Minimally invasive adrenalectomy has become the gold standard for removal of benign adrenal tumors. The imaging characteristics, biochemical evaluation, and patient selection for laparoscopic transabdominal and posterior retroperitoneoscopic approaches are discussed with details of surgical technique for both procedures.
Key points
- •
Minimally invasive adrenalectomy is the preferred method for benign, accessible adrenal masses.
- •
Adrenal imaging and biochemical evaluation are essential for characterization of adrenal lesions.
- •
Patient selection for laparoscopic transabdominal and posterior retroperitoneoscopic adrenalectomy (PRA) should be based on anthropometric parameters and characterization of the adrenal mass.
- •
Minimally invasive adrenalectomy has been shown to be safe and efficacious for adrenal metastases; however, open adrenalectomy is recommended in suspected or confirmed primary adrenal malignancy for best oncologic outcome.
Introduction
With the increased use of abdominal imaging, adrenal neoplasms are being identified more frequently. Autopsy studies have evaluated the frequency of incidental adrenal masses and found that they are present in up to 6% of patients. There is an increasing prevalence with age, as adrenal masses are present in less than 1% of patients younger than 30 years and up to 7% of patients older than 70 years. Minimally invasive adrenalectomy through a laparoscopic transabdominal approach was first introduced in the early 1990s and has transformed the management of adrenal tumors. Since then, minimally invasive adrenalectomy has been shown to have less blood loss, earlier patient mobility, decreased length of stay, and faster return to regular activity. These advantages have led to increased frequency of surgery and evolution of indications for adrenalectomy.
Laparoscopic adrenalectomy has become the gold standard for removal of benign adrenal masses. This article discusses the management of incidentally discovered adrenal masses, indications for surgery, and surgical approaches, with a focus on the transabdominal and retroperitoneal methods.
Introduction
With the increased use of abdominal imaging, adrenal neoplasms are being identified more frequently. Autopsy studies have evaluated the frequency of incidental adrenal masses and found that they are present in up to 6% of patients. There is an increasing prevalence with age, as adrenal masses are present in less than 1% of patients younger than 30 years and up to 7% of patients older than 70 years. Minimally invasive adrenalectomy through a laparoscopic transabdominal approach was first introduced in the early 1990s and has transformed the management of adrenal tumors. Since then, minimally invasive adrenalectomy has been shown to have less blood loss, earlier patient mobility, decreased length of stay, and faster return to regular activity. These advantages have led to increased frequency of surgery and evolution of indications for adrenalectomy.
Laparoscopic adrenalectomy has become the gold standard for removal of benign adrenal masses. This article discusses the management of incidentally discovered adrenal masses, indications for surgery, and surgical approaches, with a focus on the transabdominal and retroperitoneal methods.
Patient evaluation and indications for adrenalectomy
The initial presentation of an adrenal mass is frequently an adrenal incidentaloma, defined as the identification of an unsuspected adrenal mass when imaging is performed for other indications. Adrenal incidentalomas have been reported in up to 5% of patients undergoing abdominal computed tomographic (CT) scans for other indications. Most adrenal masses are benign, although biochemical evaluation is recommended in all patients with adrenal incidentalomas. Indications for adrenalectomy include a hormonally active adrenal tumor or a suspected or confirmed malignancy. Adrenal malignancies may be either a primary adrenocortical carcinoma (ACC) or metastases from another primary cancer.
Imaging of Adrenal Masses
The increased frequency and technological advances in abdominal imaging have led to the increased identification of adrenal masses. Most often the imaging is obtained for other indications and is not optimized for evaluating the adrenal glands. However, some characteristics can be identified to broadly determine the nature of the lesion. Common characteristics attributed to benign adrenal neoplasms are size less than 4 cm, smooth contours with planes between organs intact, and a homogenous density; in contrast, malignant neoplasms are frequently greater than 6 cm in size, have irregular borders without clear planes, and are heterogeneous.
Benign adrenal adenomas contain high amounts of intracytoplasmic fat; approximately 70% of adrenal adenomas are rich in lipids. This high lipid content allows for the use of densitometry, measured as Hounsfield units (HU), to distinguish benign and malignant lesions on unenhanced CT. Initial reports used an HU threshold of less than 0 to indicate a benign lesion, with high specificity (100%) but poor sensitivity (47%). A meta-analysis of 10 studies that evaluated 495 adrenal lesions (272 benign and 223 malignant) by unenhanced CT found that an HU threshold of less than 10 had a sensitivity of 71% and specificity of 98% for the diagnosis of an adrenal adenoma, without further radiologic imaging. This method has become the standard for initial evaluation of incidental adrenal lesions without intravenous contrast.
Approximately 30% of adrenal masses may have an indeterminate HU (between 10 and 30), necessitating contrast-enhanced CT with delayed washouts. Because of neovascularization, malignancies tend to have increased contrast accumulation; as a result, intravenous contrast washes out from adenomas, both lipid rich and lipid poor, more quickly than from adrenal malignancies and pheochromocytomas. Contrast washout can be calculated in 2 ways: absolute percentage washout (APW) requires both noncontrast and contrast scans ([(enhanced HU−delayed HU)÷(enhanced HU−noncontrast HU)] × 100), whereas relative percentage washout (RPW) can be calculated based on an initial CT scan with contrast and delayed scans only ([(enhanced HU−delayed HU)÷enhanced HU] × 100). In adrenal protocol CT scans, initial noncontrast imaging is followed by contrast imaging; a 15-minute delayed scan is then performed. Adrenal masses with initial noncontrast HU less than 10 do not warrant contrast imaging. A 2002 prospective study of 166 adrenal masses imaged using this protocol found that an APW threshold of greater than 60% had a sensitivity of 86% and specificity of 92% for distinguishing lipid-poor adenomas from nonadenomas and an RPW threshold of 40% had a sensitivity of 82% and specificity of 92%. Other studies have confirmed these thresholds using 15-minute delayed imaging.
MRI may also be used for the characterization of adrenal lesions. Malignant adrenal lesions tend to contain more water and less fat than benign lesions and therefore have higher signal on T2 images, although pheochromocytomas may also have a similar appearance. When gadolinium contrast is used, adenomas appear more homogenous, whereas malignancies are heterogeneous. However, there is significant overlap in the characteristics of benign and malignant lesions; therefore, MRI may not definitively distinguish adenomas from malignant masses.
Adrenal lesions not well characterized by CT or MRI may benefit from radionuclide adrenal imaging with specific radiolabeled compounds that target elements of adrenal function and help characterize lesions. These radiotracers may include meta-iodobenzylguanidine (MIBG) for medullary tissue lesions and fludeoxyglucose F 18 ( 18 F FDG) for malignant tumors. MIBG imaging may identify both nonhypersecreting and hypersecreting adrenal medulla lesions with a positive predictive value of 83%. 18 F FDG-PET/CT has a sensitivity 99% to 100% and specificity of 94% to 100% for identifying malignant lesions.
Biochemical Evaluation of Adrenal Tumors
Initial evaluation of an adrenal mass should be to determine functional status. A thorough history and physical examination should be obtained, with specific questions related to eliciting symptoms of excess production of aldosterone, cortisol, or catecholamines ( Table 1 ). Evaluation should include assessment of other constitutional symptoms, including weight loss, history of cancer, and smoking history, as a primary ACC or adrenal metastases must also be considered in the differential diagnosis.
| Signs/Symptoms | Biochemical Evaluation | |
|---|---|---|
| Cushing’s syndrome |
|
|
| Pheochromocytoma |
|
|
| Primary aldosteronism |
| Plasma aldosterone/renin ratio |
Metastases to the adrenal gland
Isolated adrenal metastases are most commonly from a primary lung cancer, but other sites of primary malignancy include breast, melanoma, kidney, colon, stomach, and lymphoma. The benefits of surgery for metastatic disease are controversial, but studies have demonstrated improved survival in properly selected patients. Adrenal metastases should be suspected in patients with known history of cancer who are found to have an adrenal mass on initial workup or routine surveillance of the primary malignancy. Evaluation should include comparison to prior imaging and biochemical evaluation for a functional adrenal tumor.
According to the American Association of Clinical Endocrinologists (AACE) and American Association of Endocrine Surgeons (AAES) guidelines on the management of adrenal incidentaloma, a thorough evaluation for locoregional recurrence and other metastatic sites is required if an adrenal metastasis is suspected. Adrenalectomy can be considered to improve disease-free survival in appropriately selected patients without significant other sites of disease and good performance status. Given the safety of minimally invasive surgery, it should be considered as a first-line approach for isolated adrenal metastases.
Several studies have examined the outcomes of patients undergoing adrenalectomy for adrenal metastases. A retrospective review from the Mayo clinic matched 166 patients who underwent adrenalectomy for adrenal metastases to Surveillance, Epidemiology, and End Results (SEER) data of similar patients who did not undergo adrenalectomy. Patients with primary soft-tissue, kidney, lung, and pancreatic tumors were found to have better overall survival at 3 years: sarcoma (86% vs 30%), kidney (72% vs 27%), lung (52% vs 25%), and pancreas (45% vs 12%). In this study, risk factors for death included shorter interval from primary diagnosis to adrenalectomy, other distant sites of disease, surgery for palliation, and persistent disease. A retrospective European multicenter review identified 317 patients who underwent adrenalectomy for adrenal metastases; the most common primary tumor was non–small cell lung cancer (47%), followed by colorectal (14%) and renal (12%) cancers. Laparoscopic adrenalectomy was performed in 146 (46%) patients. Median overall survival was 29 months, with 3- and 5-year survival of 42% and 35%, respectively. Patients who underwent laparoscopic adrenalectomy had improved survival (hazard ratio, 0.65; 95% confidence interval, 0.47–0.90).
Laparoscopic adrenalectomy has been shown to be safe and oncologically appropriate for adrenal metastases. A retrospective review of 92 patients undergoing adrenalectomy (94 adrenalectomies: 63 open and 31 laparoscopic) for isolated adrenal metastases found a median overall survival of 30 months and 5-year estimated survival of 31%. In comparing laparoscopic with open surgery, there was no difference in local recurrence, margin status, disease-free interval, or overall survival. Laparoscopic adrenalectomy was associated with decreased blood loss (106 vs 749 mL; P <.0001), operative time (175 vs 208 minutes; P = .04), length of stay (2.8 vs 8.0 days; P <.0001), and complication rates (4% vs 34%; P <.0001). A more recent study of 90 patients who underwent adrenalectomy for adrenal metastases found that laparoscopic adrenalectomy, performed in 55 (61%) patients, was associated with smaller tumor size and reduced blood loss, operative time, and length of stay. Median overall survival was 2.46 years (range, <1 month to 15 years) and 5-year survival was 38%, with no difference in overall survival between laparoscopic and open adrenalectomy.
Preoperative preparation
Preoperative preparation depends on the functional status of the mass. For patients with a pheochromocytoma, preoperative α-adrenergic blockade is necessary to decrease risk of perioperative cardiovascular complications. Medication should be started 7 to 14 days before planned surgery for adequate time to correct blood pressure and heart rate. β-Adrenergic blockade should be initiated for reflexive tachycardia only after appropriate α-blockade. Patients should also be encouraged to increase sodium and fluid intake to counteract the catecholamine-induced volume contraction. It is important that preoperative consultation and discussion is arranged with the anesthesia team so they are prepared to manage hemodynamic changes during the procedure. For patients with cortisol production, patients may require perioperative steroids with outpatient follow-up for monitoring and tapering of steroids.
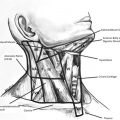
Approaches to surgery: laparoscopic transabdominal versus posterior retroperitoneoscopic adrenalectomy
The laparoscopic transabdominal and posterior retroperitoneoscopic approaches to adrenalectomy both afford specific advantages and disadvantages ( Table 2 ). Proper patient selection is essential, with minimally invasive adrenalectomy not recommended for suspected or known ACC. The transabdominal approach was initially widely adopted as the view is more familiar to most surgeons and allows for combination with other abdominal procedures. This approach requires mobilization of the colon, spleen, and pancreas (left) and liver (right), and intra-abdominal adhesions from prior surgical procedures may be present. Retrospective review of laparoscopic transabdominal adrenalectomy in patients with prior abdominal surgery has shown it to be safe, without significantly increasing operative time, complication rates, conversion to open surgery, or length of stay.
| Advantages | Disadvantages/Contraindications | |
|---|---|---|
| Retroperitoneoscopic |
|
|
| Laparoscopic transabdominal |
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree