Minimally invasive techniques have the potential to revolutionize the surgical management of pancreatic disease in the setting of benign and malignant processes. Pancreatic surgery, in particular, may be aided significantly by minimal access surgery given the high morbidity associated with traditional open pancreatic procedures. This article presents a review of two minimally invasive techniques for distal pancreatectomy and pancreaticoduodenectomy, focusing on metrics of technique, safety, morbidity, and oncologic outcomes and potential benefits.
Key points
- •
Open and minimally invasive approaches to pancreatic surgery for benign and malignant lesions have been shown to be equivalent in regards to their safety profiles in multiple large single institution series.
- •
Emerging multicenter data indicate that outcomes including morbidity/mortality, fistula occurrence, and overall survival are equivalent between the two distinct operative techniques.
- •
Laparoscopic and robotic surgical techniques have gained increasing acceptance over the last few years especially in the setting of pancreatic malignancy and may be associated with decreased patient hospital stays and comparable oncologic outcomes.
Introduction
Minimally invasive techniques have the potential to revolutionize the surgical management of pancreatic disease in the setting of benign and malignant processes. Both laparoscopic and robot-assisted approaches to pancreatic surgery have made open procedures, traditionally wrought with high morbidity, safer and more feasible. There still remains no consensus regarding the oncologic efficacy of minimally invasive surgery for pancreatic cancer even though median survival after open resection remains 16 to 19 months with 5-year overall survival averaging 22% to 25%. Recent advances in minimally invasive surgery seem to reduce the perioperative morbidity of pancreaticoduodenectomy for benign tumors while maintaining a perioperative safety profile equivalent to open approaches. The laparoscopic pancreaticoduodenectomy (LPD) was initially met with skepticism because of long operative times, but has now been established as safe and feasible when performed by select high-volume surgeons at experienced centers. The robotic pancreaticoduodenectomy (RPD), first performed in 2007, is now being increasingly used because of the perceived benefits of stereotactic vision, magnification, platform stability, and favorable ergonomics. Our institution is a strong advocate for minimally invasive approaches to pancreatic surgery and has demonstrated equivalent outcomes between open, laparoscopic, and robotic approaches and favors the robotic technique for benign and malignant processes of the pancreas. The urgency and potential benefits of minimally invasive surgery for patients with pancreatic cancer are highlighted by two recent observations: findings from the National Cancer Database show that 71.4% of patients with clinical stage 1 pancreatic adenocarcinoma currently choose no therapy for their disease and experience shorter survival compared with patients treated with pancreatectomy ( P <.001) suggesting a nihilism and fear about pancreatic surgery; and nearly half of patients undergoing open pancreaticoduodenectomy (OPD) have complications preventing administration of proven adjuvant chemotherapy. Wu and colleagues have demonstrated the impact of postoperative complications on the administration of adjuvant therapy following pancreaticoduodenectomy for adenocarcinoma. In their retrospective review of 1144 patients who underwent pancreaticoduodenectomy between 1995 and 2011, they noted an overall complication rate of 49.1%, and overall, 54% of the patients received adjuvant chemotherapy. Presence of a postoperative complication led to a definite delay in time to adjuvant therapy and reduced the likelihood of receiving multimodality therapy.
This article presents a review of two minimally invasive techniques for distal pancreatectomy (DP) and pancreaticoduodenectomy, focusing on metrics of technique, safety, morbidity, and oncologic outcomes and potential benefits.
Laparoscopic distal pancreatectomy
Indications for Minimally Invasive Distal Pancreatectomy
The minimally invasive approach to the DP (MIDP) is now considered by many to be the preferred method of resection for benign and malignant tumors of the distal pancreas. Several studies have been performed, collectively supporting that LDP and RDP can be performed with superior results to the open approach in patients with benign and malignant disease. Specifically, the minimally invasive approach results in shorter hospital stay, reduced blood loss (EBL), and decreased complication rates. Similar oncologic resections can be accomplished in terms of lymph node dissection and resection margins, although larger reports of long-term survival are still lacking. Current absolute contraindications to LDP or RDP include prohibitive medical comorbidities and poor patient functional status. Relative contraindications include locally advanced malignancies, vascular invasion, and prior major abdominal operations. Involvement of the celiac trunk is not an absolute contraindication to minimally invasive approach.
Technique of Laparoscopic Distal Pancreatectomy
The patient is placed in supine position, and the peritoneum is accessed either via a Veress needle approach or optical separator technique, which are both inserted in the left subcostal area to induce pneumoperitoneum. The second trocar is then inserted in the right supraumbilical region (12 mm). The remaining trocars are then placed in the left paraxiphoid region (5 mm), right subcostal area (5 mm), and left supraumbilical region (12 mm). Dissection begins with division of the gastrocolic ligament to enter the lesser sac. The splenic flexure of the colon is then mobilized inferiorly, and the anterior surface of the pancreas is inspected. The transverse mesocolon is then dissected off the inferior border of the pancreas, and the pancreas is dissected out of the retroperitoneum at the site of transection, creating a subpancreatic tunnel. Early identification of the splenic vessels and dissection of the vein and artery off the superoposterior aspect of the pancreas allows safer pancreatic transection. Once the vessels have been mobilized, the pancreatic parenchyma is divided using a linear stapler or harmonic scalpel, which is followed by division of the splenic vessels using a stapling device or clips. The spleen is then mobilized by sectioning the suspending ligaments, and the specimen is then placed in a large bag and brought through an access incision.
Outcomes of Laparoscopic Distal Pancreatectomy
Two methodologic problems complicate prospective studies of surgical technique for distal pancreatic cancer: only 20.8% of pancreatic ductal adenocarcinomas (PDA) arise in the distal pancreas; and the 1640 distal pancreatic resections performed annually in the United States are distributed among 1743 hospitals according to 1998 to 2003 data in the Nationwide Inpatient Sample, an average annual case volume of one per hospital. As a result, most comparative effectiveness research has been retrospective and confined to single institution data. Published outcomes after minimally invasive pancreatic resection demonstrate technical equivalence to open DP with reduced intraoperative blood loss and shortened hospital stay. There are only three published studies comparing open and laparoscopic DP (ODP and LDP) in patients with PDA. A single study of 23 patients undergoing LDP for PDC at nine centers has demonstrated median survival identical to open at 16 months by means of a 3:1 matched comparison with historical open DP control subjects.
Our institution performed a retrospective case series comparing clinicopathologic and long-term oncologic outcomes after MIDP and ODP for pancreatic ductal carcinoma in 62 consecutive patients at a single institution. Intention-to-treat analysis demonstrated no evidence for inferiority of MIDP compared with ODP in terms of postoperative outcomes or long-term survival. Another recent study by Nakamura and colleagues comparing LDP and ODP using propensity score-matching indicated the superiority of the laparoscopic approach over the open technique in regards to perioperative outcomes, including higher rate of preservation of spleen and splenic vessels ( P <.001), lower rates of intraoperative transfusion ( P = .020), clinical-grade pancreatic fistula ( P <.001), and morbidity ( P <.001). The laparoscopic cohort also had a shorter hospital stay ( P = .001), but a longer operative time ( P <.001).
Introduction
Minimally invasive techniques have the potential to revolutionize the surgical management of pancreatic disease in the setting of benign and malignant processes. Both laparoscopic and robot-assisted approaches to pancreatic surgery have made open procedures, traditionally wrought with high morbidity, safer and more feasible. There still remains no consensus regarding the oncologic efficacy of minimally invasive surgery for pancreatic cancer even though median survival after open resection remains 16 to 19 months with 5-year overall survival averaging 22% to 25%. Recent advances in minimally invasive surgery seem to reduce the perioperative morbidity of pancreaticoduodenectomy for benign tumors while maintaining a perioperative safety profile equivalent to open approaches. The laparoscopic pancreaticoduodenectomy (LPD) was initially met with skepticism because of long operative times, but has now been established as safe and feasible when performed by select high-volume surgeons at experienced centers. The robotic pancreaticoduodenectomy (RPD), first performed in 2007, is now being increasingly used because of the perceived benefits of stereotactic vision, magnification, platform stability, and favorable ergonomics. Our institution is a strong advocate for minimally invasive approaches to pancreatic surgery and has demonstrated equivalent outcomes between open, laparoscopic, and robotic approaches and favors the robotic technique for benign and malignant processes of the pancreas. The urgency and potential benefits of minimally invasive surgery for patients with pancreatic cancer are highlighted by two recent observations: findings from the National Cancer Database show that 71.4% of patients with clinical stage 1 pancreatic adenocarcinoma currently choose no therapy for their disease and experience shorter survival compared with patients treated with pancreatectomy ( P <.001) suggesting a nihilism and fear about pancreatic surgery; and nearly half of patients undergoing open pancreaticoduodenectomy (OPD) have complications preventing administration of proven adjuvant chemotherapy. Wu and colleagues have demonstrated the impact of postoperative complications on the administration of adjuvant therapy following pancreaticoduodenectomy for adenocarcinoma. In their retrospective review of 1144 patients who underwent pancreaticoduodenectomy between 1995 and 2011, they noted an overall complication rate of 49.1%, and overall, 54% of the patients received adjuvant chemotherapy. Presence of a postoperative complication led to a definite delay in time to adjuvant therapy and reduced the likelihood of receiving multimodality therapy.
This article presents a review of two minimally invasive techniques for distal pancreatectomy (DP) and pancreaticoduodenectomy, focusing on metrics of technique, safety, morbidity, and oncologic outcomes and potential benefits.
Laparoscopic distal pancreatectomy
Indications for Minimally Invasive Distal Pancreatectomy
The minimally invasive approach to the DP (MIDP) is now considered by many to be the preferred method of resection for benign and malignant tumors of the distal pancreas. Several studies have been performed, collectively supporting that LDP and RDP can be performed with superior results to the open approach in patients with benign and malignant disease. Specifically, the minimally invasive approach results in shorter hospital stay, reduced blood loss (EBL), and decreased complication rates. Similar oncologic resections can be accomplished in terms of lymph node dissection and resection margins, although larger reports of long-term survival are still lacking. Current absolute contraindications to LDP or RDP include prohibitive medical comorbidities and poor patient functional status. Relative contraindications include locally advanced malignancies, vascular invasion, and prior major abdominal operations. Involvement of the celiac trunk is not an absolute contraindication to minimally invasive approach.
Technique of Laparoscopic Distal Pancreatectomy
The patient is placed in supine position, and the peritoneum is accessed either via a Veress needle approach or optical separator technique, which are both inserted in the left subcostal area to induce pneumoperitoneum. The second trocar is then inserted in the right supraumbilical region (12 mm). The remaining trocars are then placed in the left paraxiphoid region (5 mm), right subcostal area (5 mm), and left supraumbilical region (12 mm). Dissection begins with division of the gastrocolic ligament to enter the lesser sac. The splenic flexure of the colon is then mobilized inferiorly, and the anterior surface of the pancreas is inspected. The transverse mesocolon is then dissected off the inferior border of the pancreas, and the pancreas is dissected out of the retroperitoneum at the site of transection, creating a subpancreatic tunnel. Early identification of the splenic vessels and dissection of the vein and artery off the superoposterior aspect of the pancreas allows safer pancreatic transection. Once the vessels have been mobilized, the pancreatic parenchyma is divided using a linear stapler or harmonic scalpel, which is followed by division of the splenic vessels using a stapling device or clips. The spleen is then mobilized by sectioning the suspending ligaments, and the specimen is then placed in a large bag and brought through an access incision.
Outcomes of Laparoscopic Distal Pancreatectomy
Two methodologic problems complicate prospective studies of surgical technique for distal pancreatic cancer: only 20.8% of pancreatic ductal adenocarcinomas (PDA) arise in the distal pancreas; and the 1640 distal pancreatic resections performed annually in the United States are distributed among 1743 hospitals according to 1998 to 2003 data in the Nationwide Inpatient Sample, an average annual case volume of one per hospital. As a result, most comparative effectiveness research has been retrospective and confined to single institution data. Published outcomes after minimally invasive pancreatic resection demonstrate technical equivalence to open DP with reduced intraoperative blood loss and shortened hospital stay. There are only three published studies comparing open and laparoscopic DP (ODP and LDP) in patients with PDA. A single study of 23 patients undergoing LDP for PDC at nine centers has demonstrated median survival identical to open at 16 months by means of a 3:1 matched comparison with historical open DP control subjects.
Our institution performed a retrospective case series comparing clinicopathologic and long-term oncologic outcomes after MIDP and ODP for pancreatic ductal carcinoma in 62 consecutive patients at a single institution. Intention-to-treat analysis demonstrated no evidence for inferiority of MIDP compared with ODP in terms of postoperative outcomes or long-term survival. Another recent study by Nakamura and colleagues comparing LDP and ODP using propensity score-matching indicated the superiority of the laparoscopic approach over the open technique in regards to perioperative outcomes, including higher rate of preservation of spleen and splenic vessels ( P <.001), lower rates of intraoperative transfusion ( P = .020), clinical-grade pancreatic fistula ( P <.001), and morbidity ( P <.001). The laparoscopic cohort also had a shorter hospital stay ( P = .001), but a longer operative time ( P <.001).
Robot-assisted distal pancreatectomy
Technique of Robot-Assisted Distal Pancreatectomy
MIDP has several advantages to its open counterpart with regards to blood loss, operative time, hospital length of stay, and complications particularly for benign disease. Furthermore, emerging data suggest that the robotic technique is a superior minimally invasive platform. Since 2009, our institution has performed hundreds of RDPs and has been able to demonstrate specific technical advantages provided by the robot-assisted approach, which are particularly important in the setting of pancreatic adenocarcinoma where adherence to oncologic principles are key to successful resections.
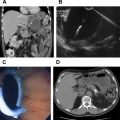
After the peritoneum is accessed in a similar fashion to that obtained in the laparoscopic approach, additional trocars are placed, and the robot is docked. Again, the lesser sac is entered by division of the gastrocolic ligament and the colonic splenic flexure is mobilized inferiorly. Focus is then paid on division of the pancreatic neck. Stereotactic vision and the robotic camera angle allow safe and quick isolation of the pancreatic neck over the superior mesenteric vein (SMV)–splenic vein confluence. The splenic artery is isolated at its takeoff from the celiac trunk, and divided with a vascular stapler ( Figs. 1 and 2 ).
A lymphadenectomy is then carried out starting from the left side of the superior mesenteric artery (SMA) laterally, taking the posterior pancreatic fascia en bloc, and a comprehensive celiac lymphadenectomy is completed. With large tumors involving the fourth portion of the duodenum or colon, the robot allows meticulous en bloc resections with reconstructions performed in a similar fashion to the open technique.
Outcomes of Robot-Assisted Distal Pancreatectomy
At the University of Pittsburgh, we compared our prospectively gathered data from the first 30 cases of RDP (performed between 2008 and 2011) with a historical control group of 94 laparoscopic cases (2004–2007, before the robot became available, and well after the group had established maturity with LDP). Patients undergoing RDP and LDP demonstrated equivalent age, gender, ethnicity, ASA (American Society of Anesthesiologists) score, and tumor size. No conversions to open surgery occurred in the RDP group compared with 16% in the LDP group ( P <.05). This was despite that more PDA were approached robotically than laparoscopically (43% vs 15%; P <.05). A more recent updated series of 100 RDPs by our institution demonstrated a persistently low conversion rate of (2%). This may be secondary to the ability of the surgeon at the console to control large vessels and manage unexpected bleeding via intracorporeal suturing more readily with the robot than using laparoscopy. In this experience, RDP outcomes were optimized after 40 cases.
Additionally, the robot platform has been shown to allow improved ability over laparoscopy to perform splenic preservation. In our institutional experience, we have demonstrated enhanced ability to preserve the spleen given increased maneuverability of the robotic arms to carefully dissect out the splenic vessels. In the difficult scenario where the splenic artery is embedded within the superior pancreatic parenchyma, robotic visualization, magnification, and improved dexterity of the instruments allow for rapid and efficient isolation and division of this vessel thereby avoiding a conversion.
The oncologic outcomes between the minimally invasive approach and the open technique for DP have been shown to be equivalent. Use of the robot seems to offer an increased advantage over laparoscopy, based on the authors’ experience. Our institutional experience demonstrated that despite a higher percentage of adenocarcinoma in the robotic group (43% vs 15%; P <.05) and a similar median tumor size of approximately 3 cm, RDP was associated with improved R0 resection rates (100% vs 64%; P <.05), and median lymph node count (19 vs 9; P <.01) when compared with laparoscopy. Although single institution outcomes may not be generalizable, we believe this observation reflects the ability to better recapitulate open oncologic principles with the robotic approach. A more comprehensive lymphadenectomy is completed given enhanced magnification and maneuverability of the robot.
Lastly, it has been shown that patients having undergone RDP as opposed to LDP or ODP have shorter hospital stays given decreased wound complications and increased rates of splenic preservation. As further experience with the robot-assisted approach is gained, additional advantages may be realized ( Table 1 ).