neoadjuvant therapy, and improvement in quality of life [9] (Table 17.2). In addition, a significant proportion of patients do not proceed with resection following neoadjuvant therapy due to progression of disease. Placement of a stent as opposed to a feeding tube in this population avoids a more invasive procedure while improving overall quality of life [6]. Complications of stent placement include migration, erosion, perforation, esophageal spasm, and obstruction. Reintervention rate has been sited to range from 20 to 60 % most often for stent migration, but this is highly dependent on the type of stent placed [9]. Our recently completed prospective trial demonstrated a reintervention rate of 6 %, thus proving that with adequate length and outer diameter, reintervention rates can be minimal [4]. Overall, esophageal stenting is effective, more efficient, less invasive, with improved quality of life tolerance, and is the optimal way to improve both nutritional measures and overall outcomes in the management of esophageal cancer.
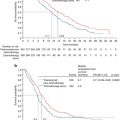
Table 17.2
Outcomes for esophageal stents during neoadjuvant therapy
Author | Date published | Number of patients | Complication rate (%) | Stent migration (%) | Dysphagia relief (%) | Success of therapy |
|---|---|---|---|---|---|---|
Langer et al. [9] | 2009 | 38 | 16 | 26 | 97.40 | Improved nutritional and dysphagia results |
Bower et al. [6] | 2009 | 25 | 4 | 24 | 100 | Improved nutritional result, tolerance of neoadjuvant therapy |
Siddiqui et al. [10] | 2009 | 12 | 22 | 60 | 100 | Improved dysphagia with similar nutrition outcomes |
Pellen et al. [11] | 2012 | 16 | 25 | 44 | 100 | Improved symptoms, maintenance of nutrition |
Brown et al. [4] | 2011 | 32 | 3 | 31 | 100 | Improved dysphagia, maintenance of performance status |
Lopes and Eloubeidi [12] | 2010 | 11 | 27 | 18 | 100 | Improved dysphagia |
Adler et al. [13] | 2009 | 13 | 0 | 46 | 100 | Improved dysphagia |
Enteral Access
Enteral access can be gained by placing a jejunostomy tube in either a percutaneous, laparoscopic, or open technique.
Percutaneous endoscopic jejunostomy (PEJ) tubes are placed in the endoscopy suite by the attending surgeon or gastroenterologist under IV conscious sedation. A variable pediatric colonoscope is the best endoscope for this procedure given the ability to variably make the scope stiffer with the adequate length needed to reach the proximal jejunum. The stomach and duodenum are traversed and the jejunum is insufflated and the site for tube placement is identified using transillumination and/or direct finger compression. The ideal location for tube placement is approximately 4 fingerbreadths below the left subcostal margin near the midclavicular line. This area is then prepped and draped and anesthetized with lidocaine. A 1 cm incision is made at the site and a needle is advanced into the jejunum under direct visualization perpendicular to the abdominal wall. The guidewire is then introduced through the needle and snared by the endoscope, which is then pulled back out of the patient’s mouth. The wire is disconnected from the scope and the PEJ tube is advanced over the wire until the wire can again be snared from the opposite end by the endoscope. The entire apparatus is again advanced into the pharynx through the esophagus into the stomach.
PEJ tube placement offers the advantage of an endoscopic procedure under conscious sedation, since most patients will require nutritional support during treatment, even if they are able to eat prior to initiating therapy. Potential complications of this procedure include injury to the bowel vessels, bleeding, infection, erosion, and bowel injury. In only a small number of patients will the esophageal tumors be so obstructive as to not allow passage of the endoscope. Overall, PEJ tubes are an option for enteral support of esophageal cancer patients, but should be used with caution. The current reported PEJ failure rate based on the inability to access the proximal jejunum is approximately 15–20 %.
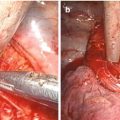
A laparoscopic jejunostomy tube is placed as an extension of the diagnostic laparoscopy with the use of one umbilical port and 2 additional 5 mm ports (Fig. 17.1). This procedure is performed under general anesthesia in the operating room (Table 17.3). Access to the abdomen is gained using a Hassan trocar in the midline with two more ports placed in the right upper quadrant under direct visualization. Visualization of the jejunum is achieved by adhesiolysis if needed and with the use of atraumatic bowel graspers to the location where the site for the J-tube placement is chosen. The jejunum is identified and followed backward to the ligament of Treitz, which commonly requires pulling the transverse colon caudally. A site for the jejunotomy is chosen 30–40 cm distal from the ligament of Treitz. The actual placement of the tube can be performed intracorporeally or extracorporeally. Three or four intracorporal 4-0 Vicryl or PDS sutures are placed circumferentially around the tube site using a laparoscopic suturing device (Fig. 17.2 and Video 17.3). A smaller catheter, 12–16 French, is passed through the abdominal wall using a stab incision and dissection with electrocautery. We prefer to use a T-tube. A jejunotomy is made, and the feeding tube is inserted into the enterotomy. The bowel is fixed to the abdominal wall at the site of the enterotomy using absorbable suture after the abdomen is desufflated. The tube is fixed to the skin with Nylon suture and all ports are closed [14]. An alternative method for laparoscopic feeding tube placement is demonstrated in Video 17.4.